A Patient's Guide To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Priority for Everyone, and Even More So for Those with Chronic Illnesses
Mouth Care: Patient/Caregiver Training Hospice of Cincinnati Mouth Care is a high priority for everyone, and even more so for those with chronic illnesses. Proper mouth care has many benefits including: 1. Increasing appetite 2. Maintaining comfort 3. Clearer speech 4. Easier swallowing 5. Preventing sores and infection. General tips: Mouth care should be performed a minimum of twice daily and more frequently for dry mouth, if breathing through the mouth, or if you are not eating. Mouth care should always be performed after using an inhaler/nebulizer to prevent thrush. Thrush is slightly raised white patches or a rash typically seen on the tongue or inner cheeks. There may be pain with swallowing. Contact your hospice nurse immediately if you suspect thrush. Dentures may no longer fit well. You may consider using them only when eating or when visiting with friends and family. Questions or concerns? Call a hospice nurse at 513-891-7700. Training: Mouth Care. ©2017 Hospice of Cincinnati Hospice of Cincinnati Relieving dry mouth: 1. Increase frequency of mouth care. 2. Encourage sucking on candy, ice chips, popsicles or taking small sips of water to increase saliva. 3. Use of a mouthwash can increase dryness. Talk to your nurse about a proper mouth moisturizer/artificial saliva product. For those with difficulty swallowing: • Raise the head of the bed and support the head with pillows, turn head to one side. • Cover the upper body with a towel to keep the area clean and dry. • Remove dentures prior to mouth care and brush separately. • Use a toothette, which is a sponge-tipped oral swab, to clean the mouth and teeth using a small amount of toothpaste. -

Hydrogen Peroxide, and This Is the Same Substance That Can Be Purchased in a 32-Ounce Plastic Bottle at Walmart, for 88 Cents, Or at Walgreens for Under a $1.00
An At-Home Treatment That Can Cure Any Virus, Including Coronavirus Originally Conceptualized, circa 1990, by Charles Farr, MD Subsequently Researched and Prescribed by Frank Shallenberger, MD Current Protocol Created by Thomas Levy, MD, JD Although COVID-19, aka coronavirus, is deadly in some select cases, and it can spread rapidly, there is a simple, very inexpensive, and highly effective treatment that can treat and rapidly resolve coronavirus and virtually any other respiratory virus. While different individuals can be expected to have variable degrees of positive response, this intervention can be anticipated to eliminate eventual fatal disease outcomes in all but the most advanced cases. As I hope you will eventually experience, the treatment works for all acute viral infections, and especially well for flu viruses of any variety. In fact, although we are constantly conditioned to not believe in anything “too good to be true,” you will never have to worry about getting a cold or the flu again because you can cure it on your own. The key ingredient in this treatment is common household 3% hydrogen peroxide, and this is the same substance that can be purchased in a 32-ounce plastic bottle at Walmart, for 88 cents, or at Walgreens for under a $1.00. Perhaps you have never heard of hydrogen peroxide therapy, but since the treatment was first championed by Dr. Charles Farr in about 1990, thousands of doctors have used this therapy for decades to conquer infections in many thousands of patients throughout the world. How and Why Hydrogen Peroxide Works Because hydrogen peroxide consists of a water molecule (H2O) with an extra oxygen atom (H2O2), it is this extra oxygen atom that makes it so deadly for viruses. -

