Garis Panduan Kaunseling Ubat-Ubatan Edisi Ke-3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
List of New Drugs Approved in India from 1991 to 2000
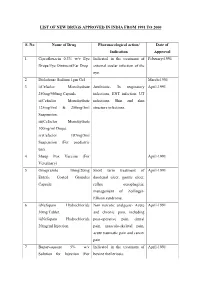
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -
Fixed Drug Eruption Due to a Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: a Case Report
ISSN: 2688-8238 DOI: 10.33552/OJOR.2020.04.000577 Online Journal of Otolaryngology and Rhinology Case Report Copyright © All rights are reserved by Akif İşlek Fixed Drug Eruption Due to A Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: A Case Report Akif İşlek1* and Engin Karaaslan2 1Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey 2Nusaybin State Hospital, Dermatology and Venereology, Mardin, Turkey *Corresponding author: Received Date: October 24, 2020 Published Date: November 03, 2020 Akif İşlek, Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey. Abstract Treatment of earwax often involves the use of a wax softening agent (cerumenolytic) with or without antimicrobial agents to easily removing. Cerumenolytic agents used to remove and soften earwax areoil-based treatments, water-based treatments. Fixed drug eruption (FDE) is a well- defined, circular, hyperpigmented plaque that usually occurs on the trunk, hands mucosal surfaces, after a systemical application of drugs. In this report, a case with FDE developed after a cerumenolytic agent (hydrogen peroxide and boric acid in water). A definitive diagnosis was made with skin punch biopsy and FDE was treated with oral levocetirizine and topical mometasone. Introduction is a well-defined, circular, hyper pigmenting plaque that usually Cerumen production is a normal and protective process occurs on the genitals, lips, trunk, and hands and the diagnosis for the external ear canal (EAC), but impact of cerumen causes can be confirmed by histopathologic examination of a small punch symptoms such as hearing loss, itching, pain, tinnitus [1]. Cerumen biopsy specimen [5]. In this report, a case with FDE developed after impaction is defined as an accumulation of cerumen in the a cerumenolytic agent (hydrogen peroxide and boric acid in water) external ear [2]. -
Inhalation Devices: Various Forms of Administration for Therapeutic Optimization
vv ISSN: 2640-8082 DOI: https://dx.doi.org/10.17352/oja CLINICAL GROUP Renata Cristina de Angelo Calsaverini Leal* Review Article Santa Fé do Sul Foundation of Education and Culture, Brazil Inhalation Devices: Various forms Dates: Received: 31 May, 2017; Accepted: 26 June, of administration for Therapeutic 2017; Published: 27 June, 2017 *Corresponding author: Renata Cristina de Angelo Optimization Calsaverini Leal, Santa Fé do Sul Foundation of Education and Culture, Brazil, Tel: 55 (17) 3272-2769, E-mail: Keywords: Inhalation; Aerosol; Nebulizer Summary https://www.peertechz.com Introduction: Aerosol therapy consists of spraying liquid particles suspended for therapeutic purposes in the respiratory tract. With direct absorption and deposition at the lung level, avoiding side effects and presenting fast response time. Several factors infl uence the drug action, such as size, particle movement, ventilatory fl ow, pulmonary expansion, anatomy, respiratory mechanics and the nebulizer and patient interface. The therapeutic optimization depends on the type of nebulizer differentiating itself by the physical principle that generates the mist. Objectives: Check advantages and disadvantages of different inhalation devices. Methodology. This is a review of the PubMed database using descriptors: ultrasonic and jet nebulizer, aerosol deposition in the lung, metered dose inhaler and dry, inhaler therapy. Results: Different devices are mentioned in the literature: pneumatic and ultrasonic nebulizers (administering solutions), metered pressurized inhalers - pMDI used with or without expander chamber (administering suspensions) and dry powder inhalers - DPI (administering powder). Discussion and Conclusion: The US has advantages: quiet, does not require coordinating abilities, without propellant gases and quick nebulization with small amount of solution. Disadvantages: change in the active principle of thermosensitive drugs, deposition in the oropharynx and VAI of 2% of inhaled particles. -

