Facilitator Guide Ch 10: Medication Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -
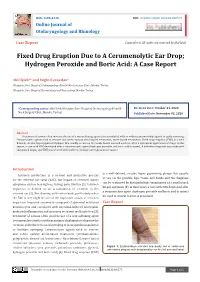
Fixed Drug Eruption Due to a Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: a Case Report
ISSN: 2688-8238 DOI: 10.33552/OJOR.2020.04.000577 Online Journal of Otolaryngology and Rhinology Case Report Copyright © All rights are reserved by Akif İşlek Fixed Drug Eruption Due to A Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: A Case Report Akif İşlek1* and Engin Karaaslan2 1Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey 2Nusaybin State Hospital, Dermatology and Venereology, Mardin, Turkey *Corresponding author: Received Date: October 24, 2020 Published Date: November 03, 2020 Akif İşlek, Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey. Abstract Treatment of earwax often involves the use of a wax softening agent (cerumenolytic) with or without antimicrobial agents to easily removing. Cerumenolytic agents used to remove and soften earwax areoil-based treatments, water-based treatments. Fixed drug eruption (FDE) is a well- defined, circular, hyperpigmented plaque that usually occurs on the trunk, hands mucosal surfaces, after a systemical application of drugs. In this report, a case with FDE developed after a cerumenolytic agent (hydrogen peroxide and boric acid in water). A definitive diagnosis was made with skin punch biopsy and FDE was treated with oral levocetirizine and topical mometasone. Introduction is a well-defined, circular, hyper pigmenting plaque that usually Cerumen production is a normal and protective process occurs on the genitals, lips, trunk, and hands and the diagnosis for the external ear canal (EAC), but impact of cerumen causes can be confirmed by histopathologic examination of a small punch symptoms such as hearing loss, itching, pain, tinnitus [1]. Cerumen biopsy specimen [5]. In this report, a case with FDE developed after impaction is defined as an accumulation of cerumen in the a cerumenolytic agent (hydrogen peroxide and boric acid in water) external ear [2]. -

Common Ear, Nose & Throat Problems
Common Ear, Nose & Throat Problems The information provided in this presentation is not intended to guide treatment or aid in making a diagnosis. Always consult a physician or nurse practitioner. Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Normal Larynx Normal larynx in a 44 yr old non-smoker Go to http://www.entusa.com/normal_larynx.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Acute Laryngitis This video shows the function of the larynx in a 24 yr old patient with acute laryngitis. Talking was painful and she only talked in a faint whisper. Go to http://www.entusa.com/laryngitis.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Paralysis This video shows the function of a larynx with a paralyzed left true vocal cord. The patient has lung cancer. She has a poorly compensated breathy voice which is difficult to understand. This patient had a 55 pack year history of smoking. Go to http://www.entusa.com/vocal_cord_paralysis_2.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Polyp This video shows the function of a larynx with a vocal cord polyp on the right true vocal cord. This patient smoked one pack a day for 30 years. Go to http://www.entusa.com/larynx_polyp-9.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Laryngeal Cancer This video shows the function of a larynx with a large T1b Cancer on both true vocal cords and anterior commissure in 72 yr old male with a 150 pack year history of smoking. -