California Essential Drug List
California Essential Drug List The Essential Drug List (formulary) includes a list of drugs covered by Health Net. The drug list is updated at least monthly and is subject to change. All previous versions are no longer in effect. You can view the most current drug list by going to our website at www.healthnet.com. Refer to Evidence of Coverage or Certificate of Insurance for specific cost share information. For California Individual & Family Plans: Drug Lists Select Health Net Large Group – Formulary (pdf). For Small Business Group: Drug Lists Select Health Net Small Business Group – Formulary (pdf). NOTE: To search the drug list online, open the (pdf) document. Hold down the “Control” (Ctrl) and “F” keys. When the search box appears, type the name of your drug and press the “Enter” key. If you have questions or need more information call us toll free. California Individual & Family Plans (off-Exchange) If you have questions about your pharmacy coverage call Customer Service at 1-800-839-2172 California Individual & Family Plans (on-Exchange) If you have questions about your pharmacy coverage call Customer Service at 1-888-926-4988 Hours of Operation 8:00am – 7:00pm Monday through Friday 8:00am – 5:00pm Saturday Small Business Group If you have questions about your pharmacy coverage call Customer Service at 1-800-361-3366 Hours of Operation 8:00am – 6:00pm Monday through Friday Updated September 1, 2021 Health Net of California, Inc. and Health Net Life Insurance Company are subsidiaries of Health Net, LLC and Centene Corporation. Health Net is a registered service mark of Health Net, LLC Table of Contents What If I Have Questions Regarding My Pharmacy Benefit? ................................... -
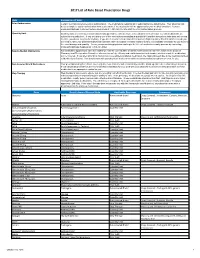
2017 List of Rule Based Prescription Drugs
2017 List of Rule Based Prescription Drugs Rule Explanation of Rule Prior Authorization Certain medications require a prior authorization. The medications requiring prior authorization are listed below. Your physician will need to complete a prior authorization form to determine if the medication will be approved for your medical condition. Contact EnvisionRXOptions Customer Service Help Desk at 1-800-361-4542 to start the Prior Authorization process. Quantity Limit Quantity limits are clinically recommended limits put in place to help ensure safe utilization of medication. Certain medications are subject to a quantity limit. If you are taking one of the medications mandating a quantity limit and the amount you take does not exceed the limit, you do not need to do anything. If you are in need of a medication that requires a higher quantity than that which is listed, you will need to have your prescribing physician submit a letter of medical necessity explaining why it is medically necessary for you to be on the exact dosage and quantity. You or your prescribing physician can begin the letter of medical necessity process by contacting EnvisionRXOptions Helpdesk at 1-800-361-4542. New-to-Market Medications Any medication approved to enter the market will only be covered after a clinical review decision has been made by the Envision Pharmacy and Therapeutics Committee who reviews safety, efficacy and cost information to determine whether or not the medication will be covered. If you attempt to fill or claim a non-covered New-to-Market medication, the claim will reject due to the medications New- to-Market classification. -
Medi-Cal Formulary May 2020
Formulary Medi-Cal MAY 2020 The IEHP Medi-Cal Formulary is subject to change throughout the year. All previous versions of the formulary are no longer in effect once a new formulary is available. The IEHP Medi-Cal Formulary can be found at: www.iehp.org/en/members/medical Last Updated: 04/17/2020 Inland Empire Health Plan (IEHP) Medi-Cal Formulary Table of Contents A . Foreword ..................................................................................................................... 2 B. IEHP Member Services .............................................................................................. 2 C. How to Use the Formulary .......................................................................................... 2 D. Prescription Coverage ................................................................................................. 3 D1. Quantity Limits .................................................................................................... 3 D2. Step Therapy ........................................................................................................ 3 E. Filling a Prescription and IEHP’s Pharmacy Network ............................................... 4 F. Definitions ................................................................................................................... 4 G. List of Covered Drugs .............................................................................................. 10 H. Index ....................................................................................................................... -

Inhalation Drug Delivery Devices: Technology Update
Medical Devices: Evidence and Research Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Inhalation drug delivery devices: technology update Mariam Ibrahim Abstract: The pulmonary route of administration has proven to be effective in local and Rahul Verma systemic delivery of miscellaneous drugs and biopharmaceuticals to treat pulmonary and non- Lucila Garcia-Contreras pulmonary diseases. A successful pulmonary administration requires a harmonic interaction between the drug formulation, the inhaler device, and the patient. However, the biggest single Department of Pharmaceutical Sciences, College of Pharmacy, problem that accounts for the lack of desired effect or adverse outcomes is the incorrect use The University of Oklahoma Health of the device due to lack of training in how to use the device or how to coordinate actuation Sciences Center, Oklahoma City, and aerosol inhalation. This review summarizes the structural and mechanical features of OK, USA aerosol delivery devices with respect to mechanisms of aerosol generation, their use with different formulations, and their advantages and limitations. A technological update of the current state-of-the-art designs proposed to overcome current challenges of existing devices is also provided. Keywords: pulmonary delivery, asthma, nebulizers, metered dose inhaler, dry powder inhaler Introduction Inhalation therapy has been used for thousands of years, albeit in a different form and use. Inhalation therapy was practiced by ancient civilizations in Egypt, Greece, India, and People’s Republic of China as evidenced by different artifacts displayed in museums, that may be considered the first used inhalation devices.1,2 Currently, inhalation therapy is the best option for lung diseases like asthma, cystic fibrosis, and chronic obstructive pulmonary disease (COPD). -

Olodaterol Monograph
Olodaterol Monograph Olodaterol (Striverdi Respimat) National Drug Monograph VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechan Olodaterol is a long-acting beta2-adrenergic agonist (LABA). Binding to and activating ism of Action beta2-adrenoceptors in the airways results in stimulation of intracellular adenyl cyclase, an enzyme that mediates the synthesis of cyclic-3’, 5’ adenosine monophosphate (cAMP). Elevated levels of cAMP induce bronchodilation by relaxation of airway smooth muscle cells. Indication(s) Under Long-term once daily maintenance bronchodilator treatment of airflow obstruction in Review patients with COPD including chronic bronchitis and/or emphysema Dosage Form(s) Inhalation spray for oral inhalation via Respimat (a soft-mist inhaler) Under Review The soft-mist inhalers (SMI) provide multi-dose medication using liquid formulations similar to that used in nebulizers and are propellant-free. Presently, Respimat is the only SMI commercially available for clinical use. The soft mist is released at a slower velocity and has more prolonged spray duration than the mist produced from pressurized metered dose inhalers (pMDIs). Pressurized MDIs require coordination of actuation with inhalation which may be difficult for some patients partly due to the rapid speed at which the drug is delivered and the short duration of the mist. -

