Texas Medication Aides Basic Course Curriculum for Nursing Facilities and Related Institutions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -
Fixed Drug Eruption Due to a Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: a Case Report
ISSN: 2688-8238 DOI: 10.33552/OJOR.2020.04.000577 Online Journal of Otolaryngology and Rhinology Case Report Copyright © All rights are reserved by Akif İşlek Fixed Drug Eruption Due to A Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: A Case Report Akif İşlek1* and Engin Karaaslan2 1Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey 2Nusaybin State Hospital, Dermatology and Venereology, Mardin, Turkey *Corresponding author: Received Date: October 24, 2020 Published Date: November 03, 2020 Akif İşlek, Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey. Abstract Treatment of earwax often involves the use of a wax softening agent (cerumenolytic) with or without antimicrobial agents to easily removing. Cerumenolytic agents used to remove and soften earwax areoil-based treatments, water-based treatments. Fixed drug eruption (FDE) is a well- defined, circular, hyperpigmented plaque that usually occurs on the trunk, hands mucosal surfaces, after a systemical application of drugs. In this report, a case with FDE developed after a cerumenolytic agent (hydrogen peroxide and boric acid in water). A definitive diagnosis was made with skin punch biopsy and FDE was treated with oral levocetirizine and topical mometasone. Introduction is a well-defined, circular, hyper pigmenting plaque that usually Cerumen production is a normal and protective process occurs on the genitals, lips, trunk, and hands and the diagnosis for the external ear canal (EAC), but impact of cerumen causes can be confirmed by histopathologic examination of a small punch symptoms such as hearing loss, itching, pain, tinnitus [1]. Cerumen biopsy specimen [5]. In this report, a case with FDE developed after impaction is defined as an accumulation of cerumen in the a cerumenolytic agent (hydrogen peroxide and boric acid in water) external ear [2]. -

Priority for Everyone, and Even More So for Those with Chronic Illnesses
Mouth Care: Patient/Caregiver Training Hospice of Cincinnati Mouth Care is a high priority for everyone, and even more so for those with chronic illnesses. Proper mouth care has many benefits including: 1. Increasing appetite 2. Maintaining comfort 3. Clearer speech 4. Easier swallowing 5. Preventing sores and infection. General tips: Mouth care should be performed a minimum of twice daily and more frequently for dry mouth, if breathing through the mouth, or if you are not eating. Mouth care should always be performed after using an inhaler/nebulizer to prevent thrush. Thrush is slightly raised white patches or a rash typically seen on the tongue or inner cheeks. There may be pain with swallowing. Contact your hospice nurse immediately if you suspect thrush. Dentures may no longer fit well. You may consider using them only when eating or when visiting with friends and family. Questions or concerns? Call a hospice nurse at 513-891-7700. Training: Mouth Care. ©2017 Hospice of Cincinnati Hospice of Cincinnati Relieving dry mouth: 1. Increase frequency of mouth care. 2. Encourage sucking on candy, ice chips, popsicles or taking small sips of water to increase saliva. 3. Use of a mouthwash can increase dryness. Talk to your nurse about a proper mouth moisturizer/artificial saliva product. For those with difficulty swallowing: • Raise the head of the bed and support the head with pillows, turn head to one side. • Cover the upper body with a towel to keep the area clean and dry. • Remove dentures prior to mouth care and brush separately. • Use a toothette, which is a sponge-tipped oral swab, to clean the mouth and teeth using a small amount of toothpaste. -

Hydrogen Peroxide, and This Is the Same Substance That Can Be Purchased in a 32-Ounce Plastic Bottle at Walmart, for 88 Cents, Or at Walgreens for Under a $1.00
An At-Home Treatment That Can Cure Any Virus, Including Coronavirus Originally Conceptualized, circa 1990, by Charles Farr, MD Subsequently Researched and Prescribed by Frank Shallenberger, MD Current Protocol Created by Thomas Levy, MD, JD Although COVID-19, aka coronavirus, is deadly in some select cases, and it can spread rapidly, there is a simple, very inexpensive, and highly effective treatment that can treat and rapidly resolve coronavirus and virtually any other respiratory virus. While different individuals can be expected to have variable degrees of positive response, this intervention can be anticipated to eliminate eventual fatal disease outcomes in all but the most advanced cases. As I hope you will eventually experience, the treatment works for all acute viral infections, and especially well for flu viruses of any variety. In fact, although we are constantly conditioned to not believe in anything “too good to be true,” you will never have to worry about getting a cold or the flu again because you can cure it on your own. The key ingredient in this treatment is common household 3% hydrogen peroxide, and this is the same substance that can be purchased in a 32-ounce plastic bottle at Walmart, for 88 cents, or at Walgreens for under a $1.00. Perhaps you have never heard of hydrogen peroxide therapy, but since the treatment was first championed by Dr. Charles Farr in about 1990, thousands of doctors have used this therapy for decades to conquer infections in many thousands of patients throughout the world. How and Why Hydrogen Peroxide Works Because hydrogen peroxide consists of a water molecule (H2O) with an extra oxygen atom (H2O2), it is this extra oxygen atom that makes it so deadly for viruses. -

