Chapter 10 *Lecture Powerpoint
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anatomy of the Rectum and Anal Canal
BASIC SCIENCE identify the rectosigmoid junction with confidence at operation. The anatomy of the rectum The rectosigmoid junction usually lies approximately 6 cm below the level of the sacral promontory. Approached from the distal and anal canal end, however, as when performing a rigid or flexible sigmoid- oscopy, the rectosigmoid junction is seen to be 14e18 cm from Vishy Mahadevan the anal verge, and 18 cm is usually taken as the measurement for audit purposes. The rectum in the adult measures 10e14 cm in length. Abstract Diseases of the rectum and anal canal, both benign and malignant, Relationship of the peritoneum to the rectum account for a very large part of colorectal surgical practice in the UK. Unlike the transverse colon and sigmoid colon, the rectum lacks This article emphasizes the surgically-relevant aspects of the anatomy a mesentery (Figure 1). The posterior aspect of the rectum is thus of the rectum and anal canal. entirely free of a peritoneal covering. In this respect the rectum resembles the ascending and descending segments of the colon, Keywords Anal cushions; inferior hypogastric plexus; internal and and all of these segments may be therefore be spoken of as external anal sphincters; lymphatic drainage of rectum and anal canal; retroperitoneal. The precise relationship of the peritoneum to the mesorectum; perineum; rectal blood supply rectum is as follows: the upper third of the rectum is covered by peritoneum on its anterior and lateral surfaces; the middle third of the rectum is covered by peritoneum only on its anterior 1 The rectum is the direct continuation of the sigmoid colon and surface while the lower third of the rectum is below the level of commences in front of the body of the third sacral vertebra. -

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

Thoracic Outlet and Pectoralis Minor Syndromes
S EMINARS IN V ASCULAR S URGERY 27 (2014) 86– 117 Available online at www.sciencedirect.com www.elsevier.com/locate/semvascsurg Thoracic outlet and pectoralis minor syndromes n Richard J. Sanders, MD , and Stephen J. Annest, MD Presbyterian/St. Luke's Medical Center, 1719 Gilpin, Denver, CO 80218 article info abstract Compression of the neurovascular bundle to the upper extremity can occur above or below the clavicle; thoracic outlet syndrome (TOS) is above the clavicle and pectoralis minor syndrome is below. More than 90% of cases involve the brachial plexus, 5% involve venous obstruction, and 1% are associate with arterial obstruction. The clinical presentation, including symptoms, physical examination, pathology, etiology, and treatment differences among neurogenic, venous, and arterial TOS syndromes. This review details the diagnostic testing required to differentiate among the associated conditions and recommends appropriate medical or surgical treatment for each compression syndrome. The long- term outcomes of patients with TOS and pectoralis minor syndrome also vary and depend on duration of symptoms before initiation of physical therapy and surgical intervention. Overall, it can be expected that 480% of patients with these compression syndromes can experience functional improvement of their upper extremity; higher for arterial and venous TOS than for neurogenic compression. & 2015 Published by Elsevier Inc. 1. Introduction compression giving rise to neurogenic TOS (NTOS) and/or neurogenic PMS (NPMS). Much less common is subclavian Compression of the neurovascular bundle of the upper and axillary vein obstruction giving rise to venous TOS (VTOS) extremity can occur above or below the clavicle. Above the or venous PMS (VPMS). -