Inhaled Steroids in Asthma a Patient's Guide
I I v v v v d v v Patient advice and liaison service (PALS) Actions r v If you have a compliment, complaint or It is sensible to ensure you make the r concern please contact our PALS team on following steps now you have a new r 020 7288 5551 or inhaler d [email protected] d d Pick up our guide on inhalers and If you need a large print, audio or spacers to complement this leaflet translated copy of this leaflet please Inhaled Steroids in Agree on a personalised asthma contact us on 020 7288 3182. We will try plan (this is done with your doctor or our best to meet your needs. Asthma nurse and usually written down for future reference) Remember to take your medicines A patient’s guide as advised Should your inhalers fail to relieve your symptoms, go straight to Accident and Emergency Need Help? Whittington Paediatric Asthma Nurse Tel: 020 7288 5527 Whittington Health Community Nurse Magdala Avenue Islington 020 3316 1950 (8am-6pm) London N19 5NF Haringey 020 8887 3301 (9am – 5pm) Phone: 020 7272 3070 www.whittington.nhs.uk Asthma UK 0300 222 5800 Date published: 25/09/2018 www.asthma.org.uk Review date: 25/09/2020 Ref: C&YP/Paed/ISA/03 © Whittington Health Please recycle Tel: 020 7272 3070 Asthma There are many types of preventer Side Effects Asthma is a common condition affecting inhaler. There are simple steroids like Parents worry about children and young the airway. Usually a trigger (such as dust beclomethasone, and then there are also adults taking inhaled steroids because of or pollen) irritates the airways which combined inhalers, called seretide or side effects they’ve heard about. -

Member List 2016
To help make the use of prescription drugs safer and more affordable, our plan is now using a Drug Quantity Management program. That is, for certain medications, you can receive an amount to last you a certain number of days. This gives you the right amount to take the daily dose considered safe and effective, according to the recommendations of the U.S. Food and Drug Administration (FDA). Based on the FDA’s guidelines and other medical information, our plan developed this program together with Express Scripts, the company chosen to manage our prescription drug benefit. The following limits are based on a 30-day supply. If your plan allows for additional days supply, your limits may be higher. For instance, you may be able to get a 90-day supply of your medication through mail order service. Your doctor could also request a prior authorization. If this request is approved, a prior authorization would let you receive more than the recommended quantity. Drug Target Maximum Quantity ABSTRAL 100 MCG TAB SUBLINGUAL 90 units per 30 days ABSTRAL 200 MCG TAB SUBLINGUAL 90 units per 30 days ABSTRAL 300 MCG TAB SUBLINGUAL 90 units per 30 days ABSTRAL 400 MCG TAB SUBLINGUAL 90 units per 30 days ABSTRAL 600 MCG TAB SUBLINGUAL 90 units per 30 days ABSTRAL 800 MCG TAB SUBLINGUAL 90 units per 30 days ACTIQ 1,200 MCG LOZENGE 90 units per 30 days ACTIQ 1,600 MCG LOZENGE 90 units per 30 days ACTIQ 200 MCG LOZENGE 90 units per 30 days ACTIQ 400 MCG LOZENGE 90 units per 30 days ACTIQ 600 MCG LOZENGE 90 units per 30 days ACTIQ 800 MCG LOZENGE 90 units per -

Common Ear, Nose & Throat Problems
Common Ear, Nose & Throat Problems The information provided in this presentation is not intended to guide treatment or aid in making a diagnosis. Always consult a physician or nurse practitioner. Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Normal Larynx Normal larynx in a 44 yr old non-smoker Go to http://www.entusa.com/normal_larynx.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Acute Laryngitis This video shows the function of the larynx in a 24 yr old patient with acute laryngitis. Talking was painful and she only talked in a faint whisper. Go to http://www.entusa.com/laryngitis.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Paralysis This video shows the function of a larynx with a paralyzed left true vocal cord. The patient has lung cancer. She has a poorly compensated breathy voice which is difficult to understand. This patient had a 55 pack year history of smoking. Go to http://www.entusa.com/vocal_cord_paralysis_2.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Polyp This video shows the function of a larynx with a vocal cord polyp on the right true vocal cord. This patient smoked one pack a day for 30 years. Go to http://www.entusa.com/larynx_polyp-9.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Laryngeal Cancer This video shows the function of a larynx with a large T1b Cancer on both true vocal cords and anterior commissure in 72 yr old male with a 150 pack year history of smoking. -
EAR, NOSE and OROPHARYNX Updated: October 2020
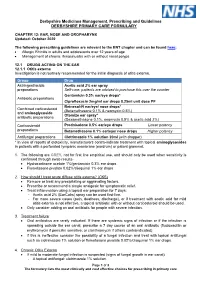
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