Preventive Drug List
navitus.com Share a Clear View Preventive Drug List Updated July 2021 Your health plan is making an effort to reduce your health care costs by giving you tools to help you stay healthy and productive. Below are the medications included on your Preventive Drug List. These medications help protect against or manage some high risk medical conditions. Taking these medications as directed by your prescriber can help avoid serious health problems. That may mean fewer doctor visits and hospitalizations, reducing your total health care costs. In the drug list below, generic drugs are shown in lowercase type. Brand name drugs are shown in uppercase type. Antiasthmatic/Bronchodilators theophylline soln ADVAIR DISKUS INHALER *generic Wixela only for wixela inhaler *brand Advair Diskus only for non-HDHP plans* HDHPs* ADVAIR HFA INHALER Anticoagulant albuterol/ipratropium neb soln ELIQUIS TAB aminophylline tab PRADAXA CAP ARNUITY ELLIPTA INHALER warfarin tab ASMANEX HFA INHALER XARELTO TAB ASMANEX INHALER Antidiabetics budesonide inh susp acarbose tab FLOVENT DISKUS INHALER chlorpropamide tab FLOVENT HFA INHALER glimepiride tab fluticasone/salmeterol inhaler glipizide ER tab ipratropium neb soln glipizide tab METAPROTERENOL SYRUP glipizide/metformin tab montelukast chew tab glyburide micronized tab montelukast tab glyburide tab THEOCHRON glyburide/metformin tab theophylline CR tab metformin ER tab theophylline ER tab metformin tab • Note: The list is subject to change and not all drugs listed may be covered on your formulary. Please refer to your Navitus -

Connecticut Medicaid
ACNE AGENTS, TOPICAL ‡ ANGIOTENSIN MODULATOR COMBINATIONS ANTICONVULSANTS, CONT. CONNECTICUT MEDICAID (STEP THERAPY CATEGORY) AMLODIPINE / BENAZEPRIL (ORAL) LAMOTRIGINE CHEW DISPERS TAB (not ODT) (ORAL) (DX CODE REQUIRED - DIFFERIN, EPIDUO and RETIN-A) AMLODIPINE / OLMESARTAN (ORAL) LAMOTRIGINE TABLET (IR) (not ER) (ORAL) Preferred Drug List (PDL) ACNE MEDICATION LOTION (BENZOYL PEROXIDE) (TOPICAL)AMLODIPINE / VALSARTAN (ORAL) LEVETIRACETAM SOLUTION, IR TABLET (not ER) (ORAL) • The Connecticut Medicaid Preferred Drug List (PDL) is a BENZOYL PEROXIDE CREAM, WASH (not FOAM) (TOPICAL) OXCARBAZEPINE TABLET (ORAL) listing of prescription products selected by the BENZOYL PEROXIDE 5% and 10% GEL (OTC) (TOPICAL) ANTHELMINTICS PHENOBARBITAL ELIXIR, TABLET (ORAL) Pharmaceutical and Therapeutics Committee as efficacious, BENZOYL PEROXIDE 6% CLEANSER (OTC) (TOPICAL) ALBENDAZOLE TABLET (ORAL) PHENYTOIN CHEW TABLET, SUSPENSION (ORAL) safe and cost effective choices when prescribing for HUSKY CLINDAMYCIN PH 1% PLEGET (TOPICAL) BILTRICIDE TABLET (ORAL) PHENYTOIN SOD EXT CAPSULE (ORAL) A, HUSKY C, HUSKY D, Tuberculosis (TB) and Family CLINDAMYCIN PH 1% SOLUTION (not GEL or LOTION) (TOPICAL)IVERMECTIN TABLET (ORAL) PRIMIDONE (ORAL) Planning (FAMPL) clients. CLINDAMYCIN / BENZOYL PEROXIDE 1.2%-5% (DUAC) (TOPICAL) SABRIL 500 MG POWDER PACK (ORAL) • Preferred or Non-preferred status only applies to DIFFERIN 0.1% CREAM (TOPICAL) (not OTC GEL) (DX CODE REQ.) ANTI-ALLERGENS, ORAL SABRIL TABLET (ORAL) those medications that fall within the drug classes DIFFERIN -