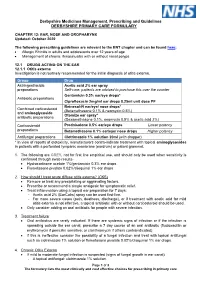
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

10/15-Hour Medication Test Answers
Appendix 10/15-Hour Medication Test Answers Name _________________________________ Facility _________________________________ Part 1: Match the term or phrase on the right with the abbreviation or term on the left by placing the correct letter on the appropriate line. _____ 1. PRN (p) a. milligram _____ 2. ac (e) b. at bedtime _____ 3. stat (j) c. Medication Administration Record _____ 4. SL (k) d. over the counter _____ 5. MAR (c) e. before meals _____ 6. mg (a) f. tablespoonful _____ 7. pc (m) g. placed and affixed to the skin _____ 8. OTC (d) h. teaspoonful _____ 9. Subcutaneous (r) i. milliliter _____ 10. po (n) j. immediately _____ 11. qhs (b) k. sublingual _____ 12. tbsp (f) l. placed under the tongue _____ 13. transdermal (g) m. after meals _____ 14. ml (i) n. by mouth _____ 15. gm (o) o. gram _____ 16. QOD (q) p. as needed _____ 17. tsp (h) q. every other day _____ 18. sublingual (l) r. inject into the fat with a syringe Medication Administration – March 2021 10/15-Hour Training Course for Adult Care Homes 4 Appendix 10/15-Hour Medication Test Answers – Continued Part 2: Fill in the blank with the appropriate word or term. You may choose to use the word bank below. 19. A heart tablet taken by mouth and swallowed is an example of a medication taken by the oral route. 20. A medication that is inserted into the rectum is given using the rectal route. 21. A topical medication is applied directly to the skin surface. -

GENTAMICIN Eye/Ear Drops 0.3% W/V Gentamicin Sulphate Please
GENTAMICIN Eye/Ear Drops 0.3% w/v Gentamicin Sulphate Please read this leaflet carefully before you start using this medicine. Keep this leaflet. You may need to read it again. If you have further questions, please ask your doctor or pharmacist. This medicine has been prescribed for you personally and you should not pass it on to others. It may harm them, even if their symptoms are the same as yours. If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist. The medicine will be called Gentamicin in this leaflet. In this leaflet: 1. What Gentamicin is and what it is used for 2. Before you use Gentamicin 3. How to use Gentamicin 4. Possible side effects 5. How to store Gentamicin 6. Further information 1. WHAT GENTAMICIN IS AND WHAT IT IS USED FOR Gentamicin eye/ear Drops are a sterile, preserved, aqueous solution used as eye/ear drops. The active ingredient Gentamicin is an antibiotic used to kill bacteria which cause infection. It is used for the management of eye & ear infection. 2. BEFORE YOU USE GENTAMICIN Do not use if you are allergic to Gentamicin, any of the ingredients, or any other aminoglycoside antibiotics if you have a perforated ear drum if you suffer from myasthenia gravis and related conditions Before you use Gentamicin: Take special care with Gentamicin Avoid prolonged use The drops must not be used in the ear if the ear drum is damaged in any way. -

Therapeutic Class Overview Otic Fluoroquinolones
