Non-Contiguous Finished Genome Sequence and Description of Bartonella Saheliensis Sp. Nov. from the Blood of Gerbilliscus Gambia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bartonella Apis Sp. Nov., a Honey Bee Gut Symbiont of the Class Alphaproteobacteria
Serveur Academique´ Lausannois SERVAL serval.unil.ch Author Manuscript Faculty of Biology and Medicine Publication This paper has been peer-reviewed but does not include the final publisher proof-corrections or journal pagination. Published in final edited form as: Title: Bartonella apis sp. nov., a honey bee gut symbiont of the class Alphaproteobacteria. Authors: Keˇsnerov´aL, Moritz R, Engel P Journal: International journal of systematic and evolutionary microbiology Year: 2016 Jan Issue: 66 Volume: 1 Pages: 414-21 DOI: 10.1099/ijsem.0.000736 In the absence of a copyright statement, users should assume that standard copyright protection applies, unless the article contains an explicit statement to the contrary. In case of doubt, contact the journal publisher to verify the copyright status of an article. 1 Bartonella apis sp. nov., a honey bee gut symbiont of the 2 class Alphaproteobacteria 3 4 Lucie Kešnerová, Roxane Moritz, Philipp Engel* 5 6 Department of Fundamental Microbiology, University of Lausanne, CH-1015 7 Lausanne, Switzerland 8 9 Running title: Description of a bee gut symbiont 10 11 *Correspondence: 12 Prof. Philipp Engel 13 Department of Fundamental Microbiology 14 University of Lausanne, CH-1015 Lausanne, Switzerland 15 Tel.: +41 (0)21 692 56 12 16 e-mail: [email protected] 17 18 Category: New Taxa – Proteobacteria 19 Keywords: Apis mellifera; insect; Bartonella; gut microbiota; Alpha-1 20 21 Sequence deposition: The 16S rRNA gene sequences and protein-coding gene 22 sequences of the bacterial strains PEB0122T, PEB0149, PEB0150, BBC0104, and 23 BBC0108 from Apis mellifera, and the uncultured Rhizobiales bacterium from 24 Herpagnathos saltator are deposited in GenBank with accession numbers KP987849 25 – KP987886 and KT315729 – KT315734. -

View Tickborne Diseases Sample Report
1360 Bayport Ave, Ste B. San Carlos, CA 94070 1(866) 364-0963 | [email protected] | www. vibrant-wellness.com PATIENT PROVIDER NAME: DEMO REPORT GENDER: Male PRACTICE NAME: Vibrant IT4 Practice DATE OF BIRTH: 04/14/1998 AGE: 22 PROVIDER NAME: Demo Client, DDD (999994) ADDRESS: TEST STREET, TEST CITY, KY- 42437. ACCESSION ID: 2009220006 PHLEBOTOMIST: 607 SPECIMEN COLLECTION TIME: 09-21-2020 11:14 SPECIMEN RECEIVED TIME: 09-22-2020 05:14 FINAL REPORT TIME: 09-25-2020 15:56 FASTING: FASTING Your Vibrant Wellness TickBorne 2.0 panel results are enclosed. These results are intended to aid in the diagnosis of tickborne diseases by your healthcare provider. The Vibrant Tickborne Diseases panel tests for IgG and IgM antibodies for Borreliosis/Lyme disease as well as co-infection(s) and opportunistic infections with other tick-borne illnesses along with detection of DNA of the species causing these infections. The Vibrant Immunochip test is a semiquantitative assay that detects IgG and IgM antibodies in human serum. The PCR Test is a real-time PCR Assay designed for qualitative detection of infectious group- specific DNA in clinical samples. Interpretation of Report: The test results of antibody levels to the individual antigens are calculated by comparing the average intensity of the individual antibody to that of a reference population and cut-off chosen for each protein. Reference ranges have been established using a well characterized set of more than 300 serum samples and antibodies to specific bacteria tested. The results are displayed as In Control, Moderate, or High Risk.for each antigen tested. -

