Anthropometric Study of the Pectoralis Minor Muscle As a Power Source To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thoracic Outlet and Pectoralis Minor Syndromes
S EMINARS IN V ASCULAR S URGERY 27 (2014) 86– 117 Available online at www.sciencedirect.com www.elsevier.com/locate/semvascsurg Thoracic outlet and pectoralis minor syndromes n Richard J. Sanders, MD , and Stephen J. Annest, MD Presbyterian/St. Luke's Medical Center, 1719 Gilpin, Denver, CO 80218 article info abstract Compression of the neurovascular bundle to the upper extremity can occur above or below the clavicle; thoracic outlet syndrome (TOS) is above the clavicle and pectoralis minor syndrome is below. More than 90% of cases involve the brachial plexus, 5% involve venous obstruction, and 1% are associate with arterial obstruction. The clinical presentation, including symptoms, physical examination, pathology, etiology, and treatment differences among neurogenic, venous, and arterial TOS syndromes. This review details the diagnostic testing required to differentiate among the associated conditions and recommends appropriate medical or surgical treatment for each compression syndrome. The long- term outcomes of patients with TOS and pectoralis minor syndrome also vary and depend on duration of symptoms before initiation of physical therapy and surgical intervention. Overall, it can be expected that 480% of patients with these compression syndromes can experience functional improvement of their upper extremity; higher for arterial and venous TOS than for neurogenic compression. & 2015 Published by Elsevier Inc. 1. Introduction compression giving rise to neurogenic TOS (NTOS) and/or neurogenic PMS (NPMS). Much less common is subclavian Compression of the neurovascular bundle of the upper and axillary vein obstruction giving rise to venous TOS (VTOS) extremity can occur above or below the clavicle. Above the or venous PMS (VPMS). -

Thoracic Outlet Syndrome of Pectoralis Minor Etiology Mimicking Cardiac
0008-3194/2012/311–315/$2.00/©JCCA 2012 Thoracic outlet syndrome of pectoralis minor etiology mimicking cardiac symptoms on activity: a case report Gary Fitzgerald BSc(NUI), BSc(Hons)(Chiro), MSc(Chiro), ICSSD* Thoracic outlet syndrome is the result of compression Le syndrome de la traversée thoracobrachial est le or irritation of neurovascular bundles as they pass résultat de la compression ou de l’irritation d’un from the lower cervical spine into the arm, via the paquet vasculonerveux au cours de son trajet entre axilla. If the pectoralis minor muscle is involved the la colonne cervicale inférieure et le bras, en passant patient may present with chest pain, along with pain par l’aisselle. Si le muscle petit pectoral est sollicité, and paraesthesia into the arm. These symptoms are also le patient peut subir de la douleur à la poitrine ainsi commonly seen in patients with chest pain of a cardiac que de la douleur et de la paresthésie dans le bras. origin. In this case, a patient presents with a history of On voit souvent ces symptômes aussi chez des patients left sided chest pain with pain and paraesthesia into the souffrant de douleurs thoraciques d’origine cardiaque. left upper limb, which only occurs whilst running. The Dans de tels cas, le patient présente des antécédents de symptoms were reproduced on both digital pressure over douleurs thoraciques du côté gauche, accompagnées the pectoralis minor muscle and on provocative testing de douleur et de paresthésie dans le membre supérieur for thoracic outlet syndrome. The patient’s treatment gauche, qui survient uniquement pendant que le patient therefore focused on the pectoralis minor muscle, with court. -