10/15-Hour Medication Test Answers
Appendix 10/15-Hour Medication Test Answers Name _________________________________ Facility _________________________________ Part 1: Match the term or phrase on the right with the abbreviation or term on the left by placing the correct letter on the appropriate line. _____ 1. PRN (p) a. milligram _____ 2. ac (e) b. at bedtime _____ 3. stat (j) c. Medication Administration Record _____ 4. SL (k) d. over the counter _____ 5. MAR (c) e. before meals _____ 6. mg (a) f. tablespoonful _____ 7. pc (m) g. placed and affixed to the skin _____ 8. OTC (d) h. teaspoonful _____ 9. Subcutaneous (r) i. milliliter _____ 10. po (n) j. immediately _____ 11. qhs (b) k. sublingual _____ 12. tbsp (f) l. placed under the tongue _____ 13. transdermal (g) m. after meals _____ 14. ml (i) n. by mouth _____ 15. gm (o) o. gram _____ 16. QOD (q) p. as needed _____ 17. tsp (h) q. every other day _____ 18. sublingual (l) r. inject into the fat with a syringe Medication Administration – March 2021 10/15-Hour Training Course for Adult Care Homes 4 Appendix 10/15-Hour Medication Test Answers – Continued Part 2: Fill in the blank with the appropriate word or term. You may choose to use the word bank below. 19. A heart tablet taken by mouth and swallowed is an example of a medication taken by the oral route. 20. A medication that is inserted into the rectum is given using the rectal route. 21. A topical medication is applied directly to the skin surface. -

Drugs That Are Not Covered
Drugs that are Not Covered* Current 10/1/21 In addition to this list, newly marketed prescription medications may not be covered until the Pharmacy & Therapeutics Committee has had an opportunity to review the medication, to determine whether the medication will be covered and if so, which tier will apply based on safety, efficacy and the availability of other products within that class of medications. The current list of newly marketed drugs can be found on our New to Market Drug list. Abilify tablets albuterol HFA inhalers (authorized Apexicon E cream Abilify MyCite tablets generics for ProAir, Proventil, Ventolin Apidra vials Absorica capsules HFA inhalers) Apidra SoloStar injection Absorica LD capsules Aldactone tablets Aplenzin tablets Abstral sublingual tablets Aldara cream Apriso capsules Acanya gel and pump gel Alkindi sprinkle capsules Arava tablets Accupril tablets Allegra Children’s Allergy ODT Arazlo lotion acetaminophen 320.5 mg/caffeine 30 Allegra ODT, suspension and tablets Arestin microspheres mg/dihydrocodeine 16 mg Alltizal tablets Aricept tablets capsulesAciphex tablets alogliptin (authorized generic for Aricept ODT Aciphex Sprinkle capsules Nesina) Arimidex tablets Acticlate tablets alogliptin/metformin tablets (authorized Arixtra injection Active-Prep kits generic for Kazano) ArmonAir Digihaler inhaler Activella tablets alogliptin/pioglitazone (authorized ArmonAir Respiclick inhaler Actonel tablets generic for Oseni) Aromasin tablets Actoplus Met tablets Alphagan P 0.1% eye drops Arthrotec 50 and 75 tablets Actos -