Therapeutic Class Overview Otic Fluoroquinolones Therapeutic Class • Overview/Summary: This review will focus on the otic fluoroquinolone antibiotics.1-4 Topical corticosteroids help to aid in the resolution of the inflammatory response accompanying bacterial infections.3,4 Fluoroquinolones are broad-spectrum antimicrobial agents that directly inhibit bacterial deoxyribonucleic acid (DNA) synthesis by blocking the actions of DNA gyrase and topoisomerase IV, which leads to bacterial cell death.5 The otic antibacterials are approved for the treatment of otitis externa and otitis media. Otitis externa (also known as swimmer’s ear) is an inflammatory condition of the external ear canal auditory canal or auricle, usually from infection. Common infectious pathogens include S. aureus, S. epidermidis and P. aeruginosa; however, several other gram-positive, gram-negative and anaerobic infections along with polymicrobic infections occur frequently.6 Topical antibacterials (alone or in combination with a corticosteroid) are very effective and systemic therapy is generally not required.7 Acute otitis media is an inflammatory condition of the middle ear with middle ear effusion and symptoms include otalgia, hearing loss and vertigo.8 Common pathogens in children include S. pneumoniae and H. influenzae (and M. catarrhalis in children).8,9 Oral antibacterials are generally the initial treatment option for children and adults; however, topical antibacterials with or without corticosteroids may be used in patients with perforated tympanic membranes, tympanostomy -

Standard Treatment Guidelines and Essential Drugs List
STANDARD TREATMENT GUIDELINES AND ESSENTIAL DRUGS LIST FOR THE MINISTRY OF HEALTH, TONGA- 2007. Standard Treatment Guidelines Tonga 2007 Standard Treatment Guidelines and Essential Drugs List: Ministry of Health. First Edition, 2007 Copyright © 2007, Ministry of Health, Tonga All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, scanned or transmitted in any form without the permission of the copyright owner. Ministry of Health PO Box 59 Nuku’alofa Tonga Phone: 676 23200 Fax: 676 24291 E-mail address: [email protected] Editors: Siale ‘Akau’ola & Siutaka Siua Cover design by: Owen Towle Formatted by: T. Nauna Paongo Printed by: Taulua Press STG 2 Ministry of Health Standard Treatment Guidelines Tonga 2007 TABLE OF CONTENTS 1. FOREWORD: 13 2. ABBREVIATIONS AND ACRONYMS: 14 3. ACKNOWLEDGEMENTS: 17 4. INTRODUCTION: 19 5. ACCIDENT AND EMERGENCY (A&E): 21 5.1. General Approach to A&E 21 5.2. Cardiac Arrest 26 5.3. Other Life Threatening Emergencies 30 5.4. Infectious Diseases 52 5.5. Severe Hypertension 58 5.6. Abdominal Pain 59 5.7. Surgical Problems 60 5.8. Red Eye 66 5.9. Dog Bite 67 6. CARDIOVASCULAR CONDITIONS. 68 6.1. Heart Failure 68 6.2. Myocardial Infarction 72 6.3. Cardiogenic Shock 77 6.4. Acute Coronary Syndrome (ACS) 79 6.5. Cardiac Arrythmias 80 6.6. Cardiac Arrest 87 6.7. Hypertension 89 6.8. Aortic Dissection 93 6.9. Bacterial Endocarditis 96 6.10. Infective Endocarditis Prophylaxis 97 7. CENTRAL NERVOUS SYSTEM (CNS) CONDITIONS 104 7.1 Headache 104 STG 3 Ministry of Health Standard Treatment Guidelines Tonga 2007 7.2 Seizures 107 7.3 Meningitis 108 7.4 Stroke 108 7.5 Involuntary Movement Disorders 110 7.6 Epilepsy 111 8 COMMON EAR, NOSE AND THROAT PROBLEMS. -

Texas Medication Aides Basic Course Curriculum for Nursing Facilities and Related Institutions