Genetic Diversity of Bartonella Species in Small Mammals in the Qaidam
www.nature.com/scientificreports OPEN Genetic diversity of Bartonella species in small mammals in the Qaidam Basin, western China Huaxiang Rao1, Shoujiang Li3, Liang Lu4, Rong Wang3, Xiuping Song4, Kai Sun5, Yan Shi3, Dongmei Li4* & Juan Yu2* Investigation of the prevalence and diversity of Bartonella infections in small mammals in the Qaidam Basin, western China, could provide a scientifc basis for the control and prevention of Bartonella infections in humans. Accordingly, in this study, small mammals were captured using snap traps in Wulan County and Ge’ermu City, Qaidam Basin, China. Spleen and brain tissues were collected and cultured to isolate Bartonella strains. The suspected positive colonies were detected with polymerase chain reaction amplifcation and sequencing of gltA, ftsZ, RNA polymerase beta subunit (rpoB) and ribC genes. Among 101 small mammals, 39 were positive for Bartonella, with the infection rate of 38.61%. The infection rate in diferent tissues (spleens and brains) (χ2 = 0.112, P = 0.738) and gender (χ2 = 1.927, P = 0.165) of small mammals did not have statistical diference, but that in diferent habitats had statistical diference (χ2 = 10.361, P = 0.016). Through genetic evolution analysis, 40 Bartonella strains were identifed (two diferent Bartonella species were detected in one small mammal), including B. grahamii (30), B. jaculi (3), B. krasnovii (3) and Candidatus B. gerbillinarum (4), which showed rodent-specifc characteristics. B. grahamii was the dominant epidemic strain (accounted for 75.0%). Furthermore, phylogenetic analysis showed that B. grahamii in the Qaidam Basin, might be close to the strains isolated from Japan and China. -

Abstract Pultorak, Elizabeth Lauren
ABSTRACT PULTORAK, ELIZABETH LAUREN. The Epidemiology of Lyme Disease and Bartonellosis in Humans and Animals. (Under the direction of Edward B. Breitschwerdt). The expansion of vector borne diseases in humans, a variety of mammalian hosts, and arthropod vectors draws attention to the need for enhanced diagnostic techniques for documenting infection in hosts, effective vector control, and treatment of individuals with associated diseases. Through improved diagnosis of vector-borne disease in both humans and animals, epidemiological studies to elucidate clinical associations or spatio-temporal relationships can be assessed. Veterinarians, through the use of the C6 peptide in the SNAP DX test kit, may be able to evaluate the changing epidemiology of borreliosis through their canine population. We developed a survey to evaluate the practices and perceptions of veterinarians in North Carolina regarding borreliosis in dogs across different geographic regions of the state. We found that veterinarians’ perception of the risk of borreliosis in North Carolina was consistent with recent scientific reports pertaining to geographic expansion of borreliosis in the state. Veterinarians should promote routine screening of dogs for Borrelia burgdorferi exposure as a simple, inexpensive form of surveillance in this transitional geographic region. We next conducted two separate studies to evaluate Bartonella spp. bacteremia or presence of antibodies against B. henselae, B. koehlerae, or B. vinsonii subsp. berkhoffii in 296 patients examined by a rheumatologist and 192 patients with animal exposure (100%) and recent animal bites and scratches (88.0%). Among 296 patients examined by a rheumatologist, prevalence of antibodies (185 [62%]) and Bartonella spp. bacteremia (122 [41.1%]) was high. -