By Dr.Ahmed Salman Assistant Professorofanatomy &Embryology My Advice to You Is to Focus on the Diagrams That I Drew
The University Of Jordan Faculty Of Medicine REPRODUCTIVE SYSTEM By Dr.Ahmed Salman Assistant ProfessorofAnatomy &embryology My advice to you is to focus on the diagrams that I drew. These diagrams cover the Edited by Dana Hamo doctor’s ENTIRE EXPLANATION AND WHAT HE HAS MENTIONED Quick Recall : Pelvic brim Pelvic diaphragm that separates the true pelvis above and perineum BELOW Perineum It is the diamond-shaped lower end of the trunk Glossary : peri : around, ineo - discharge, evacuate Location : it lies below the pelvic diaphragm, between the upper parts of the thighs. Boundaries : Anteriorly : Inferior margin of symphysis pubis. Posteriorly : Tip of coccyx. Anterolateral : Fused rami of pubis and ischium and ischial tuberosity. Posterolateral : Sacrotuberous ligaments. Dr.Ahmed Salman • Same boundaries as the pelvic Anteriorly: outlet. inferior part of • If we drew a line between the 2 symphysis pubis ischial tuberosities, the diamond shape will be divided into 2 triangles. Anterior and Anterior and Lateral : Lateral : •The ANTERIOR triangle is called ischiopubic ischiopubic urogenital triangle ramus The perineum ramus •The POSTERIOR triangle is called has a diamond anal triangle shape. ischial tuberosity Posterior and Posterior and Lateral : Lateral : Urogenital sacrotuberous sacrotuberous tri. ligament ligament Anal tri. Posteriorly : tip of coccyx UROGENITAL TRI. ANAL TRI. Divisions of the Perineum : By a line joining the anterior parts of the ischial tuberosities, the perineum is divided into two triangles : Anteriorly :Urogenital -

Lab #23 Anal Triangle
THE BONY PELVIS AND ANAL TRIANGLE (Grant's Dissector [16th Ed.] pp. 141-145) TODAY’S GOALS: 1. Identify relevant bony features/landmarks on skeletal materials or pelvic models. 2. Identify the sacrotuberous and sacrospinous ligaments. 3. Describe the organization and divisions of the perineum into two triangles: anal triangle and urogenital triangle 4. Dissect the ischiorectal (ischioanal) fossa and define its boundaries. 5. Identify the inferior rectal nerve and artery, the pudendal (Alcock’s) canal and the external anal sphincter. DISSECTION NOTES: The perineum is the diamond-shaped area between the upper thighs and below the inferior pelvic aperture and pelvic diaphragm. It is divided anatomically into 2 triangles: the anal triangle and the urogenital (UG) triangle (Dissector p. 142, Fig. 5.2). The anal triangle is bounded by the tip of the coccyx, sacrotuberous ligaments, and a line connecting the right and left ischial tuberosities. It contains the anal canal, which pierced the levator ani muscle portion of the pelvic diaphragm. The urogenital triangle is bounded by the ischiopubic rami to the inferior surface of the pubic symphysis and a line connecting the right and left ischial tuberosities. This triangular space contains the urogenital (UG) diaphragm that transmits the urethra (in male) and urethra and vagina (in female). A. Anal Triangle Turn the cadaver into the prone position. Make skin incisions as on page 144, Fig. 5.4 of the Dissector. Reflect skin and superficial fascia of the gluteal region in one flap to expose the large gluteus maximus muscle. This muscle has proximal attachments to the posteromedial surface of the ilium, posterior surfaces of the sacrum and coccyx, and the sacrotuberous ligament. -

Thoracic Outlet Syndrome of Pectoralis Minor Etiology Mimicking Cardiac
0008-3194/2012/311–315/$2.00/©JCCA 2012 Thoracic outlet syndrome of pectoralis minor etiology mimicking cardiac symptoms on activity: a case report Gary Fitzgerald BSc(NUI), BSc(Hons)(Chiro), MSc(Chiro), ICSSD* Thoracic outlet syndrome is the result of compression Le syndrome de la traversée thoracobrachial est le or irritation of neurovascular bundles as they pass résultat de la compression ou de l’irritation d’un from the lower cervical spine into the arm, via the paquet vasculonerveux au cours de son trajet entre axilla. If the pectoralis minor muscle is involved the la colonne cervicale inférieure et le bras, en passant patient may present with chest pain, along with pain par l’aisselle. Si le muscle petit pectoral est sollicité, and paraesthesia into the arm. These symptoms are also le patient peut subir de la douleur à la poitrine ainsi commonly seen in patients with chest pain of a cardiac que de la douleur et de la paresthésie dans le bras. origin. In this case, a patient presents with a history of On voit souvent ces symptômes aussi chez des patients left sided chest pain with pain and paraesthesia into the souffrant de douleurs thoraciques d’origine cardiaque. left upper limb, which only occurs whilst running. The Dans de tels cas, le patient présente des antécédents de symptoms were reproduced on both digital pressure over douleurs thoraciques du côté gauche, accompagnées the pectoralis minor muscle and on provocative testing de douleur et de paresthésie dans le membre supérieur for thoracic outlet syndrome. The patient’s treatment gauche, qui survient uniquement pendant que le patient therefore focused on the pectoralis minor muscle, with court. -