L092 Session: L168 Thoracic Epidural Analgesia in the Re
Session: L092 Session: L168 Thoracic Epidural Analgesia in the Recently Anticoagulated Patient: Is This a Good Idea? Anuj Malhotra, M.D. Icahn School of Medicine at Mount Sinai, New York, NY Disclosures: This presenter has no financial relationships with commercial interests Stem Case and Key Questions Content A 52 year old male presents for open resection for colon cancer. He has had multiple prior abdominal surgeries and the planned approach is a supraumbilical midline incision that will cover the T6-T10 dermatomes. The patient is obese and has a history of COPD. Vitals: HR 70, BP 126/68, O2 sat 95% on RA, Ht 6'0", Wt 285 lbs 1) What surgical features and patient factors make this patient a good candidate for a thoracic epidural? 2) What level should this block be placed at? Should it be placed paramedian or midline? What should be infused? 3) Does it matter if the epidural is activated before surgery (pre-emptive analgesia) or after? What are the pros and cons of early dosing? The patient also has chronic abdominal pain treated with methadone 10 mg three times daily and oxycodone 5-10 mg four times daily. He is very concerned about difficulty with extubation, postoperative pain, and ileus. Medications: Methadone 10 mg tid, oxycodone 5-10 mg q 6 hrs prn, albuterol inhaler prn, fluticasone/salmeterol inhaler bid, metoprolol XL 50 mg daily ECG: irregularly irregular @ 70 bpm, QTc 440 ms 4) What patient characteristics suggest the need for postoperative pain control? Will thoracic epidural analgesia decrease ileus? Will it shorten duration of postoperative mechanical ventilation? 5) Does thoracic epidural analgesia affect long-term outcomes such as mortality or chronic postoperative pain? 6) Should his methadone be continued perioperatively if he has a neuraxial block for pain control? Upon reviewing the ECG and questioning the patient further, he reports a recent diagnosis of atrial fibrillation for which he takes dabigatran 150 mg bid for stroke prevention. -

Medication Administration
MEDICATION ADMINISTRATION GENERAL CONSIDERATIONS A. Before administering any medication, the EMT should know: 1. What is the medication being used? 2. Does the patient have an allergy to this medication? 3. What is the safe and effective dose? 4. What is the correct administration route? 5. What are the indications? (Why are you using is?) 6. What are the contraindications? (Why or when would you NOT use this medication?) 7. What are the expected effects? 8. What are the adverse effects / side effects? 9. Is the medication expired? B. The “Six Rights” of medication administration: 1. Right patient – is the medication indicated for this patient; no contraindications; no allergies 2. Right drug – the correct name (trade name vs. generic name); correct concentration 3. Right dose 4. Right route 5. Right time – slow IVP vs. rapid IVP 6. Right documentation C. Correct documentation of medications administered and/or IV/IO placement will include: 1. Time of medication administration; IV/IO placement 2. Route of administration 3. Size of catheter (IV/IO) 4. Site location for IV/IO and SQ, IM medication (include unsuccessful IV/IO attempt locations) 5. Dose or volume infused 6. Time of infusion as indicated (e.g., rapid IVP, infused over 10 minutes, etc.) 7. Name of EMT responsible 8. Any complications and steps made to correct 9. Patient’s response to treatment D. Use of a medication simply because it is in the protocol is not an acceptable standard of medical care. When there are questions about medication administration, consult medical control. ORAL ADMINSTRATION To administer an oral (PO) medication ensure that the patient has an intact gag reflex and place the patient in a seated or semi-seated position. -
A Guide to Aerosol Delivery Devices for Respiratory Therapists 4Th Edition
A Guide To Aerosol Delivery Devices for Respiratory Therapists 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC Platinum Sponsor Copyright ©2017 by the American Association for Respiratory Care A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC With a Foreword by Timothy R. Myers, MBA, RRT-NPS, FAARC Chief Business Officer American Association for Respiratory Care DISCLOSURE Douglas S. Gardenhire, EdD, RRT-NPS, FAARC has served as a consultant for the following companies: Westmed, Inc. and Boehringer Ingelheim. Produced by the American Association for Respiratory Care 2 A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition American Association for Respiratory Care, © 2017 Foreward Aerosol therapy is considered to be one of the corner- any) benefit from their prescribed metered-dose inhalers, stones of respiratory therapy that exemplifies the nuances dry-powder inhalers, and nebulizers simply because they are of both the art and science of 21st century medicine. As not adequately trained or evaluated on their proper use. respiratory therapists are the only health care providers The combination of the right medication and the most who receive extensive formal education and who are tested optimal delivery device with the patient’s cognitive and for competency in aerosol therapy, the ability to manage physical abilities is the critical juncture where science inter- patients with both acute and chronic respiratory disease as sects with art.