Pectoral Region and Axilla Doctors Notes Notes/Extra Explanation Editing File Objectives
Color Code Important Pectoral Region and Axilla Doctors Notes Notes/Extra explanation Editing File Objectives By the end of the lecture the students should be able to : Identify and describe the muscles of the pectoral region. I. Pectoralis major. II. Pectoralis minor. III. Subclavius. IV. Serratus anterior. Describe and demonstrate the boundaries and contents of the axilla. Describe the formation of the brachial plexus and its branches. The movements of the upper limb Note: differentiate between the different regions Flexion & extension of Flexion & extension of Flexion & extension of wrist = hand elbow = forearm shoulder = arm = humerus I. Pectoralis Major Origin 2 heads Clavicular head: From Medial ½ of the front of the clavicle. Sternocostal head: From; Sternum. Upper 6 costal cartilages. Aponeurosis of the external oblique muscle. Insertion Lateral lip of bicipital groove (humerus)* Costal cartilage (hyaline Nerve Supply Medial & lateral pectoral nerves. cartilage that connects the ribs to the sternum) Action Adduction and medial rotation of the arm. Recall what we took in foundation: Only the clavicular head helps in flexion of arm Muscles are attached to bones / (shoulder). ligaments / cartilage by 1) tendons * 3 muscles are attached at the bicipital groove: 2) aponeurosis Latissimus dorsi, pectoral major, teres major 3) raphe Extra Extra picture for understanding II. Pectoralis Minor Origin From 3rd ,4th, & 5th ribs close to their costal cartilages. Insertion Coracoid process (scapula)* 3 Nerve Supply Medial pectoral nerve. 4 Action 1. Depression of the shoulder. 5 2. Draw the ribs upward and outwards during deep inspiration. *Don’t confuse the coracoid process on the scapula with the coronoid process on the ulna Extra III. -
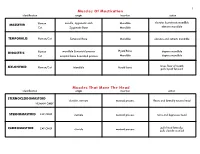
Muscles of Mastication Muscles That Move the Head
1 Muscles Of Mastication identification origin insertion action maxilla, zygomatic arch Mandible elevates & protracts mandible MASSETER Human Cat Zygomatic Bone Mandible elevates mandible TEMPORALIS Human/Cat Temporal Bone Mandible elevates and retracts mandible Hyoid Bone DIGASTRIC Human mandible & mastoid process depress mandible Cat occipital bone & mastoid process Mandible depress mandible raises floor of mouth; MYLOHYOID Human/Cat Mandible Hyoid bone pulls hyoid forward Muscles That Move The Head identification origin insertion action STERNOCLEIDOMAStoID clavicle, sternum mastoid process flexes and laterally rotates head HUMAN ONLY STERNOMAStoID CAT ONLY sternum mastoid process turns and depresses head pulls head laterally; CLEIDOMAStoID CAT ONLY clavicle mastoid process pulls clavicle craniad 2 Muscles Of The Hyoid, Larynx And Tongue identification origin insertion action Human Sternum Hyoid depresses hyoid bone STERNOHYOID Cat costal cartilage 1st rib Hyoid pulls hyoid caudally; raises ribs and sternum sternum Throid cartilage of larynx Human depresses thyroid cartilage STERNothYROID Cat costal cartilage 1st rib Throid cartilage of larynx pulls larynx caudad elevates thyroid cartilage and Human thyroid cartilage of larynx Hyoid THYROHYOID depresses hyoid bone Cat thyroid cartilage of larynx Hyoid raises larynx GENIOHYOID Human/Cat Mandible Hyoid pulls hyoid craniad 3 Muscles That Attach Pectoral Appendages To Vertebral Column identification origin insertion action Human Occipital bone; Thoracic and Cervical raises clavicle; adducts, -

Congenital Absence of the Pectoral Muscles
Arch Dis Child: first published as 10.1136/adc.12.68.123 on 1 April 1937. Downloaded from CONGENITAL ABSENCE OF THE PECTORAL MUSCLES BY E. D. IRVINE, M.D., AND J. B. TILLEY, M.D. (Blackburn). The four patients described in this paper exhibit congenital absence of the pectoral muscles in varying degree, and illustrate many points of interest. Three of them were observed during routine and special medical examinations of approximately 15,000 elementary school children, and one was a pre-school child in hospital: it is interesting to note that Scheslinger, according to Rector', discovered five cases in 54,000 patients. Case 1 was discovered during the examination of a boy aged ten, the second of four children, who complained of cough: he is under observation http://adc.bmj.com/ on September 30, 2021 by guest. Protected copyright. FIG. 1. as a tuberculosis contact. The sterno-costal portion of the left pectoralis major and the left pectoralis minor are both missing. Although not previously noted, this is believed to be a congenital defect. The clavicular head of the pectoralis major is well developed and arises from the inner half of the clavicle; the deltoid is not hypertrophied (fig. 1). When the arms are extended above the head, a well-marked fold of skin running vertically across the axilla to the second left rib and interspace can be seen and in Arch Dis Child: first published as 10.1136/adc.12.68.123 on 1 April 1937. Downloaded from I 2d4 AIICIlIVES 0O' DISEASE IN CHILDHOOD the fold fibrous tissue can be felt deep to the skin: whether this is simply fascia or a vestigial or degenerated muscle is not known. -