Build-A-Pelvis: Modeling Pelvic and Perineal Anatomy Female Pelvis
Build-A-Pelvis: Modeling Pelvic and Perineal Anatomy Female Pelvis Theodore Smith, M.S. Polly Husmann, Ph.D All images in this activity were created by the authors © Theodore Smith & Polly Husmann 2017 Materials needed: Pipecleaners-5 different colors Plastic Binder Pockets Scotch Tape Removable Adhesive Tack Masking Tape Scissors Bony Pelvis/Plastic Pelvis Model Fuzzy Pom-Poms Pens/Markers Flexible Plastic Tubing (optional) Image created by authors Structures Discussed: Perineal Membrane Ischiocavernosus Muscle Anal Triangle Bulbospongiosus Muscle Urogenital Diaphragm Superficial Perineal Pouch Deep Perineal Pouch External Anal Sphincter Superior fascia of the Urogenital Diaphragm Internal Anal Sphincter* External Urethral Sphincter Internal Urethral Sphincter* Compressor Urethrae Crura of the Clitoris Urethrovaginal Sphincter Bulb of the Vestibule Deep Transverse Perineal Muscle Greater Vestibular Glands Internal pudendal artery and vein Pudendal nerve Anal Canal* Vagina* Urethra* Superficial Transverse Perineal Muscles *only in optional activity with plastic tubing © Theodore Smith & Polly Husmann 2017 Build-A-Pelvis: Female Pelvis Directions 1) Begin by cutting 2 triangular pieces (wide isosceles, see Appendix A for templates) of the plastic binder dividers. These will serve as the perineal membrane (inferior fascia of urogenital diaphragm) and a boundary for the anal triangle. Cut a 3rd smaller triangle from the plastic dividers to serve as the superior fascia of the urogenital diaphragm. 2) Choose one large triangle to serve as the perineal membrane. Place the small triangle in the center of the large triangle and mark 2 spots a few centimeters apart in the midline of each triangle. At the marks, cut 2 holes. The hole closest to the pinnacle of the triangle will represent the opening for the urethra and the in- ferior will represent the opening for the vagina. -

Pectoral Region and Axilla Doctors Notes Notes/Extra Explanation Editing File Objectives
Color Code Important Pectoral Region and Axilla Doctors Notes Notes/Extra explanation Editing File Objectives By the end of the lecture the students should be able to : Identify and describe the muscles of the pectoral region. I. Pectoralis major. II. Pectoralis minor. III. Subclavius. IV. Serratus anterior. Describe and demonstrate the boundaries and contents of the axilla. Describe the formation of the brachial plexus and its branches. The movements of the upper limb Note: differentiate between the different regions Flexion & extension of Flexion & extension of Flexion & extension of wrist = hand elbow = forearm shoulder = arm = humerus I. Pectoralis Major Origin 2 heads Clavicular head: From Medial ½ of the front of the clavicle. Sternocostal head: From; Sternum. Upper 6 costal cartilages. Aponeurosis of the external oblique muscle. Insertion Lateral lip of bicipital groove (humerus)* Costal cartilage (hyaline Nerve Supply Medial & lateral pectoral nerves. cartilage that connects the ribs to the sternum) Action Adduction and medial rotation of the arm. Recall what we took in foundation: Only the clavicular head helps in flexion of arm Muscles are attached to bones / (shoulder). ligaments / cartilage by 1) tendons * 3 muscles are attached at the bicipital groove: 2) aponeurosis Latissimus dorsi, pectoral major, teres major 3) raphe Extra Extra picture for understanding II. Pectoralis Minor Origin From 3rd ,4th, & 5th ribs close to their costal cartilages. Insertion Coracoid process (scapula)* 3 Nerve Supply Medial pectoral nerve. 4 Action 1. Depression of the shoulder. 5 2. Draw the ribs upward and outwards during deep inspiration. *Don’t confuse the coracoid process on the scapula with the coronoid process on the ulna Extra III. -

