Therapeutic Class Overview Otic Fluoroquinolones
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -
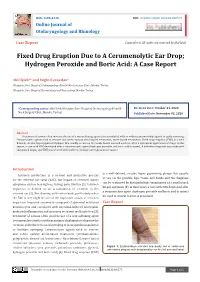
Fixed Drug Eruption Due to a Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: a Case Report
ISSN: 2688-8238 DOI: 10.33552/OJOR.2020.04.000577 Online Journal of Otolaryngology and Rhinology Case Report Copyright © All rights are reserved by Akif İşlek Fixed Drug Eruption Due to A Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: A Case Report Akif İşlek1* and Engin Karaaslan2 1Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey 2Nusaybin State Hospital, Dermatology and Venereology, Mardin, Turkey *Corresponding author: Received Date: October 24, 2020 Published Date: November 03, 2020 Akif İşlek, Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey. Abstract Treatment of earwax often involves the use of a wax softening agent (cerumenolytic) with or without antimicrobial agents to easily removing. Cerumenolytic agents used to remove and soften earwax areoil-based treatments, water-based treatments. Fixed drug eruption (FDE) is a well- defined, circular, hyperpigmented plaque that usually occurs on the trunk, hands mucosal surfaces, after a systemical application of drugs. In this report, a case with FDE developed after a cerumenolytic agent (hydrogen peroxide and boric acid in water). A definitive diagnosis was made with skin punch biopsy and FDE was treated with oral levocetirizine and topical mometasone. Introduction is a well-defined, circular, hyper pigmenting plaque that usually Cerumen production is a normal and protective process occurs on the genitals, lips, trunk, and hands and the diagnosis for the external ear canal (EAC), but impact of cerumen causes can be confirmed by histopathologic examination of a small punch symptoms such as hearing loss, itching, pain, tinnitus [1]. Cerumen biopsy specimen [5]. In this report, a case with FDE developed after impaction is defined as an accumulation of cerumen in the a cerumenolytic agent (hydrogen peroxide and boric acid in water) external ear [2]. -

Antibiotic Resistance in the European Union Associated with Therapeutic Use of Veterinary Medicines
The European Agency for the Evaluation of Medicinal Products Veterinary Medicines Evaluation Unit EMEA/CVMP/342/99-Final Antibiotic Resistance in the European Union Associated with Therapeutic use of Veterinary Medicines Report and Qualitative Risk Assessment by the Committee for Veterinary Medicinal Products 14 July 1999 Public 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Switchboard: (+44-171) 418 8400 Fax: (+44-171) 418 8447 E_Mail: [email protected] http://www.eudra.org/emea.html ãEMEA 1999 Reproduction and/or distribution of this document is authorised for non commercial purposes only provided the EMEA is acknowledged TABLE OF CONTENTS Page 1. INTRODUCTION 1 1.1 DEFINITION OF ANTIBIOTICS 1 1.1.1 Natural antibiotics 1 1.1.2 Semi-synthetic antibiotics 1 1.1.3 Synthetic antibiotics 1 1.1.4 Mechanisms of Action 1 1.2 BACKGROUND AND HISTORY 3 1.2.1 Recent developments 3 1.2.2 Authorisation of Antibiotics in the EU 4 1.3 ANTIBIOTIC RESISTANCE 6 1.3.1 Microbiological resistance 6 1.3.2 Clinical resistance 6 1.3.3 Resistance distribution in bacterial populations 6 1.4 GENETICS OF RESISTANCE 7 1.4.1 Chromosomal resistance 8 1.4.2 Transferable resistance 8 1.4.2.1 Plasmids 8 1.4.2.2 Transposons 9 1.4.2.3 Integrons and gene cassettes 9 1.4.3 Mechanisms for inter-bacterial transfer of resistance 10 1.5 METHODS OF DETERMINATION OF RESISTANCE 11 1.5.1 Agar/Broth Dilution Methods 11 1.5.2 Interpretative criteria (breakpoints) 11 1.5.3 Agar Diffusion Method 11 1.5.4 Other Tests 12 1.5.5 Molecular techniques 12 1.6 MULTIPLE-DRUG RESISTANCE -