Bartonella Henselae • Fleas and Black-Legged Ticks (Also Called Deer Ticks) of the Genus Ixodes May Serve As Vectors, but This Has Not Disease Agent: Been Proven
APPENDIX 2 Bartonella henselae • Fleas and black-legged ticks (also called deer ticks) of the genus Ixodes may serve as vectors, but this has not Disease Agent: been proven. • Bartonella henselae Blood Phase: Disease Agent Characteristics: • Agent found in endothelial cells and associated with RBCs in symptomatic cases • Gram-negative bacillus or coccobacillus, aerobic, • Occult bacteremia sometimes occurs in the absence nonmotile, nonspore-forming, facultatively intracel- of specific antibodies. lular bacterium • Order: Rhizobiales; Family: Bartonellaceae Survival/Persistence in Blood Products: • Size: 0.3-0.6 ¥ 0.3-1.0 mm • Nucleic acid: Approximately 1900 kb of DNA • A spiking study suggests that B. henselae added to RBCs can be recovered on solid media through 35 Disease Name: days of storage at 4°C. • Cat scratch disease • Cat scratch fever Transmission by Blood Transfusion: • Bacillary angiomatosis • Theoretical • Bacillary peliosis Cases/Frequency in Population: Priority Level: • 22,000 cases per year estimated in the US • Scientific/Epidemiologic evidence regarding blood • 2-6% in US blood donors safety: Theoretical • Cumulative seroprevalence of 7.1% to B. henselae and • Public perception and/or regulatory concern regard- B. quintana in US veterinary professionals ing blood safety: Absent • Public concern regarding disease agent: Very low Incubation Period: Background: • 3-10 days to appearance of papule at inoculation site; regional adenopathy may follow after a few weeks • In 1909,ALBartondescribed organisms that adhered to RBCs. Likelihood of Clinical Disease: • The name Bartonella bacilliformis was used for the • Relatively benign and self-limiting, lasting 6-12 weeks only member of the group identified before 1993. in the absence of antibiotic therapy • Several other species of Bartonella are known to infect humans, but at present, B. -

Detection and Partial Molecular Characterization of Rickettsia and Bartonella from Southern African Bat Species
Detection and partial molecular characterization of Rickettsia and Bartonella from southern African bat species by Tjale Mabotse Augustine (29685690) Submitted in partial fulfillment of the requirements for the degree MAGISTER SCIENTIAE (MICROBIOLOGY) in the Department of Microbiology and Plant Pathology Faculty of Natural and Agricultural Sciences University of Pretoria Pretoria, South Africa Supervisor: Dr Wanda Markotter Co-supervisors: Prof Louis H. Nel Dr Jacqueline Weyer May, 2012 I declare that the thesis, which I hereby submit for the degree MSc (Microbiology) at the University of Pretoria, South Africa, is my own work and has not been submitted by me for a degree at another university ________________________________ Tjale Mabotse Augustine i Acknowledgements I would like send my sincere gratitude to the following people: Dr Wanda Markotter (University of Pretoria), Dr Jacqueline Weyer (National Institute for Communicable Diseases-National Health Laboratory Service) and Prof Louis H Nel (University of Pretoria) for their supervision and guidance during the project. Dr Jacqueline Weyer (Centre for Zoonotic and Emerging diseases (Previously Special Pathogens Unit), National Institute for Communicable Diseases (National Heath Laboratory Service), for providing the positive control DNA for Rickettsia and Dr Jenny Rossouw (Special Bacterial Pathogens Reference Unit, National Institute for Communicable Diseases-National Health Laboratory Service), for providing the positive control DNA for Bartonella. Dr Teresa Kearney (Ditsong Museum of Natural Science), Gauteng and Northern Region Bat Interest Group, Kwa-Zulu Natal Bat Interest Group, Prof Ara Monadjem (University of Swaziland), Werner Marias (University of Johannesburg), Dr Francois du Rand (University of Johannesburg) and Prof David Jacobs (University of Cape Town) for collection of blood samples. -

