Utah Medicaid Pharmacy & Therapeutics Committee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

In Silico Methods for Drug Repositioning and Drug-Drug Interaction Prediction
In silico Methods for Drug Repositioning and Drug-Drug Interaction Prediction Pathima Nusrath Hameed ORCID: 0000-0002-8118-9823 Submitted in total fulfilment of the requirements for the degree of Doctor of Philosophy Department of Mechanical Engineering THE UNIVERSITY OF MELBOURNE May 2018 Copyright © 2018 Pathima Nusrath Hameed All rights reserved. No part of the publication may be reproduced in any form by print, photoprint, microfilm or any other means without written permission from the author. Abstract Drug repositioning and drug-drug interaction (DDI) prediction are two fundamental ap- plications having a large impact on drug development and clinical care. Drug reposi- tioning aims to identify new uses for existing drugs. Moreover, understanding harmful DDIs is essential to enhance the effects of clinical care. Exploring both therapeutic uses and adverse effects of drugs or a pair of drugs have significant benefits in pharmacology. The use of computational methods to support drug repositioning and DDI prediction en- able improvements in the speed of drug development compared to in vivo and in vitro methods. This thesis investigates the consequences of employing a representative training sam- ple in achieving better performance for DDI classification. The Positive-Unlabeled Learn- ing method introduced in this thesis aims to employ representative positives as well as reliable negatives to train the binary classifier for inferring potential DDIs. Moreover, it explores the importance of a finer-grained similarity metric to represent the pairwise drug similarities. Drug repositioning can be approached by new indication detection. In this study, Anatomical Therapeutic Chemical (ATC) classification is used as the primary source to determine the indications/therapeutic uses of drugs for drug repositioning. -

Eslicarbazepine Acetate Longer Procedure No
European Medicines Agency London, 19 February 2009 Doc. Ref.: EMEA/135697/2009 CHMP ASSESSMENT REPORT FOR authorised Exalief International Nonproprietary Name: eslicarbazepine acetate longer Procedure No. EMEA/H/C/000987 no Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. product Medicinal 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 84 16 E-mail: [email protected] http://www.emea.europa.eu TABLE OF CONTENTS 1. BACKGROUND INFORMATION ON THE PROCEDURE........................................... 3 1.1. Submission of the dossier ...................................................................................................... 3 1.2. Steps taken for the assessment of the product..................................................................... 3 2. SCIENTIFIC DISCUSSION................................................................................................. 4 2.1. Introduction............................................................................................................................ 4 2.2. Quality aspects ....................................................................................................................... 5 2.3. Non-clinical aspects................................................................................................................ 8 2.4. Clinical aspects.................................................................................................................... -

Therapeutic Class Overview Anticonvulsants
Therapeutic Class Overview Anticonvulsants INTRODUCTION Epilepsy is a disease of the brain defined by any of the following (Fisher et al 2014): ○ At least 2 unprovoked (or reflex) seizures occurring > 24 hours apart; ○ 1 unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after 2 unprovoked seizures, occurring over the next 10 years; ○ Diagnosis of an epilepsy syndrome. Types of seizures include generalized seizures, focal (partial) seizures, and status epilepticus (Centers for Disease Control and Prevention [CDC] 2018, Epilepsy Foundation 2016). ○ Generalized seizures affect both sides of the brain and include: . Tonic-clonic (grand mal): begin with stiffening of the limbs, followed by jerking of the limbs and face . Myoclonic: characterized by rapid, brief contractions of body muscles, usually on both sides of the body at the same time . Atonic: characterized by abrupt loss of muscle tone; they are also called drop attacks or akinetic seizures and can result in injury due to falls . Absence (petit mal): characterized by brief lapses of awareness, sometimes with staring, that begin and end abruptly; they are more common in children than adults and may be accompanied by brief myoclonic jerking of the eyelids or facial muscles, a loss of muscle tone, or automatisms. ○ Focal seizures are located in just 1 area of the brain and include: . Simple: affect a small part of the brain; can affect movement, sensations, and emotion, without a loss of consciousness . Complex: affect a larger area of the brain than simple focal seizures and the patient loses awareness; episodes typically begin with a blank stare, followed by chewing movements, picking at or fumbling with clothing, mumbling, and performing repeated unorganized movements or wandering; they may also be called “temporal lobe epilepsy” or “psychomotor epilepsy” . -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -

(12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant Et Al
US 2010.0143507A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant et al. (43) Pub. Date: Jun. 10, 2010 (54) CARBOXYLIC ACID INHIBITORS OF Publication Classification HISTONE DEACETYLASE, GABA (51) Int. Cl. TRANSAMINASE AND SODIUM CHANNEL A633/00 (2006.01) A 6LX 3/553 (2006.01) A 6LX 3/553 (2006.01) (75) Inventors: Thomas G. Gant, Carlsbad, CA A63L/352 (2006.01) (US); Sepehr Sarshar, Cardiff by A6II 3/19 (2006.01) the Sea, CA (US) C07C 53/128 (2006.01) A6IP 25/06 (2006.01) A6IP 25/08 (2006.01) Correspondence Address: A6IP 25/18 (2006.01) GLOBAL PATENT GROUP - APX (52) U.S. Cl. .................... 424/722:514/211.13: 514/221; 10411 Clayton Road, Suite 304 514/456; 514/557; 562/512 ST. LOUIS, MO 63131 (US) (57) ABSTRACT Assignee: AUSPEX The present invention relates to new carboxylic acid inhibi (73) tors of histone deacetylase, GABA transaminase, and/or PHARMACEUTICALS, INC., Sodium channel activity, pharmaceutical compositions Vista, CA (US) thereof, and methods of use thereof. (21) Appl. No.: 12/632,507 Formula I (22) Filed: Dec. 7, 2009 Related U.S. Application Data (60) Provisional application No. 61/121,024, filed on Dec. 9, 2008. US 2010/014.3507 A1 Jun. 10, 2010 CARBOXYLIC ACID INHIBITORS OF HISTONE DEACETYLASE, GABA TRANSAMNASE AND SODIUM CHANNEL 0001. This application claims the benefit of priority of Valproic acid U.S. provisional application No. 61/121,024, filed Dec. 9, 2008, the disclosure of which is hereby incorporated by ref 0004 Valproic acid is extensively metabolised via erence as if written herein in its entirety. -
Acetazolamide
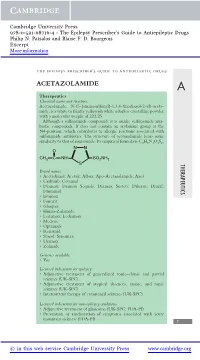
Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. Patsalos and Blaise F. D. Bourgeois Excerpt More information the epilepsy prescriber’s guide to antiepileptic drugs ACETAZOLAMIDE A Therapeutics Chemical name and structure: Acetazolamide, N-(5-(aminosulfonyl)-1,3,4-thiadiazol-2-yl)-aceta- mide, is a white to faintly yellowish white odorless crystalline powder with a molecular weight of 222.25. Although a sulfonamide compound, it is unlike sulfonamide anti- biotic compounds. It does not contain an arylamine group at the N4-position, which contributes to allergic reactions associated with sulfonamide antibiotics. The structure of acetazolamide bears some similarity to that of zonisamide. Its empirical formula is C4H6N4O3S2. NN O CH3 CNH SO2NH2 S THERAPEUTICS Brand names: r Acetadiazol; Acetak; Albox; Apo-Acetazolamide; Azol r Carbinib; Cetamid r Diamox; Diamox Sequals; Diamox Sustets; Diluran; Diural; Diuramid r Evamox r Fonurit r Glaupax r Huma-Zolamide r Ledamox; Lediamox r Medene r Optamide r Renamid r Stazol; Synomax r Uramox r Zolmide Generics available: r Yes Licensed indications for epilepsy: r Adjunctive treatment of generalized tonic–clonic and partial seizures (UK-SPC) r Adjunctive treatment of atypical absences, atonic, and tonic seizures (UK-SPC) r Intermittent therapy of catamenial seizures (UK-SPC) Licensed indications for non-epilepsy conditions: r Adjunctive treatment of glaucoma (UK-SPC; FDA-PI) r Prevention or amelioration of symptoms associated with acute mountain sickness (FDA-PI) 1 © in this web service Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. -