CHAPTER 6 Perineum and True Pelvis
193 CHAPTER 6 Perineum and True Pelvis THE PELVIC REGION OF THE BODY Posterior Trunk of Internal Iliac--Its Iliolumbar, Lateral Sacral, and Superior Gluteal Branches WALLS OF THE PELVIC CAVITY Anterior Trunk of Internal Iliac--Its Umbilical, Posterior, Anterolateral, and Anterior Walls Obturator, Inferior Gluteal, Internal Pudendal, Inferior Wall--the Pelvic Diaphragm Middle Rectal, and Sex-Dependent Branches Levator Ani Sex-dependent Branches of Anterior Trunk -- Coccygeus (Ischiococcygeus) Inferior Vesical Artery in Males and Uterine Puborectalis (Considered by Some Persons to be a Artery in Females Third Part of Levator Ani) Anastomotic Connections of the Internal Iliac Another Hole in the Pelvic Diaphragm--the Greater Artery Sciatic Foramen VEINS OF THE PELVIC CAVITY PERINEUM Urogenital Triangle VENTRAL RAMI WITHIN THE PELVIC Contents of the Urogenital Triangle CAVITY Perineal Membrane Obturator Nerve Perineal Muscles Superior to the Perineal Sacral Plexus Membrane--Sphincter urethrae (Both Sexes), Other Branches of Sacral Ventral Rami Deep Transverse Perineus (Males), Sphincter Nerves to the Pelvic Diaphragm Urethrovaginalis (Females), Compressor Pudendal Nerve (for Muscles of Perineum and Most Urethrae (Females) of Its Skin) Genital Structures Opposed to the Inferior Surface Pelvic Splanchnic Nerves (Parasympathetic of the Perineal Membrane -- Crura of Phallus, Preganglionic From S3 and S4) Bulb of Penis (Males), Bulb of Vestibule Coccygeal Plexus (Females) Muscles Associated with the Crura and PELVIC PORTION OF THE SYMPATHETIC -