Bartonella Henselae Detected in Malignant Melanoma, a Preliminary Study
pathogens Article Bartonella henselae Detected in Malignant Melanoma, a Preliminary Study Marna E. Ericson 1, Edward B. Breitschwerdt 2 , Paul Reicherter 3, Cole Maxwell 4, Ricardo G. Maggi 2, Richard G. Melvin 5 , Azar H. Maluki 4,6 , Julie M. Bradley 2, Jennifer C. Miller 7, Glenn E. Simmons, Jr. 5 , Jamie Dencklau 4, Keaton Joppru 5, Jack Peterson 4, Will Bae 4, Janet Scanlon 4 and Lynne T. Bemis 5,* 1 T Lab Inc., 910 Clopper Road, Suite 220S, Gaithersburg, MD 20878, USA; [email protected] 2 Intracellular Pathogens Research Laboratory, Comparative Medicine Institute, College of Veterinary Medicine, North Carolina State University, Raleigh, NC 27607, USA; [email protected] (E.B.B.); [email protected] (R.G.M.); [email protected] (J.M.B.) 3 Dermatology Clinic, Truman Medical Center, University of Missouri, Kansas City, MO 64108, USA; [email protected] 4 Department of Dermatology, University of Minnesota, Minneapolis, MN 55455, USA; [email protected] (C.M.); [email protected] (A.H.M.); [email protected] (J.D.); [email protected] (J.P.); [email protected] (W.B.); [email protected] (J.S.) 5 Department of Biomedical Sciences, Duluth Campus, Medical School, University of Minnesota, Duluth, MN 55812, USA; [email protected] (R.G.M.); [email protected] (G.E.S.J.); [email protected] (K.J.) 6 Department of Dermatology, College of Medicine, University of Kufa, Kufa 54003, Iraq 7 Galaxy Diagnostics Inc., Research Triangle Park, NC 27709, USA; [email protected] Citation: Ericson, M.E.; * Correspondence: [email protected]; Tel.: +1-720-560-0278; Fax: +1-218-726-7906 Breitschwerdt, E.B.; Reicherter, P.; Maxwell, C.; Maggi, R.G.; Melvin, Abstract: Bartonella bacilliformis (B. -

Human Case of Bartonella Alsatica Lymphadenitis
LETTERS (6). The sequence is distinct from a DOI: 10.3201/eid1412.080944 Human Case of small number of sequences derived from rabies viruses in Vietnam, which References Bartonella alsatica suggests that China is a stronger can- Lymphadenitis 1. Smith JS, Fishbein DB, Rupprecht CE, didate for the source of the virus than Clark K. Unexplained rabies in three To the Editor: Lymph node en- her native country. immigrants in the United States: a vi- Although the case history could rologic investigation. N Engl J Med. largement is a common medical prob- not provide evidence for interaction 1991;324:205–11. lem that is usually caused by bacterial, 2. Grattan-Smith PJ, O’Regan WJ, Ellis PS, with a dog while her family was in viral, fungal, or protozoal agents (1). O’Flaherty SJ, McIntyre PB, Barnes CJ. A Malignancies or lymphoproliferative Hong Kong Special Administrative second Australian case, with a long incuba- Region, rabies was endemic within tion period. Med J Aust. 1992;156:651–4. diseases are often found, especially in the colony at the time that the pa- 3. McColl KA, Gould AR, Selleck PW, elderly patients (1). Bartonella hense- Hooper PT, Westbury HA, Smith JS. tient’s family was resident. From 1980 lae, the main causative agent of cat- Polymerase chain reaction and other labo- scratch disease (CSD), appears to be through 1984, 5 human cases were re- ratory techniques in the diagnosis of long corded (9). Only 2 case-patients had incubation rabies in Australia. Aust Vet the most common organism respon- clear evidence of a dog bite; histories J. -

