Approach to Managing Patients with Sulfa Allergy Use of Antibiotic and Nonantibiotic Sulfonamides
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019): a Cross-Sectional Study
Tropical Medicine and Infectious Disease Article National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019): A Cross-Sectional Study Joseph Sam Kanu 1,2,* , Mohammed Khogali 3, Katrina Hann 4 , Wenjing Tao 5, Shuwary Barlatt 6,7, James Komeh 6, Joy Johnson 6, Mohamed Sesay 6, Mohamed Alex Vandi 8, Hannock Tweya 9, Collins Timire 10, Onome Thomas Abiri 6,11 , Fawzi Thomas 6, Ahmed Sankoh-Hughes 12, Bailah Molleh 4, Anna Maruta 13 and Anthony D. Harries 10,14 1 National Disease Surveillance Programme, Sierra Leone National Public Health Emergency Operations Centre, Ministry of Health and Sanitation, Cockerill, Wilkinson Road, Freetown, Sierra Leone 2 Department of Community Health, Faculty of Clinical Sciences, College of Medicine and Allied Health Sciences, University of Sierra Leone, Freetown, Sierra Leone 3 Special Programme for Research and Training in Tropical Diseases (TDR), World Health Organization, 1211 Geneva, Switzerland; [email protected] 4 Sustainable Health Systems, Freetown, Sierra Leone; [email protected] (K.H.); [email protected] (B.M.) 5 Unit for Antibiotics and Infection Control, Public Health Agency of Sweden, Folkhalsomyndigheten, SE-171 82 Stockholm, Sweden; [email protected] 6 Pharmacy Board of Sierra Leone, Central Medical Stores, New England Ville, Freetown, Sierra Leone; [email protected] (S.B.); [email protected] (J.K.); [email protected] (J.J.); [email protected] (M.S.); [email protected] (O.T.A.); [email protected] (F.T.) Citation: Kanu, J.S.; Khogali, M.; 7 Department of Pharmaceutics and Clinical Pharmacy & Therapeutics, Faculty of Pharmaceutical Sciences, Hann, K.; Tao, W.; Barlatt, S.; Komeh, College of Medicine and Allied Health Sciences, University of Sierra Leone, Freetown 0000, Sierra Leone 8 J.; Johnson, J.; Sesay, M.; Vandi, M.A.; Directorate of Health Security & Emergencies, Ministry of Health and Sanitation, Sierra Leone National Tweya, H.; et al. -

Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications
International Journal of Molecular Sciences Review Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications Daniel Fernández-Villa 1, Maria Rosa Aguilar 1,2 and Luis Rojo 1,2,* 1 Instituto de Ciencia y Tecnología de Polímeros, Consejo Superior de Investigaciones Científicas, CSIC, 28006 Madrid, Spain; [email protected] (D.F.-V.); [email protected] (M.R.A.) 2 Consorcio Centro de Investigación Biomédica en Red de Bioingeniería, Biomateriales y Nanomedicina, 28029 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-915-622-900 Received: 18 September 2019; Accepted: 7 October 2019; Published: 9 October 2019 Abstract: Bacterial, protozoan and other microbial infections share an accelerated metabolic rate. In order to ensure a proper functioning of cell replication and proteins and nucleic acids synthesis processes, folate metabolism rate is also increased in these cases. For this reason, folic acid antagonists have been used since their discovery to treat different kinds of microbial infections, taking advantage of this metabolic difference when compared with human cells. However, resistances to these compounds have emerged since then and only combined therapies are currently used in clinic. In addition, some of these compounds have been found to have an immunomodulatory behavior that allows clinicians using them as anti-inflammatory or immunosuppressive drugs. Therefore, the aim of this review is to provide an updated state-of-the-art on the use of antifolates as antibacterial and immunomodulating agents in the clinical setting, as well as to present their action mechanisms and currently investigated biomedical applications. Keywords: folic acid antagonists; antifolates; antibiotics; antibacterials; immunomodulation; sulfonamides; antimalarial 1. -

Eslicarbazepine Acetate Longer Procedure No
European Medicines Agency London, 19 February 2009 Doc. Ref.: EMEA/135697/2009 CHMP ASSESSMENT REPORT FOR authorised Exalief International Nonproprietary Name: eslicarbazepine acetate longer Procedure No. EMEA/H/C/000987 no Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. product Medicinal 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 84 16 E-mail: [email protected] http://www.emea.europa.eu TABLE OF CONTENTS 1. BACKGROUND INFORMATION ON THE PROCEDURE........................................... 3 1.1. Submission of the dossier ...................................................................................................... 3 1.2. Steps taken for the assessment of the product..................................................................... 3 2. SCIENTIFIC DISCUSSION................................................................................................. 4 2.1. Introduction............................................................................................................................ 4 2.2. Quality aspects ....................................................................................................................... 5 2.3. Non-clinical aspects................................................................................................................ 8 2.4. Clinical aspects.................................................................................................................... -