Common Ear, Nose & Throat Problems
Common Ear, Nose & Throat Problems The information provided in this presentation is not intended to guide treatment or aid in making a diagnosis. Always consult a physician or nurse practitioner. Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Normal Larynx Normal larynx in a 44 yr old non-smoker Go to http://www.entusa.com/normal_larynx.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Acute Laryngitis This video shows the function of the larynx in a 24 yr old patient with acute laryngitis. Talking was painful and she only talked in a faint whisper. Go to http://www.entusa.com/laryngitis.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Paralysis This video shows the function of a larynx with a paralyzed left true vocal cord. The patient has lung cancer. She has a poorly compensated breathy voice which is difficult to understand. This patient had a 55 pack year history of smoking. Go to http://www.entusa.com/vocal_cord_paralysis_2.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Polyp This video shows the function of a larynx with a vocal cord polyp on the right true vocal cord. This patient smoked one pack a day for 30 years. Go to http://www.entusa.com/larynx_polyp-9.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Laryngeal Cancer This video shows the function of a larynx with a large T1b Cancer on both true vocal cords and anterior commissure in 72 yr old male with a 150 pack year history of smoking. -
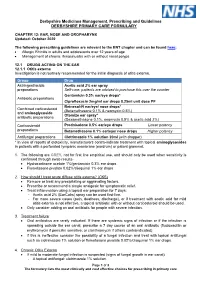
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

Formulary (List of Covered Drugs)
3ODQ<HDU 202 Formulary (List of Covered Drugs) PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THE FOLLOWING PLAN: $0 Cost Share AI/AN HMO Minimum Coverage HMO Silver 70 HMO Active Choice PPO Silver Opal 25 Gold HMO Silver 70 OFF Exchange HMO Amber 50 HMO Silver Opal 50 Silver HMO Silver 73 HMO Bronze 60 HDHP HMO Platinum 90 HMO Silver 87 HMO Bronze 60 HMO Ruby 10 Platinum HMO Silver 94 HMO Gold 80 HMO Ruby 20 Platinum HMO Jade 15 HMO Ruby 40 Platinum HMO This formulary was last updated on8//20. This formulary is VXEMHFWto change and all previous versions of the formulary no longer apply. For more recent information or other questions, please contact Chinese Community Health Plan Member Services at 1-888-775-7888 or, for TTY users, 1-877-681-8898, seven days a week from 8:00 a.m. to 8:00 p.m., or visit www.cchphealthplan.com/family-member -,-ϭ -,-ϭ"&* !#" + 5 5 ),-$+" %(%'.')/"+#" %&/"+ -%/"$)% "%&/"+ *& )&! %&/"+ 0 $(#" '"+ %&/"+ *& %&/"+ %&/"+ +)(2" &-%(.' %&/"+ +)(2" .1&-%(.' %&/"+ )&! .1&-%(.' !" .1&-%(.' dŚŝƐĨŽƌŵƵůĂƌLJǁĂƐůĂƐƚƵƉĚĂƚĞĚ8ͬϭͬϮϬϮϭ͘dŚŝƐĨŽƌŵƵůĂƌLJŝƐƐƵďũĞĐƚƚŽ ĐŚĂŶŐĞĂŶĚĂůůƉƌĞǀŝŽƵƐǀĞƌƐŝŽŶƐŽĨƚŚĞĨŽƌŵƵůĂƌLJŶŽůŽŶŐĞƌĂƉƉůLJ͘&ŽƌŵŽƌĞ ƌĞĐĞŶƚŝŶĨŽƌŵĂƚŝŽŶŽƌŽƚŚĞƌƋƵĞƐƚŝŽŶƐ͕ƉůĞĂƐĞĐŽŶƚĂĐƚŚŝŶĞƐĞŽŵŵƵŶŝƚLJ ,ĞĂůƚŚWůĂŶDĞŵďĞƌ^ĞƌǀŝĐĞƐĂƚϭͲϴϴϴͲϳϳϱͲϳϴϴϴŽƌ͕ĨŽƌddzƵƐĞƌƐ͕ ϭͲϴϳϳͲϲϴϭͲϴϴϵϴ͕ƐĞǀĞŶĚĂLJƐĂǁĞĞŬĨƌŽŵϴ͗ϬϬĂ͘ŵ͘ƚŽϴ͗ϬϬƉ͘ŵ͕͘ŽƌǀŝƐŝƚ ǁǁǁ͘ĐĐŚƉŚĞĂůƚŚƉůĂŶ͘ĐŽŵͬĨĂŵŝůLJͲŵĞŵďĞƌ !! %+)&,+ &%+&+&)$,#)0),# *+666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666I % + &%*6666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666I -