Bartonella Spp. Infection Rate and B. Grahamii in Ticks
LETTERS 8. Reif KE, Macaluso KR. Ecology which is common in Europe, may nlm.nih.gov/Blast.cgi) comparison to of Rickettsia felis: a review. J Med also transmit zoonotic Bartonella spp. published sequences. Entomol. 2009;46:723–36. http://dx.doi. org/10.1603/033.046.0402 Evidence of possible tick transmission On the basis of the amplicon- 9. Reif KE, Stout RW, Henry GC, Foil LD, of bartonellae to humans under natural specifi c melting temperature and DNA Macaluso KR. Prevalence and infection conditions was provided by Eskow et bands representing the specifi c size load dynamics of Rickettsia felis in al. (3) and Angelakis et al. (4), who of 249-bp after gel electrophoresis, actively feeding cat fl eas. PLoS ONE. 2008;3:e2805. http://dx.doi.org/10.1371/ identifi ed Bartonella spp. in tissue results of qPCR showed 100 (4.76%) journal.pone.0002805 samples of patients who were recently infected I. ricinus ticks (Table). 10. Mitchell CJ. The role of Aedes albopictus bitten by ticks. We determined the Positive results did not vary by as an arbovirus vector. Parassitologia. prevalence of Bartonella spp. in developmental tick stages; 4.84% 1995;37:109–13. questing I. ricinus ticks in the city (18/372) adult ticks (5.08% [9/177] Address for correspondence: Didier Raoult, of Hanover, Germany, which is female and 4.62% [9/195] male), URMITE, UMR CNRS 7278, IRD 198, nicknamed The Green Metropolis and 4.71% (80/1,698) nymphs, and 6.67% INSERM 1095, Faculté de Médecine, 27 Bd was selected the German Capital of (2/30) larvae were infected (Table). -

Tick-Borne Pathogens in Removed Ticks Veneto, Northeastern Italy
Tick-borne pathogens in removed ticks Veneto, northeastern Italy: A cross-sectional investigation Anna Beltrame, Maureen Laroche, Monica Degani, Francesca Perandin, Zeno Bisoffi, Didier Raoult, Philippe Parola To cite this version: Anna Beltrame, Maureen Laroche, Monica Degani, Francesca Perandin, Zeno Bisoffi, et al.. Tick- borne pathogens in removed ticks Veneto, northeastern Italy: A cross-sectional investigation. Travel Medicine and Infectious Disease, Elsevier, 2018, 26, pp.58-61. 10.1016/j.tmaid.2018.08.008. hal- 01970220 HAL Id: hal-01970220 https://hal.archives-ouvertes.fr/hal-01970220 Submitted on 10 Apr 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Travel Medicine and Infectious Disease 26 (2018) 58–61 Contents lists available at ScienceDirect Travel Medicine and Infectious Disease journal homepage: www.elsevier.com/locate/tmaid Tick-borne pathogens in removed ticks Veneto, northeastern Italy: A cross- sectional investigation T ∗ Anna Beltramea, , Maureen Larocheb, Monica Degania, Francesca Perandina, Zeno Bisoffia, Didier Raoultc, Philippe Parolab a Centre for Tropical Diseases, IRCCS Sacro Cuore Don Calabria Hospital, Via Sempreboni 5, 37024, Negrar, Italy b Aix Marseille Univ, AP-HM, SSA, VITROME, IHU-Méditerranée Infection, 19-21 Bd Jean Moulin, 13005, Marseille, France c Aix Marseille Univ, AP-HM, MEPHI, IHU-Méditerranée Infection, 19-21 Bd Jean Moulin, 13005, Marseille, France ARTICLE INFO ABSTRACT Keywords: Background: In Italy, the incidence of tick-borne diseases in humans is underestimated, as they are not ob- Tick-borne diseases ligatorily notifiable. -

Endocarditis Due to Bartonella Quintana, the Etiological Agent of Trench Fever