Isolated Tears of Pectoralis Minor Muscle in Professional Football Players: a Case Series John E
(aspects of sports medicine) Isolated Tears of Pectoralis Minor Muscle in Professional Football Players: A Case Series John E. Zvijac, MD, Bashir Zikria, MD, and Angie Botto-van Bemden, PhD ABSTRACT ciae covering the intercostals, passing sent mechanisms of injury, clinical Our objective is to include pectoralis superiorly and laterally to insert on presentations, appropriate diagnostic minor injuries in the comprehensive the coracoid process of the scapula. studies, and treatments. assessment of differential diagnoses It provides an anatomical landmark for anterior chest wall pain or medi- for deeper structures, specifically MATERIALS AND METHODS al anterior shoulder pain sustained the axillary artery, the medial pec- during blocking activities, which Case 1 may present in football players. toral nerve, and the brachial plexus A right-hand–dominant man in his In this article, we report 2 cases cords. The pectoralis minor origin late 20s presented with pain in the of isolated pectoralis minor tears and insertion are subject to variation.6 anterior region of the left shoulder in professional football players and The pectoralis minor action includes just inferior to the clavicle. The present mechanisms of injury, clini- protraction and depression of the lat- patient was a fullback in the US cal presentations, appropriate diag- eral angle of the scapula. National Football League (NFL). nostic studies, and treatments. A multitude of differential diagno- His injury initially occurred during ses may be considered when athletes practice; when performing blocking ith individuals’ present with anterior chest wall pain. drills, he experienced increasing increasing participa- Our objective is to include pectoralis pain in the left shoulder and chest. -

Sonographic Tracking of Trunk Nerves: Essential for Ultrasound-Guided Pain Management and Research
Journal name: Journal of Pain Research Article Designation: Perspectives Year: 2017 Volume: 10 Journal of Pain Research Dovepress Running head verso: Chang et al Running head recto: Sonographic tracking of trunk nerve open access to scientific and medical research DOI: http://dx.doi.org/10.2147/JPR.S123828 Open Access Full Text Article PERSPECTIVES Sonographic tracking of trunk nerves: essential for ultrasound-guided pain management and research Ke-Vin Chang1,2 Abstract: Delineation of architecture of peripheral nerves can be successfully achieved by Chih-Peng Lin2,3 high-resolution ultrasound (US), which is essential for US-guided pain management. There Chia-Shiang Lin4,5 are numerous musculoskeletal pain syndromes involving the trunk nerves necessitating US for Wei-Ting Wu1 evaluation and guided interventions. The most common peripheral nerve disorders at the trunk Manoj K Karmakar6 region include thoracic outlet syndrome (brachial plexus), scapular winging (long thoracic nerve), interscapular pain (dorsal scapular nerve), and lumbar facet joint syndrome (medial branches Levent Özçakar7 of spinal nerves). Until now, there is no single article systematically summarizing the anatomy, 1 Department of Physical Medicine sonographic pictures, and video demonstration of scanning techniques regarding trunk nerves. and Rehabilitation, National Taiwan University Hospital, Bei-Hu Branch, In this review, the authors have incorporated serial figures of transducer placement, US images, Taipei, Taiwan; 2National Taiwan and videos for scanning the nerves in the trunk region and hope this paper helps physicians University College of Medicine, familiarize themselves with nerve sonoanatomy and further apply this technique for US-guided Taipei, Taiwan; 3Department of Anesthesiology, National Taiwan pain medicine and research. -