Texas Medication Aides Basic course curriculum for Nursing Facilities and related institutions Effective Date: January 2017 Texas Health and Human Services Commisson (HHSC) Medication Aide Program, E‐416 P.O. Box 14930, Austin, Texas 78714‐9030 Communicate before you medicate! Helping people make the best of medications REVISED JUNE 2016 | Texas Health and Human Services Commisson (HHSC) HHSC Licensing and Credentialing TEXAS MEDICATION AIDE AND BASIC COURSE CURRICULUM 100‐hour curriculum Acknowledgements We would like to extend a very special thank you to the following people who worked many hours in revising and updating this curriculum. Your cooperation and dedication is appreciated. Darren Christian, R.N., Texas Health and Human Services Commisson, Elizabeth Demps, Texas Health and Human Services Commisson, Katherine Hafner, B.S, R.Ph, Fellow in the American Society of Consultant Pharmacists, Kim Lammons Texas Health and Human Services Commisson, Debi Majo, BSN R.N., TMF Health Quality Institute, Elizabeth McManamy, R.Ph, Texas Health and Human Services Commisson, Joyce Meredith, Texas Health and Human Services Commisson, Carolyn Reese, MSN, R.N., Blinn College, Brenda Renfro‐King, R.N., McLennan Community College, Jacqueline Smith, Texas Health and Human Services Commisson, Camden Frost, Texas Health and Human Services Commisson, Sean Steele, Texas Department on Aging and Disability Services, Sunny Stout, R.N., Senior Care Centers, Mavon Tidwell, R.N., Marble Falls High School, Kingsland Hills Care Center, Anne Trejo, Texas Health and Human Services Commisson. © 2016 Texas Health and Human Services Commisson (formerly Texas Department of Human Services) TEXAS HEALTH AND HUMAN SERVICES COMMISSION (HHSC) 1 TEXAS MEDICATION AIDE AND BASIC COURSE CURRICULUM 100‐hour curriculum Table of Contents: Medication Aide and basic course curriculum Unit I. -
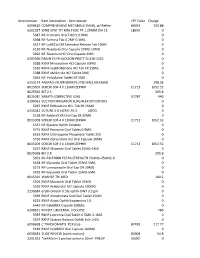
Item Master CPT Code Charge 6090610 COMPREHENSIVE
Item Number Item Description - Item Master CPT Code Charge 6090610 COMPREHENSIVE METABOLIC PANEL w/ Reflex- 80053 103.88 6202327 WIRE SYNT TIT KIRS TROC PT 1.25MM DIA 15 L8699 0 5387 NF-Premarin Oral Tablet 0.9MG 0 5398 NF-Falmina Tab 0.2MF-0.1MG 0 5517 NF-LaMICtal XR Extended Release Tab 100M 0 6130 NF-Nuedexta Oral Capsule 20MG-10MG 0 5992 NF-Terazosin HCl Oral Capsule 2MG 0 6203390 DRAIN 19 FR JACKSON-PRATT SU130-1325 0 5288 RXNF Minocycline HCl Capsule 50MG 0 5310 RXNF oxyMORphone HCl Tab ER 15MG 0 5388 RXNF aMILoride HCl Tablet 5MG 0 5564 NF- Felodipine Tablet ER 5MG 0 6213174 ANSPACH BURR 6MM FLUTED BALL MIA166B 298.36 8015007 SCREW SOF 4 X 11MM ZEPHIR C1713 1052.52 8025916 BIT 2.3 205.8 8026081 SA6AT5 CORRECTIVE LENS V2787 440 6200062 SUCTION IRRIGATOR SURGIFLEX 007200-903 0 5287 RXNF PARoxetine HCL Tab ER 25MG 0 6215042 SUTURE 3-0 VICRYL PS-2 J497G 0 6138 NF-Adderall XR Oral Cap ER 30MG 0 8015008 SCREW SOF 4 X 13MM ZEPHIR C1713 1052.52 5337 NF-Systane Ophth Solution 0 3774 RXNF Premarin Oral Tablet 0.9MG 0 6162 RXNF Chloroquine Phosphate Tablet 250 0 5756 RXNF Ziprasidone HCl Oral Capsule 20MG 0 8015009 SCREW SOF 4 X 15MM ZEPHIR C1713 1052.52 5427 RXNF Glyxambi Oral Tablet 25MG-5MG 0 8025918 BIT 2.5 205.8 5959 NF-EXCEDRIN EXTRA STRENGTH 250MG-250MG-6 0 5428 NF-Glyxambi Oral Tablet 25MG-5MG 0 5273 NF-Lansoprazole Oral Cap DR 30MG 0 5429 NF-Glyxambi Oral Tablet 25MG-5MG 0 8015391 WASHER TRI MED 180.2 5504 RXNF Movantik Oral Tablet 25MG 0 5336 RXNF Acebutolol HCl Capsule 200MG 0 2290384 erythromycin 0.5% ophth OINT 3.5 gm 0 5399 RXNF -

Policy and Procedure on Safe Medicaton Assistance And
