Eslicarbazepine Acetate Longer Procedure No
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metabolic-Hydroxy and Carboxy Functionalization of Alkyl Moieties in Drug Molecules: Prediction of Structure Influence and Pharmacologic Activity
molecules Review Metabolic-Hydroxy and Carboxy Functionalization of Alkyl Moieties in Drug Molecules: Prediction of Structure Influence and Pharmacologic Activity Babiker M. El-Haj 1,* and Samrein B.M. Ahmed 2 1 Department of Pharmaceutical Sciences, College of Pharmacy and Health Sciences, University of Science and Technology of Fujairah, Fufairah 00971, UAE 2 College of Medicine, Sharjah Institute for Medical Research, University of Sharjah, Sharjah 00971, UAE; [email protected] * Correspondence: [email protected] Received: 6 February 2020; Accepted: 7 April 2020; Published: 22 April 2020 Abstract: Alkyl moieties—open chain or cyclic, linear, or branched—are common in drug molecules. The hydrophobicity of alkyl moieties in drug molecules is modified by metabolic hydroxy functionalization via free-radical intermediates to give primary, secondary, or tertiary alcohols depending on the class of the substrate carbon. The hydroxymethyl groups resulting from the functionalization of methyl groups are mostly oxidized further to carboxyl groups to give carboxy metabolites. As observed from the surveyed cases in this review, hydroxy functionalization leads to loss, attenuation, or retention of pharmacologic activity with respect to the parent drug. On the other hand, carboxy functionalization leads to a loss of activity with the exception of only a few cases in which activity is retained. The exceptions are those groups in which the carboxy functionalization occurs at a position distant from a well-defined primary pharmacophore. Some hydroxy metabolites, which are equiactive with their parent drugs, have been developed into ester prodrugs while carboxy metabolites, which are equiactive to their parent drugs, have been developed into drugs as per se. -

Actions of Glucagon-Like Peptide-1 on KATP Channel-Dependent and -Independent Effects of Glucose, Sulphonylureas and Nateglinide
889 Actions of glucagon-like peptide-1 on KATP channel-dependent and -independent effects of glucose, sulphonylureas and nateglinide Neville H McClenaghan1, Peter R Flatt1 and Andrew J Ball1,2 1School of Biomedical Sciences, University of Ulster, Coleraine BT52 1SA, Northern Ireland, UK 2Chemicon International Inc., 28820 Single Oak Drive, Temecula, California 92590, USA (Requests for offprints should be addressed to A J Ball; Email: [email protected]) Abstract This study examined the effects of glucagon-like peptide-1 PKA and PKC downregulation, indicating that GLP-1 can (GLP-1) on insulin secretion alone and in combination with modulate KATP channel-independent insulin secretion by sulphonylureas or nateglinide, with particular attention to KATP protein kinase-dependent and -independent mechanisms. The channel-independent insulin secretion. In depolarised cells, synergistic insulin-releasing effects of combinatorial GLP-1 and GLP-1 significantly augmented glucose-induced KATP sulphonylurea/nateglinide were lost following PKA- or PKC- channel-independent insulin secretion in a glucose concen- desensitisation, despite GLP-1 retaining an insulin-releasing tration-dependent manner. GLP-1 similarly augmented the effect, demonstrating that GLP-1 can induce insulin release KATP channel-independent insulin-releasing effects of tolbuta- under conditions where sulphonylureas and nateglinide are no mide, glibenclamide or nateglinide. Downregulation of protein longer effective. Our results provide new insights into the kinase A (PKA)- or protein kinase C (PKC)-signalling pathways mechanisms of action of GLP-1, and further highlight the in culture revealed that the KATP channel-independent effects of promise of GLP-1 or similarly acting analogues alone or in sulphonylureas or nateglinide were critically dependent upon combination with sulphonylureas or meglitinide drugs in type 2 intact PKA and PKC signalling. -