PRACTICE | CASES CPD VULNERABLE POPULATIONS Endocarditis due to Bartonella quintana, the etiological agent of trench fever Carl Boodman MD, Terence Wuerz MD MSc (Epi), Philippe Lagacé-Wiens MD n Cite as: CMAJ 2020 December 7;192:E1723-6. doi: 10.1503/cmaj.201170 CMAJ Podcasts: author interview at www.cmaj.ca/lookup/doi/10.1503/cmaj.201170/tab-related-content 48-year-old man presented to the emergency depart- ment with a 2-day history of pleuritic chest pain and KEY POINTS shortness of breath. His medical history included HIV • Bartonella quintana, the causal agent of trench fever, is infection,A diagnosed 14 years earlier in the context of intraven- transmitted by body lice (Pediculus humanus var. corporis). ous drug use. Three months previously, he had an undetectable • Although B. quintana is notorious for causing disease in the First viral load and a CD4 count of 94 cells/mm3 (normal range: 500– World War, outbreaks of trench fever have recently occurred in 1400 cells/mm3) or 0.09 (normal range 0.50–1.40) × 109/L. The urban populations experiencing homelessness. patient adhered to his prescribed antiretroviral regimen (darunavir, • B. quintana causes culture-negative endocarditis and may be ritonavir and abacavir-lamivudine) and prophylaxis against oppor- fatal without antimicrobial and surgical treatment, despite mild tunistic infections (valacyclovir, trimethoprim-sulfamethoxazole symptomatology during chronic bacteremia. Consultation with infectious disease specialists is encouraged. and fluconazole). In addition, the patient had a congenital soli- Because B. quintana evades identification in routine blood tary kidney with normal baseline renal function, alcohol expos- • cultures, diagnosis of B. -
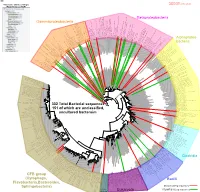
Bacteria Clostridia Bacilli Eukaryota CFB Group
AM935842.1.1361 uncultured Burkholderiales bacterium Class Betaproteobacteria AY283260.1.1552 Alcaligenes sp. PCNB−2 Class Betaproteobacteria AM934953.1.1374 uncultured Burkholderiales bacterium Class Betaproteobacteria AJ581593.1.1460 uncultured betaAM936569.1.1351 proteobacterium uncultured Class Betaproteobacteria Derxia sp. Class Betaproteobacteria AJ581621.1.1418 uncultured beta proteobacterium Class Betaproteobacteria DQ248272.1.1498 uncultured soil bacterium soil uncultured DQ248272.1.1498 DQ248235.1.1498 uncultured soil bacterium RS49 DQ248270.1.1496 uncultured soil bacterium DQ256489.1.1211 Variovorax paradoxus Class Betaproteobacteria Class paradoxus Variovorax DQ256489.1.1211 AF523053.1.1486 uncultured Comamonadaceae bacterium Class Betaproteobacteria AY706442.1.1396 uncultured bacterium uncultured AY706442.1.1396 AJ536763.1.1422 uncultured bacterium CS000359.1.1530 Variovorax paradoxus Class Betaproteobacteria Class paradoxus Variovorax CS000359.1.1530 AY168733.1.1411 uncultured bacterium AJ009470.1.1526 uncultured bacterium SJA−62 Class Betaproteobacteria Class SJA−62 bacterium uncultured AJ009470.1.1526 AY212561.1.1433 uncultured bacterium D16212.1.1457 Rhodoferax fermentans Class Betaproteobacteria Class fermentans Rhodoferax D16212.1.1457 AY957894.1.1546 uncultured bacterium AJ581620.1.1452 uncultured beta proteobacterium Class Betaproteobacteria RS76 AY625146.1.1498 uncultured bacterium RS65 DQ316832.1.1269 uncultured beta proteobacterium Class Betaproteobacteria DQ404909.1.1513 uncultured bacterium uncultured DQ404909.1.1513 AB021341.1.1466 bacterium rM6 AJ487020.1.1500 uncultured bacterium uncultured AJ487020.1.1500 RS7 RS86RC AF364862.1.1425 bacterium BA128 Class Betaproteobacteria AY957931.1.1529 uncultured bacterium uncultured AY957931.1.1529 CP000884.723807.725332 Delftia acidovorans SPH−1 Class Betaproteobacteria AY957923.1.1520 uncultured bacterium uncultured AY957923.1.1520 RS18 AY957918.1.1527 uncultured bacterium uncultured AY957918.1.1527 AY945883.1.1500 uncultured bacterium AF526940.1.1489 uncultured Ralstonia sp.