Topiramate Is More Effective Than Acetazolamide at Lowering
University of Birmingham Topiramate is more effective than acetazolamide at lowering intracranial pressure Scotton, William J; Botfield, Hannah F; Westgate, Connar Sj; Mitchell, James L; Yiangou, Andreas; Uldall, Maria S; Jensen, Rigmor H; Sinclair, Alex J DOI: 10.1177/0333102418776455 License: Creative Commons: Attribution (CC BY) Document Version Publisher's PDF, also known as Version of record Citation for published version (Harvard): Scotton, WJ, Botfield, HF, Westgate, CS, Mitchell, JL, Yiangou, A, Uldall, MS, Jensen, RH & Sinclair, AJ 2018, 'Topiramate is more effective than acetazolamide at lowering intracranial pressure', Cephalalgia. https://doi.org/10.1177/0333102418776455 Link to publication on Research at Birmingham portal Publisher Rights Statement: William J Scotton, Hannah F Botfield, Connar SJ Westgate, James L Mitchell, Andreas Yiangou, Maria S Uldall, Rigmor H Jensen, and Alex J Sinclair, Topiramate is more effective than acetazolamide at lowering intracranial pressure, Cephalalgia, First Published June 13, 2018; https://doi.org/10.1177/0333102418776455. Checked 02/07/2018. General rights Unless a licence is specified above, all rights (including copyright and moral rights) in this document are retained by the authors and/or the copyright holders. The express permission of the copyright holder must be obtained for any use of this material other than for purposes permitted by law. •Users may freely distribute the URL that is used to identify this publication. •Users may download and/or print one copy of the publication from the University of Birmingham research portal for the purpose of private study or non-commercial research. •User may use extracts from the document in line with the concept of ‘fair dealing’ under the Copyright, Designs and Patents Act 1988 (?) •Users may not further distribute the material nor use it for the purposes of commercial gain. -

Approach to Managing Patients with Sulfa Allergy Use of Antibiotic and Nonantibiotic Sulfonamides
CME Approach to managing patients with sulfa allergy Use of antibiotic and nonantibiotic sulfonamides David Ponka, MD, CCFP(EM) ABSTRACT OBJECTIVE To present an approach to use of sulfonamide-based (sulfa) medications for patients with sulfa allergy and to explore whether sulfa medications are contraindicated for patients who require them but are allergic to them. SOURCES OF INFORMATION A search of current pharmacology textbooks and of MEDLINE from 1966 to the present using the MeSH key words “sulfonamide” and “drug sensitivity” revealed review articles, case reports, one observational study (level II evidence), and reports of consensus opinion (level III evidence). MAIN MESSAGE Cross-reactivity between sulfa antibiotics and nonantibiotics is rare, but on occasion it can affect the pharmacologic and clinical management of patients with sulfa allergy. CONCLUSION How a physician approaches using sulfa medications for patients with sulfa allergy depends on the certainty and severity of the initial allergy, on whether alternatives are available, and on whether the contemplated agent belongs to the same category of sulfa medications (ie, antibiotic or nonantibiotic) as the initial offending agent. RÉSUMÉ OBJECTIF Proposer une façon d’utiliser les médicaments à base de sulfamides (sulfas) chez les patients allergiques aux sulfas et vérifier si ces médicaments sont contre-indiqués pour ces patients. SOURCES DE L’INFORMATION Une consultation des récents ouvrages de pharmacologie et de MEDLINE entre 1966 et aujourd’hui à l’aide des mots clés MeSH «sulfonamide» et «drug sensitivity» a permis de repérer plusieurs articles de revue et études de cas, une étude d’observation et des rapports d’opinion consensuelles (preuves de niveau III). -

Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis With
University of Rhode Island DigitalCommons@URI Pharmacy Practice Faculty Publications Pharmacy Practice 2018 Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis with Antiepileptic Drugs: An Analysis of the Food and Drug Administration Adverse Event Reporting System (FAERS) Eric P. Borrelli University of Rhode Island, [email protected] Erica Y. Lee University of Rhode Island SeFoe nelloxtw pa thige fors aaddndition addal aitutionhorsal works at: https://digitalcommons.uri.edu/php_facpubs The University of Rhode Island Faculty have made this article openly available. Please let us know how Open Access to this research benefits oy u. This is a pre-publication author manuscript of the final, published article. Terms of Use This article is made available under the terms and conditions applicable towards Open Access Policy Articles, as set forth in our Terms of Use. Citation/Publisher Attribution Borrelli EP, Lee EY, Descoteaux AM, Kogut SJ, Caffrey AR. Stevens‐Johnson syndrome and toxic epidermal necrolysis with antiepileptic drugs: An analysis of the US Food and Drug Administration Adverse Event Reporting System. Epilepsia. 2018;00:1–7. https://doi.org/10.1111/epi.14591 Available at: https://doi.org/10.1111/epi.14591 This Article is brought to you for free and open access by the Pharmacy Practice at DigitalCommons@URI. It has been accepted for inclusion in Pharmacy Practice Faculty Publications by an authorized administrator of DigitalCommons@URI. For more information, please contact [email protected]. Authors Eric P. Borrelli, Erica Y. Lee, Andrew M. Descoteaux, Stephen Jon Kogut, and Aisling R. Caffrey This article is available at DigitalCommons@URI: https://digitalcommons.uri.edu/php_facpubs/124 Title: Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis with Antiepileptic Drugs: An Analysis of the Food and Drug Administration Adverse Event Reporting System (FAERS) Authors: Eric P. -

"2-Oxo-1-Pyrrolidine Derivative and Its Pharmaceutical Uses"
(19) & (11) EP 1 452 524 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07D 207/27 (2006.01) A61K 31/4015 (2006.01) 14.10.2009 Bulletin 2009/42 A61P 25/08 (2006.01) (21) Application number: 04007878.4 (22) Date of filing: 21.02.2001 (54) "2-oxo-1-pyrrolidine derivative and its pharmaceutical uses" "2-Oxo-1-Pyrrolidinderivate und ihre pharmazeutische Verwendung" "Dérivé de 2-oxo-1-pyrrolidine et ses applications pharmaceutique" (84) Designated Contracting States: • Talaga, Patrice AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU 1170 Watermael-Boitsfort (BE) MC NL PT SE TR (74) Representative: UCB (30) Priority: 23.02.2000 GB 0004297 Intellectual Property c/o UCB S.A. (43) Date of publication of application: Intellectual Property Department 01.09.2004 Bulletin 2004/36 Allée de la Recherche 60 1070 Brussels (BE) (62) Document number(s) of the earlier application(s) in accordance with Art. 76 EPC: (56) References cited: 01925354.1 / 1 265 862 WO-A-99/13911 GB-A- 1 309 692 (73) Proprietor: UCB Pharma, S.A. • PROUS: "LEVETIRACETAM" DRUGS OF THE 1170 Brussels (BE) FUTURE, BARCELONA, ES, vol. 19, no. 2, 1994, pages 111-113, XP000908882 ISSN: 0377-8282 (72) Inventors: • FISCHER W ET AL: "Die Wirksamkeit von • Differding, Edmond Piracetam, Meclofenoxat und Vinpocetin in 1348 Ottignies-Louvain-La-Neuve (BE) verschiedenen Krampfmodellen bei der Maus" • Kenda, Benoît PHARMAZIE, VEB VERLAG VOLK UND 5080 Emines (BE) GESUNDHEIT. BERLIN, DD, vol. 46, no. -