Ana Tomical Triangles J
43 ANA TOMICAL TRIANGLES J. LESLIE PACE, M.D. Department of Anatomy, Royal University of Malta Anatomical description is given of certain areas in the human hody which have :.l triangular sha!)e and which are of anatomical or surgical importance. There are at lea;,t 30 describe,d ,anatomical triangles, many of which receive eponymous names. Some are of nUlrked importance and well known e.g. Scarpa's femoral triangle, Hesselbach's inguinal triangle, H!ld Petit '5 lumbar triangle; others arc of relative1y minor importance and n.ot so well-known e.g. Elau's, Friteau's and Assezat's triangles. Anatomical trianlfles are described in various regions .of the body e.g. Macewen's ana Trautmann's in the head regiml, Beclaud's and PirDgoff's in the neck region, He'lSelbach '5, Henke '5, Petit's amI Grynfeltt's in the ,abdominal wall region and Searpa's Hnd Weber's in the lower limb Tf~gion. Their size varies, some being large e.g. Scarpa's triangle, others being very small e.g. Macewen's triangle. The bDundaries of these triangular areas may cDnsist of muscle borders e.g. the triangle .of Lannier and the variDUS tria,ngles of the neck; of n111sc1e borders and· bony cn1"fac(1,~ e.g. P(~lit'.~l tri,f)ng]c, t]1(' tria11['1]" ,C)f M'll"('ille J;lIlfl t1H~ tl"i[J11~le of Auscultation; of muscle borders and blood ves,ds e.g. Uesselbach's; of imaginary line, clrawn hetween fixed bony points e.g. -
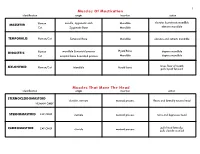
Muscles of Mastication Muscles That Move the Head
1 Muscles Of Mastication identification origin insertion action maxilla, zygomatic arch Mandible elevates & protracts mandible MASSETER Human Cat Zygomatic Bone Mandible elevates mandible TEMPORALIS Human/Cat Temporal Bone Mandible elevates and retracts mandible Hyoid Bone DIGASTRIC Human mandible & mastoid process depress mandible Cat occipital bone & mastoid process Mandible depress mandible raises floor of mouth; MYLOHYOID Human/Cat Mandible Hyoid bone pulls hyoid forward Muscles That Move The Head identification origin insertion action STERNOCLEIDOMAStoID clavicle, sternum mastoid process flexes and laterally rotates head HUMAN ONLY STERNOMAStoID CAT ONLY sternum mastoid process turns and depresses head pulls head laterally; CLEIDOMAStoID CAT ONLY clavicle mastoid process pulls clavicle craniad 2 Muscles Of The Hyoid, Larynx And Tongue identification origin insertion action Human Sternum Hyoid depresses hyoid bone STERNOHYOID Cat costal cartilage 1st rib Hyoid pulls hyoid caudally; raises ribs and sternum sternum Throid cartilage of larynx Human depresses thyroid cartilage STERNothYROID Cat costal cartilage 1st rib Throid cartilage of larynx pulls larynx caudad elevates thyroid cartilage and Human thyroid cartilage of larynx Hyoid THYROHYOID depresses hyoid bone Cat thyroid cartilage of larynx Hyoid raises larynx GENIOHYOID Human/Cat Mandible Hyoid pulls hyoid craniad 3 Muscles That Attach Pectoral Appendages To Vertebral Column identification origin insertion action Human Occipital bone; Thoracic and Cervical raises clavicle; adducts, -

Congenital Absence of the Pectoral Muscles
Arch Dis Child: first published as 10.1136/adc.12.68.123 on 1 April 1937. Downloaded from CONGENITAL ABSENCE OF THE PECTORAL MUSCLES BY E. D. IRVINE, M.D., AND J. B. TILLEY, M.D. (Blackburn). The four patients described in this paper exhibit congenital absence of the pectoral muscles in varying degree, and illustrate many points of interest. Three of them were observed during routine and special medical examinations of approximately 15,000 elementary school children, and one was a pre-school child in hospital: it is interesting to note that Scheslinger, according to Rector', discovered five cases in 54,000 patients. Case 1 was discovered during the examination of a boy aged ten, the second of four children, who complained of cough: he is under observation http://adc.bmj.com/ on September 30, 2021 by guest. Protected copyright. FIG. 1. as a tuberculosis contact. The sterno-costal portion of the left pectoralis major and the left pectoralis minor are both missing. Although not previously noted, this is believed to be a congenital defect. The clavicular head of the pectoralis major is well developed and arises from the inner half of the clavicle; the deltoid is not hypertrophied (fig. 1). When the arms are extended above the head, a well-marked fold of skin running vertically across the axilla to the second left rib and interspace can be seen and in Arch Dis Child: first published as 10.1136/adc.12.68.123 on 1 April 1937. Downloaded from I 2d4 AIICIlIVES 0O' DISEASE IN CHILDHOOD the fold fibrous tissue can be felt deep to the skin: whether this is simply fascia or a vestigial or degenerated muscle is not known.