Smoking and Asthma
If you smoke and have asthma, the most important step you can take to improve your health and reduce asthma attacks is to QUIT SMOKING . Tobacco smoke is a major trigger for asthma attacks. Asthmatic breathing tube triggered by smoking Muscles tighten and squeeze tubes Extra mucus forms inside tubes Tubes swell and fill with fluid Asthmatic breathing tube Normal breathing tube Eight hours after your last cigarette, oxygen levels in your No matter blood return to normal. After 72 hours (3 days), breathing tubes relax, lung capacity how long increases, and breathing is easier. After 1 to 9 months, sinus congestion, coughing, fatigue, you smoked, and shortness of breath decrease. Your lungs’ ability to quitting helps clean themselves and handle mucus improves. Chances of lung infections are reduced. you b r e a t h e You’ll save trips to the doctor and ER and save money on asthma medication or possibly not buy it at all. more easily! You’ll save money from no longer buying cigarettes! TOBACCO CESSATION PROGRAM | 2600 TOWER DRIVE, SUITE 216, MONROE Tobacco smoke is the most toxic indoor Quitting smoking is difficult to do alone, air pollutant that triggers asthma. but support is available through your It is worse than dust mites, St. Francis Tobacco Cessation Program. cockroaches, and mold, and people with asthma should not smoke or be around secondhand smoke. Any time you need assistance WHAT HAPPENS WHEN with your cessation journey, need to ask questions YOU QUIT SMOKING or just need to talk, When a person who has asthma quits smok- call us at (318) 966-QUIT. -

Novel Therapeutic Approaches to Eosinophilic Esophagitis
Novel Therapeutic Approaches to Eosinophilic Esophagitis Claire Beveridge, MD, and Gary W. Falk, MD, MS Dr Beveridge is a gastroenterology Abstract: Eosinophilic esophagitis is a chronic inflammatory condi- and hepatology fellow and Dr Falk is a tion that requires treatment to improve symptoms and prevent professor of medicine in the Division complications of esophageal remodeling, such as strictures and of Gastroenterology and Hepatology narrow-caliber esophagus. First-line treatments include proton at the University of Pennsylvania Perelman School of Medicine in pump inhibitors, topical corticosteroids, elimination or elemental Philadelphia, Pennsylvania. diets, and esophageal dilation. Topical corticosteroids have typi- cally required repurposing inhaled asthma medications by swal- lowing an aerosolized medication or mixing a nebulizer solution Address correspondence to: into a slurry. New topical corticosteroid formulations undergoing Dr Gary W. Falk investigation include a premade budesonide oral suspension and Division of Gastroenterology and Hepatology disintegrating budesonide and fluticasone propionate tablets. The University of Pennsylvania Perelman approach to an elimination diet is also changing, with an emphasis School of Medicine on patient preference when considering a traditional 6-food elim- Perelman Center for Advanced ination diet compared with a step-up approach. This approach Medicine involves eliminating only 2 or 4 foods initially and expanding if 7th Floor South Pavilion 750 necessary. While this method can be initially less effective for some 3400 Civic Center Boulevard Philadelphia, PA 19104 patients, it generally involves fewer endoscopies and minimizes Tel: 215-615-4951 diet restriction. Beyond conventional therapies, a number of novel Fax: 215-349-5915 biologic agents are also under investigation. These include week- E-mail: gary.falk@pennmedicine. -

Using an Inhaler and Nebulizer
inhalercover.pdf 1 8/27/18 7:32 AM Using an Inhaler and Nebulizer C M Y CM MY CY CMY K Using an Inhaler and Nebulizer Inhalers An inhaler is a handheld device. It delivers medication directly into your airways. Inhalers are commonly used to treat problems that affect your ability to breathe. Your health care provider may recommend that you use an inhaler if you have: • Asthma. • Chronic obstructive pulmonary disease. • Other ongoing respiratory problems. The asthma medications delivered by the inhalers include: • Bronchodilators. • Steroids. • Combination of bronchodilators and steroids. Bronchodilators cause small airways in the lungs to open up. Steroids are used to relieve swelling and inflammation. Some inhalers are meant for limited use during an emergency situation. Others are used daily to prevent breathing problems. Using the right amount of medication is important in the treatment and prevention of ongoing respiratory problems. Medications can also decrease the sensitivity of the lungs to allergens. Inhalers are commonly used to deliver these medications directly into the airways. Inhaled medicine relieves symptoms faster than the same medicine given in pill form. Using an Inhaler and Nebulizer 1 Fewer side effects happen when medicine is delivered by an inhaler instead of taken in pill form. That’s because medicine from an inhaler goes directly into the airways. Very little medicine ends up in the bloodstream. Inhalers come in many different forms. The most commonly used inhalers are: • Metered dose inhalers. • Metered dose inhalers with a spacer. • Dry powder inhalers. A metered dose inhaler, or MDI, is a small aerosol canister that holds medicine.