Common Ear, Nose & Throat Problems
Common Ear, Nose & Throat Problems The information provided in this presentation is not intended to guide treatment or aid in making a diagnosis. Always consult a physician or nurse practitioner. Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Normal Larynx Normal larynx in a 44 yr old non-smoker Go to http://www.entusa.com/normal_larynx.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Acute Laryngitis This video shows the function of the larynx in a 24 yr old patient with acute laryngitis. Talking was painful and she only talked in a faint whisper. Go to http://www.entusa.com/laryngitis.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Paralysis This video shows the function of a larynx with a paralyzed left true vocal cord. The patient has lung cancer. She has a poorly compensated breathy voice which is difficult to understand. This patient had a 55 pack year history of smoking. Go to http://www.entusa.com/vocal_cord_paralysis_2.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Polyp This video shows the function of a larynx with a vocal cord polyp on the right true vocal cord. This patient smoked one pack a day for 30 years. Go to http://www.entusa.com/larynx_polyp-9.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Laryngeal Cancer This video shows the function of a larynx with a large T1b Cancer on both true vocal cords and anterior commissure in 72 yr old male with a 150 pack year history of smoking. -
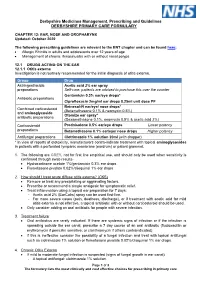
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

10/15-Hour Medication Test Answers
Appendix 10/15-Hour Medication Test Answers Name _________________________________ Facility _________________________________ Part 1: Match the term or phrase on the right with the abbreviation or term on the left by placing the correct letter on the appropriate line. _____ 1. PRN (p) a. milligram _____ 2. ac (e) b. at bedtime _____ 3. stat (j) c. Medication Administration Record _____ 4. SL (k) d. over the counter _____ 5. MAR (c) e. before meals _____ 6. mg (a) f. tablespoonful _____ 7. pc (m) g. placed and affixed to the skin _____ 8. OTC (d) h. teaspoonful _____ 9. Subcutaneous (r) i. milliliter _____ 10. po (n) j. immediately _____ 11. qhs (b) k. sublingual _____ 12. tbsp (f) l. placed under the tongue _____ 13. transdermal (g) m. after meals _____ 14. ml (i) n. by mouth _____ 15. gm (o) o. gram _____ 16. QOD (q) p. as needed _____ 17. tsp (h) q. every other day _____ 18. sublingual (l) r. inject into the fat with a syringe Medication Administration – March 2021 10/15-Hour Training Course for Adult Care Homes 4 Appendix 10/15-Hour Medication Test Answers – Continued Part 2: Fill in the blank with the appropriate word or term. You may choose to use the word bank below. 19. A heart tablet taken by mouth and swallowed is an example of a medication taken by the oral route. 20. A medication that is inserted into the rectum is given using the rectal route. 21. A topical medication is applied directly to the skin surface. -

Fluoroquinolone Mechanisms of Action and Resistance
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 1, 2021 - Published by Cold Spring Harbor Laboratory Press Topoisomerase Inhibitors: Fluoroquinolone Mechanisms of Action and Resistance David C. Hooper1 and George A. Jacoby2 1Division of Infectious Diseases, Massachusetts General Hospital, Boston, Massachusetts 02114 2Lahey Hospital and Medical Center, Burlington, Massachusetts 01805 Correspondence: [email protected] Quinolone antimicrobials are widely used in clinical medicine and are the only current class of agents that directly inhibit bacterial DNA synthesis. Quinolones dually target DNA gyrase and topoisomerase IV binding to specific domains and conformations so as to block DNA strand passage catalysis and stabilize DNA–enzyme complexes that block the DNA repli- cation apparatus and generate double breaks in DNA that underlie their bactericidal activity. Resistance has emerged with clinical use of these agents and is common in some bacterial pathogens. Mechanisms of resistance include mutational alterations in drug target affinity and efflux pump expression and acquisition of resistance-conferring genes. Resistance mu- tations in one or both of the two drug target enzymes are commonly in a localized domain of the GyrA and ParC subunits of gyrase and topoisomerase IV, respectively, and reduce drug binding to the enzyme–DNA complex. Other resistance mutations occur in regulatory genes that control the expression of native efflux pumps localized in the bacterial membrane(s). These pumps have broad substrate profiles that include other antimicrobials as well as quin- olones. Mutations of both types can accumulate with selection pressure and produce highly resistant strains. Resistance genes acquired on plasmids confer low-level resistance that promotes the selection of mutational high-level resistance. -