Inhibitory Effect of Eslicarbazepine Acetate and S-Licarbazepine on 2 Nav1.5 Channels
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.24.059188; this version posted August 14, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Inhibitory effect of eslicarbazepine acetate and S-licarbazepine on 2 Nav1.5 channels 3 Theresa K. Leslie1, Lotte Brückner 1, Sangeeta Chawla1,2, William J. Brackenbury1,2* 4 1Department of Biology, University of York, Heslington, York, YO10 5DD, UK 5 2York Biomedical Research Institute, University of York, Heslington, York, YO10 5DD, UK 6 * Correspondence: Dr William J. Brackenbury, Department of Biology and York Biomedical 7 Research Institute, University of York, Wentworth Way, Heslington, York YO10 5DD, UK. Email: 8 [email protected]. Tel: +44 1904 328284. 9 Keywords: Anticonvulsant, cancer, epilepsy, eslicarbazepine acetate, Nav1.5, S-licarbazepine, 10 voltage-gated Na+ channel. 11 Abstract 12 Eslicarbazepine acetate (ESL) is a dibenzazepine anticonvulsant approved as adjunctive treatment for 13 partial-onset epileptic seizures. Following first pass hydrolysis of ESL, S-licarbazepine (S-Lic) 14 represents around 95 % of circulating active metabolites. S-Lic is the main enantiomer responsible 15 for anticonvulsant activity and this is proposed to be through the blockade of voltage-gated Na+ 16 channels (VGSCs). ESL and S-Lic both have a voltage-dependent inhibitory effect on the Na+ current 17 in N1E-115 neuroblastoma cells expressing neuronal VGSC subtypes including Nav1.1, Nav1.2, 18 Nav1.3, Nav1.6 and Nav1.7. -

Management of Chronic Problems
MANAGEMENT OF CHRONIC PROBLEMS INTERACTIONS BETWEEN ALCOHOL AND DRUGS A. Leary,* T. MacDonald† SUMMARY concerned. Alcohol may alter the effects of the drug; drug In western society alcohol consumption is common as is may change the effects of alcohol; or both may occur. the use of therapeutic drugs. It is not surprising therefore The interaction between alcohol and drug may be that concomitant use of these should occur frequently. The pharmacokinetic, with altered absorption, metabolism or consequences of this combination vary with the dose of elimination of the drug, alcohol or both.2 Alcohol may drug, the amount of alcohol taken, the mode of affect drug pharmacokinetics by altering gastric emptying administration and the pharmacological effects of the drug or liver metabolism. Drugs may affect alcohol kinetics by concerned. Interactions may be pharmacokinetic or altering gastric emptying or inhibiting gastric alcohol pharmacodynamic, and while coincidental use of alcohol dehydrogenase (ADH).3 This may lead to altered tissue may affect the metabolism or action of a drug, a drug may concentrations of one or both agents, with resultant toxicity. equally affect the metabolism or action of alcohol. Alcohol- The results of concomitant use may also be principally drug interactions may differ with acute and chronic alcohol pharmacodynamic, with combined alcohol and drug effects ingestion, particularly where toxicity is due to a metabolite occurring at the receptor level without important changes rather than the parent drug. There is both inter- and intra- in plasma concentration of either. Some interactions have individual variation in the response to concomitant drug both kinetic and dynamic components and, where this is and alcohol use. -

Therapeutic Class Overview Anticonvulsants
Therapeutic Class Overview Anticonvulsants INTRODUCTION Epilepsy is a disease of the brain defined by any of the following (Fisher et al 2014): ○ At least 2 unprovoked (or reflex) seizures occurring > 24 hours apart; ○ 1 unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after 2 unprovoked seizures, occurring over the next 10 years; ○ Diagnosis of an epilepsy syndrome. Types of seizures include generalized seizures, focal (partial) seizures, and status epilepticus (Centers for Disease Control and Prevention [CDC] 2018, Epilepsy Foundation 2016). ○ Generalized seizures affect both sides of the brain and include: . Tonic-clonic (grand mal): begin with stiffening of the limbs, followed by jerking of the limbs and face . Myoclonic: characterized by rapid, brief contractions of body muscles, usually on both sides of the body at the same time . Atonic: characterized by abrupt loss of muscle tone; they are also called drop attacks or akinetic seizures and can result in injury due to falls . Absence (petit mal): characterized by brief lapses of awareness, sometimes with staring, that begin and end abruptly; they are more common in children than adults and may be accompanied by brief myoclonic jerking of the eyelids or facial muscles, a loss of muscle tone, or automatisms. ○ Focal seizures are located in just 1 area of the brain and include: . Simple: affect a small part of the brain; can affect movement, sensations, and emotion, without a loss of consciousness . Complex: affect a larger area of the brain than simple focal seizures and the patient loses awareness; episodes typically begin with a blank stare, followed by chewing movements, picking at or fumbling with clothing, mumbling, and performing repeated unorganized movements or wandering; they may also be called “temporal lobe epilepsy” or “psychomotor epilepsy” . -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -

Eslicarbazepine Acetate: a New Improvement on a Classic Drug Family for the Treatment of Partial-Onset Seizures
Drugs R D DOI 10.1007/s40268-017-0197-5 REVIEW ARTICLE Eslicarbazepine Acetate: A New Improvement on a Classic Drug Family for the Treatment of Partial-Onset Seizures 1 1 1 Graciana L. Galiana • Angela C. Gauthier • Richard H. Mattson Ó The Author(s) 2017. This article is an open access publication Abstract Eslicarbazepine acetate is a new anti-epileptic drug belonging to the dibenzazepine carboxamide family Key Points that is currently approved as adjunctive therapy and monotherapy for partial-onset (focal) seizures. The drug Eslicarbazepine acetate is an effective and safe enhances slow inactivation of voltage-gated sodium chan- treatment option for partial-onset seizures as nels and subsequently reduces the activity of rapidly firing adjunctive therapy and monotherapy. neurons. Eslicarbazepine acetate has few, but some, drug– drug interactions. It is a weak enzyme inducer and it Eslicarbazepine acetate improves upon its inhibits cytochrome P450 2C19, but it affects a smaller predecessors, carbamazepine and oxcarbazepine, by assortment of enzymes than carbamazepine. Clinical being available in a once-daily regimen, interacting studies using eslicarbazepine acetate as adjunctive treat- with a smaller range of drugs, and causing less side ment or monotherapy have demonstrated its efficacy in effects. patients with refractory or newly diagnosed focal seizures. The drug is generally well tolerated, and the most common side effects include dizziness, headache, and diplopia. One of the greatest strengths of eslicarbazepine acetate is its ability to be administered only once per day. Eslicar- 1 Introduction bazepine acetate has many advantages over older anti- epileptic drugs, and it should be strongly considered when Epilepsy is a common neurological disorder affecting over treating patients with partial-onset epilepsy. -

Epilepsy & Behavior
Epilepsy & Behavior 80 (2018) 365–369 Contents lists available at ScienceDirect Epilepsy & Behavior journal homepage: www.elsevier.com/locate/yebeh Brief Communication Eslicarbazepine acetate as a replacement for levetiracetam in people with epilepsy developing behavioral adverse events Virupakshi Jalihal a, Rohit Shankar b,c,⁎, William Henley c, Mary Parrett d, Phil Tittensor e, Brendan N. McLean d, Ammad Ahmed f, Josemir W. Sander g,h,i a Ramaiah Medical College and Hospitals, Bengaluru, Karnataka 560054, India b Cornwall Partnership NHS Foundation Trust, Threemilestone Industrial Estate, Truro TR4 9LD, UK c Exeter Medical School, Knowledge Spa, Royal Cornwall Hospital, Truro, Cornwall TR1 3HD, UK d Royal Cornwall Hospital, Truro, Cornwall TR1 3LJ, UK e Royal Wolverhampton NHS Trust, UK f Bial Pharma Ltd., Admiral House, Windsor SL4 3BL, UK g NIHR University College London Hospitals Biomedical Research Centre, UCL Institute of Neurology, Queen Square, London WC1N 3BG, UK h Chalfont Centre for Epilepsy, Chalfont St Peter, Buckinghamshire SL9 0RJ, UK i Stichting Epilepsie Instellingen Nederland (SEIN), Achterweg 5, 2103 SW Heemstede, Netherlands article info abstract Article history: Background: Psychiatric and behavioral side effects (PBSEs) are a major cause of antiepileptic drug (AED) Received 13 November 2017 withdrawal. Levetiracetam (LEV) is a recognized first-line AED with good seizure outcomes but recognized Revised 16 January 2018 with PBSEs. Eslicarbazepine (ESL) is considered to function similarly to an active metabolite of the commonly Accepted 17 January 2018 used carbamazepine (CBZ). Carbamazepine is used as psychotropic medication to assist in various psychiatric Available online 5 February 2018 illnesses such as mood disorders, aggression, and anxiety. -