Diamox/Aldactone to Increase the Urinary Excretion of Sodium: an Investigational Study in Congestive Heart Failure
Official Title: Diamox/Aldactone to Increase the URinary Excretion of Sodium: an Investigational Study in Congestive Heart Failure NCT01973335 Date: August 27, 2015 DIURESIS-CHF – Study protocol version August 27, 2015 1 1. Background Aging of the population and prolongation of the lives of cardiac patients by modern therapeutic innovations have led to an increased incidence of congestive heart failure (CHF).1 During the last two decades, important progress has been made in the treatment of ambulatory CHF patients with reduced ejection fraction. Renin-angiotensin system blockers, β-blockers, mineralocorticoid receptor antagonists (MRA), ivabradine and cardiac resynchronization therapy have all demonstrated to reduce morbidity and/or mortality in ambulatory CHF patients.2-17 Despite these important advances, many patients are still hospitalized frequently with signs and symptoms of systemic congestion, which is associated with worse outcome.18 Treatment in these cases mainly focuses on symptomatic relief through administration of diuretics, although clear evidence on the optimal agent, dosing schedule, and administration route is lacking. Coexisting renal dysfunction often complicates decongestive treatment and worsening renal function (WRF), often defined as a 0.3 mg/dL rise in serum creatinine (Cr), is a common finding in this context.19 However, the prognostic impact of WRF, defined as Cr change is unsure as it might be associated with worse, neutral or even better outcome.20-22 In contrast, persistent congestion, as a reflection of the inability of the kidneys to preserve sodium homeostasis, has been more consistently associated with higher mortality and more frequent readmissions in CHF.23 This suggests that achieving a negative sodium balance might be an attractive treatment target in heart failure. -

Drugs Affecting the Central Nervous System
Drugs affecting the central nervous system 15. Antiepileptic drugs (AEDs) Epilepsy is caused by the disturbance of the functions of the CNS. Although epileptic seizures have different symptoms, all of them involve the enhanced electric charge of a certain group of central neurons which is spontaneously discharged during the seizure. The instability of the cell membrane potential is responsible for this spontaneous discharge. This instability may result from: increased concentration of stimulating neurotransmitters as compared to inhibiting neurotransmitters decreased membrane potential caused by the disturbance of the level of electrolytes in cells and/or the disturbance of the function of the Na+/K+ pump when energy is insufficient. 2 Mutations in sodium and potassium channels are most common, because they give rise to hyperexcitability and burst firing. Mutations in the sodium channel subunits gene have been associated with - in SCN2A1; benign familial neonatal epilepsy - in SCN1A; severe myoclonic epilepsy of infancy - in SCN1A and SCN1B; generalized epilepsy with febrile seizures The potassium channel genes KCNQ2 and KCNQ3 are implicated in some cases of benign familial neonatal epilepsy. Mutations of chloride channels CLCN2 gene have been found to be altered in several cases of classical idiopathic generalized epilepsy suptypes: child-epilepsy and epilepsy with grand mal on awakening. Mutations of calcium channel subunits have been identified in juvenile absence epilepsy (mutation in CACNB4; the B4 subunit of the L-type calcium channel) and idiopathic generalized epilepsy (CACN1A1). 3 Mutations of GABAA receptor subunits also have been detected. The gene encoding the 1 subunit, GABRG1, has been linked to juvenile myoclonic epilepsy; mutated GABRG2, encoding an abnormal subunit, has been associated with generalized epilepsy with febrile seizures and childhood absence epilepsy.