PACKAGE LEAFLET: INFORMATION for the USER Levofloxacin 5 Mg
PACKAGE LEAFLET: INFORMATION FOR THE USER Levofloxacin 5 mg/ml solution for infusion Levofloxacin Read all of this leaflet carefully before you are given this medicine because it contains important information for you • Keep this leaflet. You may need to read it again. • If you have any further questions, ask your doctor, pharmacist or nurse. • This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. • If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Levofloxacin solution for infusion is and what it is used for 2. What you need to know before you are given Levofloxacin solution for infusion 3. How Levofloxacin solution for infusion is given 4. Possible side effects 5. How to store Levofloxacin solution for infusion 6. Contents of the pack and other information 1. What Levofloxacin solution for infusion is and what it is used for The name of your medicine is Levofloxacin solution for infusion. Levofloxacin solution for infusion contains a medicine called levofloxacin. This belongs to a group of medicines called antibiotics. Levofloxacin is a ’quinolone’ antibiotic. It works by killing the bacteria that cause infections in your body. Levofloxacin solution for infusion can be used to treat infections of the: • Lungs, in people with pneumonia • Urinary tract, including your kidneys or bladder • Prostate gland, where you have a long lasting infection • Skin and underneath the skin, including muscles. -

Disabling and Potentially Permanent Side Effects Lead to Suspension Or Restrictions of Quinolone and Fluoroquinolone Antibiotics
16 November 2018 EMA/795349/2018 Disabling and potentially permanent side effects lead to suspension or restrictions of quinolone and fluoroquinolone antibiotics EMA has reviewed serious, disabling and potentially permanent side effects with quinolone and fluoroquinolone antibiotics given by mouth, injection or inhalation. The review incorporated the views of patients, healthcare professionals and academics presented at EMA’s public hearing on fluoroquinolone and quinolone antibiotics in June 2018. EMA’s human medicines committee (CHMP) has endorsed the recommendations of EMA’s safety committee (PRAC) and concluded that the marketing authorisation of medicines containing cinoxacin, flumequine, nalidixic acid, and pipemidic acid should be suspended. The CHMP confirmed that the use of the remaining fluoroquinolone antibiotics should be restricted. In addition, the prescribing information for healthcare professionals and information for patients will describe the disabling and potentially permanent side effects and advise patients to stop treatment with a fluoroquinolone antibiotic at the first sign of a side effect involving muscles, tendons or joints and the nervous system. Restrictions on the use of fluoroquinolone antibiotics will mean that they should not be used: • to treat infections that might get better without treatment or are not severe (such as throat infections); • to treat non-bacterial infections, e.g. non-bacterial (chronic) prostatitis; • for preventing traveller’s diarrhoea or recurring lower urinary tract infections (urine infections that do not extend beyond the bladder); • to treat mild or moderate bacterial infections unless other antibacterial medicines commonly recommended for these infections cannot be used. Importantly, fluoroquinolones should generally be avoided in patients who have previously had serious side effects with a fluoroquinolone or quinolone antibiotic. -

Pharmaceutical Services Division and the Clinical Research Centre Ministry of Health Malaysia
A publication of the PHARMACEUTICAL SERVICES DIVISION AND THE CLINICAL RESEARCH CENTRE MINISTRY OF HEALTH MALAYSIA MALAYSIAN STATISTICS ON MEDICINES 2008 Edited by: Lian L.M., Kamarudin A., Siti Fauziah A., Nik Nor Aklima N.O., Norazida A.R. With contributions from: Hafizh A.A., Lim J.Y., Hoo L.P., Faridah Aryani M.Y., Sheamini S., Rosliza L., Fatimah A.R., Nour Hanah O., Rosaida M.S., Muhammad Radzi A.H., Raman M., Tee H.P., Ooi B.P., Shamsiah S., Tan H.P.M., Jayaram M., Masni M., Sri Wahyu T., Muhammad Yazid J., Norafidah I., Nurkhodrulnada M.L., Letchumanan G.R.R., Mastura I., Yong S.L., Mohamed Noor R., Daphne G., Kamarudin A., Chang K.M., Goh A.S., Sinari S., Bee P.C., Lim Y.S., Wong S.P., Chang K.M., Goh A.S., Sinari S., Bee P.C., Lim Y.S., Wong S.P., Omar I., Zoriah A., Fong Y.Y.A., Nusaibah A.R., Feisul Idzwan M., Ghazali A.K., Hooi L.S., Khoo E.M., Sunita B., Nurul Suhaida B.,Wan Azman W.A., Liew H.B., Kong S.H., Haarathi C., Nirmala J., Sim K.H., Azura M.A., Asmah J., Chan L.C., Choon S.E., Chang S.Y., Roshidah B., Ravindran J., Nik Mohd Nasri N.I., Ghazali I., Wan Abu Bakar Y., Wan Hamilton W.H., Ravichandran J., Zaridah S., Wan Zahanim W.Y., Kannappan P., Intan Shafina S., Tan A.L., Rohan Malek J., Selvalingam S., Lei C.M.C., Ching S.L., Zanariah H., Lim P.C., Hong Y.H.J., Tan T.B.A., Sim L.H.B, Long K.N., Sameerah S.A.R., Lai M.L.J., Rahela A.K., Azura D., Ibtisam M.N., Voon F.K., Nor Saleha I.T., Tajunisah M.E., Wan Nazuha W.R., Wong H.S., Rosnawati Y., Ong S.G., Syazzana D., Puteri Juanita Z., Mohd. -