10/15-Hour Medication Test Answers
Appendix 10/15-Hour Medication Test Answers Name _________________________________ Facility _________________________________ Part 1: Match the term or phrase on the right with the abbreviation or term on the left by placing the correct letter on the appropriate line. _____ 1. PRN (p) a. milligram _____ 2. ac (e) b. at bedtime _____ 3. stat (j) c. Medication Administration Record _____ 4. SL (k) d. over the counter _____ 5. MAR (c) e. before meals _____ 6. mg (a) f. tablespoonful _____ 7. pc (m) g. placed and affixed to the skin _____ 8. OTC (d) h. teaspoonful _____ 9. Subcutaneous (r) i. milliliter _____ 10. po (n) j. immediately _____ 11. qhs (b) k. sublingual _____ 12. tbsp (f) l. placed under the tongue _____ 13. transdermal (g) m. after meals _____ 14. ml (i) n. by mouth _____ 15. gm (o) o. gram _____ 16. QOD (q) p. as needed _____ 17. tsp (h) q. every other day _____ 18. sublingual (l) r. inject into the fat with a syringe Medication Administration – March 2021 10/15-Hour Training Course for Adult Care Homes 4 Appendix 10/15-Hour Medication Test Answers – Continued Part 2: Fill in the blank with the appropriate word or term. You may choose to use the word bank below. 19. A heart tablet taken by mouth and swallowed is an example of a medication taken by the oral route. 20. A medication that is inserted into the rectum is given using the rectal route. 21. A topical medication is applied directly to the skin surface. -

Smoking and Asthma
If you smoke and have asthma, the most important step you can take to improve your health and reduce asthma attacks is to QUIT SMOKING . Tobacco smoke is a major trigger for asthma attacks. Asthmatic breathing tube triggered by smoking Muscles tighten and squeeze tubes Extra mucus forms inside tubes Tubes swell and fill with fluid Asthmatic breathing tube Normal breathing tube Eight hours after your last cigarette, oxygen levels in your No matter blood return to normal. After 72 hours (3 days), breathing tubes relax, lung capacity how long increases, and breathing is easier. After 1 to 9 months, sinus congestion, coughing, fatigue, you smoked, and shortness of breath decrease. Your lungs’ ability to quitting helps clean themselves and handle mucus improves. Chances of lung infections are reduced. you b r e a t h e You’ll save trips to the doctor and ER and save money on asthma medication or possibly not buy it at all. more easily! You’ll save money from no longer buying cigarettes! TOBACCO CESSATION PROGRAM | 2600 TOWER DRIVE, SUITE 216, MONROE Tobacco smoke is the most toxic indoor Quitting smoking is difficult to do alone, air pollutant that triggers asthma. but support is available through your It is worse than dust mites, St. Francis Tobacco Cessation Program. cockroaches, and mold, and people with asthma should not smoke or be around secondhand smoke. Any time you need assistance WHAT HAPPENS WHEN with your cessation journey, need to ask questions YOU QUIT SMOKING or just need to talk, When a person who has asthma quits smok- call us at (318) 966-QUIT. -