Partnership Resources, Inc. POLICY AND PROCEDURE ON SAFE MEDICATION ASSISTANCE AND ADMINISTRATION I. PURPOSE The purpose of this policy is to establish guidelines to promote the health and safety of persons served by ensuring the safe assistance and administration of medication and treatments or other necessary procedures. II. POLICY Partnership Resources, Inc. (PRI) is responsible for meeting health service needs including medication-related services of persons as assigned in the Coordinated Service and Support Plan (CSSP) and/or CSSP Addendum. Persons served will be encouraged to participate in the process of medication administration to the fullest extent of their abilities, unless otherwise noted in the Coordinated Service and Support Plan and/or CSSP Addendum. The following procedures contain information on medication-related services for the administration of medication as well as the assistance staff may provide to a person who self-administers their own medication. All medications and treatments will be administered according to this policy and procedure and PRI’s medication administration training curriculum. III. PROCEDURE Staff training A. When medication set up and/or or administration has been assigned to PRI as stated in the Coordinated Service and Support Plan and/or CSSP Addendum, staff who will set up or administer medications to persons served will receive training and demonstrate competency as well as reviewing this policy and procedure. B. Unlicensed staff, prior to the set up and/or administration of medication, must successfully complete a medication set up or medication administration training course developed by a registered nurse or appropriate licensed health professional. The training curriculum must incorporate an observed skill assessment conducted by the trainer to ensure staff demonstrate the ability to safely and correctly follow medication procedures. -

Hospital Charges As of 2018 3
2018 ALL HOSPITAL CHARGES 2018 Charge Description CPT-4 code Price "L" PLATES - LEFT C1713 $ 645.47 (PT) CONTACT PRODUCT 85730 $ 16.32 (TB) DIRECT SMEAR 87206 $ 14.63 **FB REMOVAL RECTUM 45307 $ 6,123.85 .062 X 7 LONG GUIDE WIRE C1713 $ 86.25 .99MM TURBO ELITE LASER CATH C1885 $ 3,150.00 .99MM TURBO ELITE LASER CATHETER C1887 $ 2,200.00 0 27 GUT CHROMIC SH $ 14.87 0 30 ETHIBOND BRAIDED CT-1 $ 103.50 0 30 PROLENE MONO CTX $ 105.10 0 36 ETHIBOND BRAIDED V-7 $ 310.52 0 54 COATED VICRYL $ 33.80 0 54 GUT CHROMIC $ 33.02 0 54 GUT CHROMIC PLAIN $ 54.98 0 8-18 ETHIBOND EXTRA GRN MO-7 $ 240.30 0 8-18ETHIBOND EXTRA GRN CT-2 $ 206.51 0 PROLENE BL SH $ 129.30 0 SILK SUTUPAK 13 STRANDS 24 C1713 $ 35.55 0.8MM OFFSET PLATE C1713 $ 636.00 0.9MM CATH RAPD-EXCHANGE 150CM C1885 $ 3,150.00 0.9MM CATH X-80, CONT.ON RAPID-EXCHG 150 C1885 $ 3,150.00 02 SATURATION DIRECT 82810 $ 23.69 1 25-OH2D 82652 $ 104.57 1 27 GUT CHROMIC CT-1 $ 155.71 1 30 ETHIBOND BRAIDED DS-8 $ 157.52 1 30ETHIBOND BRAIDED CT-1 $ 87.92 1 36 GUT CHROMIC CTX $ 120.57 1 36 IN COATED VICRYL CTX $ 96.06 1 36 PDS II MONO CT $ 85.41 1 PDS II MONON TP-1 $ 72.48 1 PROLENE CTX $ 103.46 1 VERT MUSCLE 67314 $ 4,790.26 1 VICRYL 27CTB-1 $ 143.21 1.0MM 4 HOLE LARGE XLONG GAP C1713 $ 1,006.50 1.0MM 7HOLE PLATE STRGHT PLATE C1713 $ 1,158.00 1.1MM GUIDE WIRE C1713 $ 43.04 1.2 GUIDEWIRE C1713 $ 322.50 1.3 GUIDE PIN C1713 $ 30.12 1.3MM DRILL BIT MINI QC 55MM X C1713 $ 169.50 1.3MM TI T-PLATE C1713 $ 469.50 1.3MMTPLATE4HOLEHEAD/8HOLESHFT C1713 $ 562.50 1.4MM CATH 80HZ, CONT.ON RAPID-EX 150CM C1885 $ 4,200.00