On the Extraction of Antibiotics from Shrimps Prior to Chromatographic Analysis
separations Review On the Extraction of Antibiotics from Shrimps Prior to Chromatographic Analysis Victoria Samanidou *, Dimitrios Bitas, Stamatia Charitonos and Ioannis Papadoyannis Laboratory of Analytical Chemistry, University of Thessaloniki, GR 54124 Thessaloniki, Greece; [email protected] (D.B.); [email protected] (S.C.); [email protected] (I.P.) * Correspondence: [email protected]; Tel.: +30-2310-997698; Fax: +30-2310-997719 Academic Editor: Frank L. Dorman Received: 2 February 2016; Accepted: 26 February 2016; Published: 4 March 2016 Abstract: The widespread use of antibiotics in veterinary practice and aquaculture has led to the increase of antimicrobial resistance in food-borne pathogens that may be transferred to humans. Global concern is reflected in the regulations from different agencies that have set maximum permitted residue limits on antibiotics in different food matrices of animal origin. Sensitive and selective methods are required to monitor residue levels in aquaculture species for routine regulatory analysis. Since sample preparation is the most important step, several extraction methods have been developed. In this review, we aim to summarize the trends in extraction of several antibiotics classes from shrimps and give a comparison of performance characteristics in the different approaches. Keywords: sample preparation; extraction; aquaculture; shrimps; chromatography; antibiotics 1. Introduction According to FAO (CWP Handbook of Fishery Statistical Standards, Section J: AQUACULTURE), “aquaculture is the farming of aquatic organisms: fish, mollusks, crustaceans, aquatic plants, crocodiles, alligators, turtles, and amphibians. Farming implies some form of intervention in the rearing process to enhance production, such as regular stocking, feeding, protection from predators, etc.”[1]. Since 1960, aquaculture practice and production has increased as a result of the improved conditions in the aquaculture facilities. -

LEVAQUIN (Levofloxacin) Tablets Are Supplied As 250, 500, and 750 Mg Capsule-Shaped, Coated Tablets
LEVAQUIN (levofloxacin) TABLETS LEVAQUIN (levofloxacin) ORAL SOLUTION LEVAQUIN (levofloxacin) INJECTION LEVAQUIN (levofloxacin in 5% dextrose) INJECTION To reduce the development of drug-resistant bacteria and maintain the effectiveness of LEVAQUIN (levofloxacin) and other antibacterial drugs, LEVAQUIN should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION LEVAQUIN (levofloxacin) is a synthetic broad spectrum antibacterial agent for oral and intravenous administration. Chemically, levofloxacin, a chiral fluorinated carboxyquinolone, is the pure (-)-(S)-enantiomer of the racemic drug substance ofloxacin. The chemical name is (-)-(S)-9-fluoro-2,3-dihydro-3-methyl-10-(4-methyl- 1-piperazinyl)-7-oxo-7H-pyrido[1,2,3-de]-1,4-benzoxazine-6-carboxylic acid hemihydrate. O F COOH 1/2 H2O N N N O CH3 H3C The chemical structure is: H Its empirical formula is C18H20FN3O4 • ½ H2O and its molecular weight is 370.38. Levofloxacin is a light yellowish-white to yellow-white crystal or crystalline powder. The molecule exists as a zwitterion at the pH conditions in the small intestine. The data demonstrate that from pH 0.6 to 5.8, the solubility of levofloxacin is essentially constant (approximately 100 mg/mL). Levofloxacin is considered soluble to freely soluble in this pH range, as defined by USP nomenclature. Above pH 5.8, the solubility increases rapidly to its maximum at pH 6.7 (272 mg/mL) and is considered freely soluble in this range. Above pH 6.7, the solubility decreases and reaches a minimum value (about 50 mg/mL) at a pH of approximately 6.9.