Novel Therapeutic Approaches to Eosinophilic Esophagitis
Novel Therapeutic Approaches to Eosinophilic Esophagitis Claire Beveridge, MD, and Gary W. Falk, MD, MS Dr Beveridge is a gastroenterology Abstract: Eosinophilic esophagitis is a chronic inflammatory condi- and hepatology fellow and Dr Falk is a tion that requires treatment to improve symptoms and prevent professor of medicine in the Division complications of esophageal remodeling, such as strictures and of Gastroenterology and Hepatology narrow-caliber esophagus. First-line treatments include proton at the University of Pennsylvania Perelman School of Medicine in pump inhibitors, topical corticosteroids, elimination or elemental Philadelphia, Pennsylvania. diets, and esophageal dilation. Topical corticosteroids have typi- cally required repurposing inhaled asthma medications by swal- lowing an aerosolized medication or mixing a nebulizer solution Address correspondence to: into a slurry. New topical corticosteroid formulations undergoing Dr Gary W. Falk investigation include a premade budesonide oral suspension and Division of Gastroenterology and Hepatology disintegrating budesonide and fluticasone propionate tablets. The University of Pennsylvania Perelman approach to an elimination diet is also changing, with an emphasis School of Medicine on patient preference when considering a traditional 6-food elim- Perelman Center for Advanced ination diet compared with a step-up approach. This approach Medicine involves eliminating only 2 or 4 foods initially and expanding if 7th Floor South Pavilion 750 necessary. While this method can be initially less effective for some 3400 Civic Center Boulevard Philadelphia, PA 19104 patients, it generally involves fewer endoscopies and minimizes Tel: 215-615-4951 diet restriction. Beyond conventional therapies, a number of novel Fax: 215-349-5915 biologic agents are also under investigation. These include week- E-mail: gary.falk@pennmedicine. -

Anthem Blue Cross Prescription Formulary List
National Drug List Drug list — Three Tier Drug Plan Your prescription benefit comes with a drug list, which is also called a formulary. This list is made up of brand-name and generic prescription drugs approved by the U.S. Food & Drug Administration (FDA). We’re here to help. If you are a current Anthem member with questions about your pharmacy benefits, we're here to help. Just call us at the Member Services number on your ID card. The plan names to which this formulary applies are shown below. Solution PPO 1500/15/20 $5/$15/$50/$65/30% to $250 after deductible Solution PPO 2000/20/20 $5/$20/$30/$50/30% to $250 Solution PPO 2500/25/20 $5/$20/$40/$60/30% to $250 Solution PPO 3500/30/30 $5/$20/$40/$60/30% to $250 Rx ded $150 Solution PPO 4500/30/30 $5/$20/$40/$75/30% to $250 Solution PPO 5500/30/30 $5/$20/$40/$75/30% to $250 Rx ded $250 $5/$15/$25/$45/30% to $250 $5/$20/$50/$65/30% to $250 Rx ded $500 $5/$15/$30/$50/30% to $250 $5/$20/$50/$70/30% to $250 $5/$15/$40/$60/30% to $250 $5/$20/$50/$70/30% to $250 after deductible Here are a few things to remember: o You can view and search our current drug lists when you visit anthem.com/ca/pharmacyinformation. Please note: The formulary is subject to change and all previous versions of the formulary are no longer in effect. -

Using an Inhaler and Nebulizer
inhalercover.pdf 1 8/27/18 7:32 AM Using an Inhaler and Nebulizer C M Y CM MY CY CMY K Using an Inhaler and Nebulizer Inhalers An inhaler is a handheld device. It delivers medication directly into your airways. Inhalers are commonly used to treat problems that affect your ability to breathe. Your health care provider may recommend that you use an inhaler if you have: • Asthma. • Chronic obstructive pulmonary disease. • Other ongoing respiratory problems. The asthma medications delivered by the inhalers include: • Bronchodilators. • Steroids. • Combination of bronchodilators and steroids. Bronchodilators cause small airways in the lungs to open up. Steroids are used to relieve swelling and inflammation. Some inhalers are meant for limited use during an emergency situation. Others are used daily to prevent breathing problems. Using the right amount of medication is important in the treatment and prevention of ongoing respiratory problems. Medications can also decrease the sensitivity of the lungs to allergens. Inhalers are commonly used to deliver these medications directly into the airways. Inhaled medicine relieves symptoms faster than the same medicine given in pill form. Using an Inhaler and Nebulizer 1 Fewer side effects happen when medicine is delivered by an inhaler instead of taken in pill form. That’s because medicine from an inhaler goes directly into the airways. Very little medicine ends up in the bloodstream. Inhalers come in many different forms. The most commonly used inhalers are: • Metered dose inhalers. • Metered dose inhalers with a spacer. • Dry powder inhalers. A metered dose inhaler, or MDI, is a small aerosol canister that holds medicine.