A Detailed Review on the Clinical Anatomy of the Pectoralis Major Muscle
SMGr up Review Article SM Journal of A Detailed Review on the Clinical Clinical Anatomy Anatomy of the Pectoralis Major Muscle Alexey Larionov, Peter Yotovski and Luis Filgueira* University of Fribourg, Faculty of Science and Medicine, Switzerland Article Information Abstract Received date: Aug 25, 2018 The pectoralis major is a muscle of the upper limb girdle. This muscle has a unique morphological Accepted date: Sep 07, 2018 architectonic and a high rate of clinical applications. However, there is lack of data regarding the morphological and functional interactions of the pectoralis major with other muscle and fascial compartments. According to the Published date: Sep 12, 2018 applied knowledge, the “Humero-pectoral” morpho-functional concept has been postulated. The purpose of this review was the dissectible investigation of the muscle anatomy and literature review of surgical applications. *Corresponding author Luis Filgueira, University of Fribourg, General Anatomy Faculty of Science and Medicine,1 Albert Gockel, CH-1700 Fribourg, Switzerland, The pectoralis major is a large, flat muscle of the pectoral girdle of the upper limb. It has a fan- Tel: +41 26 300 8441; shaped appearance with three heads or portions: the clavicular, the sternocostal and the abdominal Email: [email protected] head. Distributed under Creative Commons The clavicular head originates from the medial two-thirds of the clavicle (collar bone). The muscle fibers of the clavicular head have a broad origin on the caudal-anterior and caudal-posterior surface CC-BY 4.0 of the clavicle covering approximately half to two-thirds of that surface and converting toward the humerus, resulting in a triangular shape [1]. -

Chapter 10 *Lecture Powerpoint
Chapter 10 *Lecture PowerPoint The Muscular System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Facts about muscles – Muscles constitute nearly half of the body’s weight and occupy a place of central interest in several fields of health care and fitness • Physical and occupational therapy, athletes, dancers, trainers, acrobats, nurses, and more – Muscular system is closely related to other systems covered previously – Chapters 11 and 12 will examine the mechanisms of muscle contraction at the cellular and molecular levels 10-2 Introduction • In this chapter we will cover: – Structural and functional organization of muscles – Muscles of the head and neck – Muscles of the trunk – Muscles acting on the shoulder and upper limb – Muscles acting on the hip and lower limb Figure 10.5 10-3 The Structural and Functional Organization of Muscles • Expected Learning Outcomes – Describe the varied functions of muscles. – Describe the connective tissue components of a muscle and their relationship to the bundling of muscle fibers. – Describe the various shapes of skeletal muscles and relate this to their functions. – Explain what is meant by the origin, insertion, belly, action, and innervation of a muscle. 10-4 The Structural and Functional Organization of Muscles Cont. – Describe the ways that muscles work in groups to aid, oppose, or moderate each other’s actions. – Distinguish between intrinsic and extrinsic muscles. – Describe in general terms the nerve supply to the muscles and where these nerves originate. – Explain how the Latin names of muscles can aid in visualizing and remembering them. -

Thoracic Radiology Mount Sinai
Michael Chung, MD Assistant Professor Cardiothoracic Radiology Mount Sinai World Congress of Thoracic Imaging June 2017 Disclosures There are no disclosures pertinent to this presentation Mount Sinai Department of Radiology Introduction • The chest wall muscular anatomy is an aspect of chest CT that can be often overlooked by the cardiothoracic radiologist • Goals: • Review the normal chest wall anatomy on CT • Highlight the common normal variations in chest wall anatomy and shape • Focus on a few conditions which may distort the normal anatomy • Review common chest wall surgeries, including their indications and imaging appearance on CT Mount Sinai Department of Radiology 16 1 8 / 4 14 15 9 11 KEY: NOTES: 1. Pectoralis major 10. Long Head of Triceps • Sternocleidomastoid (16) 2. Pectoralis minor 11. Deltoid • Divides neck into anterior and posterior triangles 3. Subscapularis 12. Serratus Anterior • Will often see a portion of the SCM as it attaches to its 4. Teres Major 13. Rhomboid origin on the manubrium 5. Teres Minor 14. Erector Spinae 6. Supraspinatus 15. Levator Scapulae • Platysma 7. Infraspinatus 16. Sternocleidomastoid • Not visualized here, but can be seen on chest CTs as a 8. Latissimus Dorsi 17. Rectus Abdominis broad sheet of thin muscle covering the anterior neck 9. Trapezius Mount Sinai Department of Radiology 1 8 / 4 14 15 11 13 9 NOTES: KEY: 1. Pectoralis major 10. Long Head of Triceps • Deltoid (11) 2. Pectoralis minor 11. Deltoid • Largest shoulder muscle, will commonly see on chest 3. Subscapularis 12. Serratus Anterior CTs with patient’s arms elevated 4. Teres Major 13. Rhomboid • Innervated by the axillary nerve (C5-6) 5. -