Mechanisms of Action of Antiepileptic Drugs
Review Mechanisms of action of antiepileptic drugs Epilepsy affects up to 1% of the general population and causes substantial disability. The management of seizures in patients with epilepsy relies heavily on antiepileptic drugs (AEDs). Phenobarbital, phenytoin, carbamazepine and valproic acid have been the primary medications used to treat epilepsy for several decades. Since 1993 several AEDs have been approved by the US FDA for use in epilepsy. The choice of the AED is based primarily on the seizure type, spectrum of clinical activity, side effect profile and patient characteristics such as age, comorbidities and concurrent medical treatments. Those AEDs with broad- spectrum activity are often found to exert an action at more than one molecular target. This article will review the proposed mechanisms of action of marketed AEDs in the US and discuss the future of AEDs in development. 1 KEYWORDS: AEDs anticonvulsant drugs antiepileptic drugs epilepsy Aaron M Cook mechanism of action seizures & Meriem K Bensalem-Owen† The therapeutic armamentarium for the treat- patients with refractory seizures. The aim of this 1UK HealthCare, 800 Rose St. H-109, ment of seizures has broadened significantly article is to discuss the past, present and future of Lexington, KY 40536-0293, USA †Author for correspondence: over the past decade [1]. Many of the newer AED pharmacology and mechanisms of action. College of Medicine, Department of anti epileptic drugs (AEDs) have clinical advan- Neurology, University of Kentucky, 800 Rose Street, Room L-455, tages over older, so-called ‘first-generation’ First-generation AEDs Lexington, KY 40536, USA AEDs in that they are more predictable in their Broadly, the mechanisms of action of AEDs can Tel.: +1 859 323 0229 Fax: +1 859 323 5943 dose–response profile and typically are associ- be categorized by their effects on the neuronal [email protected] ated with less drug–drug interactions. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -
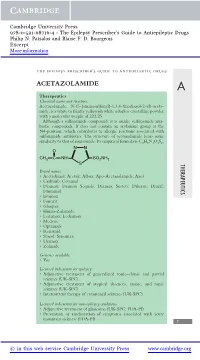
Acetazolamide
Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. Patsalos and Blaise F. D. Bourgeois Excerpt More information the epilepsy prescriber’s guide to antiepileptic drugs ACETAZOLAMIDE A Therapeutics Chemical name and structure: Acetazolamide, N-(5-(aminosulfonyl)-1,3,4-thiadiazol-2-yl)-aceta- mide, is a white to faintly yellowish white odorless crystalline powder with a molecular weight of 222.25. Although a sulfonamide compound, it is unlike sulfonamide anti- biotic compounds. It does not contain an arylamine group at the N4-position, which contributes to allergic reactions associated with sulfonamide antibiotics. The structure of acetazolamide bears some similarity to that of zonisamide. Its empirical formula is C4H6N4O3S2. NN O CH3 CNH SO2NH2 S THERAPEUTICS Brand names: r Acetadiazol; Acetak; Albox; Apo-Acetazolamide; Azol r Carbinib; Cetamid r Diamox; Diamox Sequals; Diamox Sustets; Diluran; Diural; Diuramid r Evamox r Fonurit r Glaupax r Huma-Zolamide r Ledamox; Lediamox r Medene r Optamide r Renamid r Stazol; Synomax r Uramox r Zolmide Generics available: r Yes Licensed indications for epilepsy: r Adjunctive treatment of generalized tonic–clonic and partial seizures (UK-SPC) r Adjunctive treatment of atypical absences, atonic, and tonic seizures (UK-SPC) r Intermittent therapy of catamenial seizures (UK-SPC) Licensed indications for non-epilepsy conditions: r Adjunctive treatment of glaucoma (UK-SPC; FDA-PI) r Prevention or amelioration of symptoms associated with acute mountain sickness (FDA-PI) 1 © in this web service Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. -

Anticonvulsants
Clinical Pharmacy Program Guidelines for Anticonvulsants Program Prior Authorization - Anticonvulsants Medication Aptiom (eslicarbazepine), Briviact (brivaracetam), Fycompa (perampanel), Vimpat (lacosamide), Gabitril (tiagabine), Banzel (rufinamide), Onfi (clobazam), Epidiolex (cannabidiol), Sympazan (clobazam), Sabril, (vigabatrin), Diacomit (stiripentol), Xcopri (cenobamate), Fintepla (fenfluramine) Markets in Scope Arizona, California, Colorado, Hawaii, Nevada, New Jersey, New York, New York EPP, Pennsylvania- CHIP, Rhode Island, South Carolina Issue Date 6/2016 Pharmacy and 10/2020 Therapeutics Approval Date Effective Date 12/2020 1. Background: Aptiom (eslicarbazepine acetate), Briviact (brivaracetam), Vimpat (lacosamide) and Xcopri are indicated in the treatment of partial-onset seizures. Banzel (rufinamide), Onfi (clobazam), and Sympazan (clobazam) are indicated for the adjunctive treatment of seizures associated with Lennox-Gastaut syndrome (LGS). There is some clinical evidence to support the use of clobazam for refractory partial onset seizures. Diacomit (stiripentol) is indicated for seizures associated with Dravet syndrome in patients taking clobazam. Epidiolex (cannabadiol) is indicated for seizures associated with Lennox-Gastaut syndrome, Dravet syndrome or tuberous sclerosis complex. Fintepla (fenfluramine) is indicated for the treatment of seizures associated with Dravet syndrome. Fycompa (perampanel) is indicated for the treatment of partial-onset seizures with or without secondarily generalized seizures and as adjunctive therapy for the treatment of primary generalized tonic-clonic seizures. Gabitril (tiagabine) is indicated ad adjunctive therapy in the treatment of partial-onset seizures. Confidential and Proprietary, © 2020 UnitedHealthcare Services Inc. Sabril (vigabatrin) is indicated as adjunctive therapy for refractory complex partial seizures in patients who have inadequately responded to several alternative treatments and for infantile spasms for whom the potential benefits outweigh the risk of vision loss.