Anatomy Module 3. Muscles. Materials for Colloquium Preparation
Section 3. Muscles 1 Trapezius muscle functions (m. trapezius): brings the scapula to the vertebral column when the scapulae are stable extends the neck, which is the motion of bending the neck straight back work as auxiliary respiratory muscles extends lumbar spine when unilateral contraction - slightly rotates face in the opposite direction 2 Functions of the latissimus dorsi muscle (m. latissimus dorsi): flexes the shoulder extends the shoulder rotates the shoulder inwards (internal rotation) adducts the arm to the body pulls up the body to the arms 3 Levator scapula functions (m. levator scapulae): takes part in breathing when the spine is fixed, levator scapulae elevates the scapula and rotates its inferior angle medially when the shoulder is fixed, levator scapula flexes to the same side the cervical spine rotates the arm inwards rotates the arm outward 4 Minor and major rhomboid muscles function: (mm. rhomboidei major et minor) take part in breathing retract the scapula, pulling it towards the vertebral column, while moving it upward bend the head to the same side as the acting muscle tilt the head in the opposite direction adducts the arm 5 Serratus posterior superior muscle function (m. serratus posterior superior): brings the ribs closer to the scapula lift the arm depresses the arm tilts the spine column to its' side elevates ribs 6 Serratus posterior inferior muscle function (m. serratus posterior inferior): elevates the ribs depresses the ribs lift the shoulder depresses the shoulder tilts the spine column to its' side 7 Latissimus dorsi muscle functions (m. latissimus dorsi): depresses lifted arm takes part in breathing (auxiliary respiratory muscle) flexes the shoulder rotates the arm outward rotates the arm inwards 8 Sources of muscle development are: sclerotome dermatome truncal myotomes gill arches mesenchyme cephalic myotomes 9 Muscle work can be: addacting overcoming ceding restraining deflecting 10 Intrinsic back muscles (autochthonous) are: minor and major rhomboid muscles (mm. -

Chest Wall Anatomy
CHEST WALL ANATOMY & MEDIASTINUM Luca Novelli, MD Physician – Pulmonary Medicine Unit Papa Giovanni XXIII Hospital, Bergamo, IT Sternum consists of the manubrium sterni, the corpus sterni, and the processus xiphoideus The sternum and cartilage of ribs 1–10 represent the anterior chest wall. The posterior part consists of 12 thoracic vertebrae and the posterior aspects of ribs 1–12. Laterally the chest cavity consists of ribs 1–12 Free ribs (11th and 12th) The RIBS are divided into 1. real ribs (costae verae, 1–7) that have sternal joints 2. false ribs (costae spuriae, 8–10) with cartilagenous joints to the costal arch (arcus costalis) 3. free ribs (costae fluctuantes, 11–12) that end in the soft tissue of the lateral chest wall. The 12th rib is not always present. The ribs move upwards during inspiration around their rib neck and downwards during expiration as well as by the interactions between the cartilage, sternum, and costal arch. The ribs move upwards during inspiration around their rib neck and downwards during expiration as well as by the interactions between the cartilage, sternum, and costal arch. Pectus Excavatum It is the most common congenital abnormalities of chest wall. It is characterized by prominent indentation of the lower sternum, which is usually asymmetric to the right, and resulting decrease in AP diameter of the rib cage. The mean pectus index in a normal population is around 2.56. Haller index is 3.7 (272.4/74.1) Pectus Carinatum In contrast to pectus excavatum, pectus carinatum is an outward protrusion of the sternum resulting in increased AP diameter of the thorax.