The Local Use of the Sulfonamide Drugs
THE LOCAL USE OF THE SULFONAMIDE DRUGS GEORGE CRILE Jr., M.D. Since the introduction of sulfanilamide and its derivatives, the reliance upon chemotherapy for the control of acute surgical infections has temporarily overshadowed the importance of sound surgical princi- ples and often has resulted in the administration of inefficient or inade- quate treatment. Too often, the physician fails to recognize the limita- tions of chemotherapy and vainly attempts to control the infection well beyond the optimum time for surgical intervention. Chemotherapy is very effective in controlling infections from hemo- lytic streptococcus; is moderately effective in controlling staphylococcic infections; but is of slight value when administered systemically in patients infected with the nonhemolytic streptococcus or colon bacillus. However, even in infections caused by the hemolytic streptococcus or the staphylococcus, sulfanilamide and sulfathiazole cannot replace surgery after suppuration has taken place and mechanical drainage of an abscess is required. It is in the treatment of lymphangitis and cellulitis, not in the treatment of abscesses, that chemotherapy has been of the greatest value. The work of Lockwood1 and others has indicated that the products of proteolysis in vitro interfere with the bacteriostatic and bacteriocidal powers of sulfanilamide. The presence of similar substances in undrained abscess cavities probably interferes with the destruction of the organ- isms by chemotherapy. Accordingly, the sulfonamide drugs should supplement rather than replace early and adequate surgical drainage, especially in the presence of suppuration. The local application of the sulfonamide drugs is based upon the principle that the local concentration of the drug in the tissues is ten to twenty times as high as that which can be obtained by any method of systemic administration. -
Xifaxan® (Rifaximin)
Wednesday, October 14, 2015 4 p.m. Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review Board Members FROM: Bethany Holderread, Pharm.D. SUBJECT: Packet Contents for Board Meeting – October 14, 2015 DATE: October 1, 2015 NOTE: The DUR Board will meet at 4:00 p.m. The meeting will be held at 4345 N Lincoln Blvd. Enclosed are the following items related to the October meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Action Item – Vote on 2016 Meeting Dates – Appendix B Update on Medication Coverage Authorization Unit/Bowel Preparation Medication Post-Educational Mailing – Appendix C Action Item – Vote to Prior Authorize Tykerb® (Lapatinib), Halaven® (Eribulin), Ixempra® (Ixabepilone), Kadcyla® (Ado-Trastuzumab), Afinitor® (Everolimus), & Perjeta® (Pertuzumab) – Appendix D Action Item – Vote to Prior Authorize Orkambi™ (Lumacaftor/Ivacaftor) – Appendix E Action Item – Vote to Prior Authorize Savaysa® (Edoxaban) – Appendix F Action Item – Vote to Prior Authorize Epanova® (Omega-3-Carboxylic Acids), Praluent® (Alirocumab), & Repatha™ (Evolocumab) – Appendix G Annual Review of Constipation and Diarrhea Medications and 30-Day Notice to Prior Authorize Movantik™ (Naloxegol), Viberzi™ (Eluxadoline), & Xifaxan® (Rifaximin) – Appendix H 30-Day Notice to Prior Authorize Daraprim® (Pyrimethamine) – Appendix I Annual Review of Allergy Immunotherapies and 30-Day Notice to Prior Authorize Oralair® (Sweet Vernal, Orchard, Perennial Rye, Timothy, & Kentucky Blue Grass Mixed Pollens Allergen Extract) – Appendix J Annual Review of Non-Steroidal Anti-Inflammatory Drugs and 30-Day Notice to Prior Authorize Dyloject™ (Diclofenac Sodium) – Appendix K ORI-4403 • P.O. -

Chloroquinoxaline Sulfonamide (NSC 339004) Is a Topoisomerase II␣/ Poison1
[CANCER RESEARCH 60, 5937–5940, November 1, 2000] Advances in Brief Chloroquinoxaline Sulfonamide (NSC 339004) Is a Topoisomerase II␣/ Poison1 Hanlin Gao, Edith F. Yamasaki, Kenneth K. Chan, Linus L. Shen, and Robert M. Snapka2 Departments of Radiology [H. G., E. F. Y., R. M. S.]; Molecular Virology, Immunology and Medical Genetics [H. G., R. M. S.]; College of Medicine [H. G., E. F. Y., R. M. S., K. K. C.]; and College of Pharmacy [K. K. C.], Ohio State University, Columbus, Ohio 43210, and Abbott Laboratories, Abbott Park, Illinois 60064 [L. L. S.] Abstract Drugs and Enzymes. CQS (NSC 339004) was provided by Dr. R. Shoe- maker, National Cancer Institute. VM-26 (teniposide, NSC 122819) was Chloroquinoxaline sulfonamide (chlorosulfaquinoxaline, CQS, NSC obtained from the National Cancer Institute Division of Cancer Treatment, 339004) is active against murine and human solid tumors. On the basis of Natural Products Branch. DMSO was the solvent for all drug stocks. Purified  its structural similarity to the topoisomerase II -specific drug XK469, human topoisomerase II␣ was from TopoGen (Columbus, OH) and LLS ␣ CQS was tested and found to be both a topoisomerase-II and a topoi- (Abbott Laboratories, Abbott Park, IL). Purified topoisomerase II was a  somerase-II poison. Topoisomerase II poisoning by CQS is essentially gift of Dr. Caroline Austin (University of Newcastle, Newcastle upon Tyne, undetectable in assays using the common protein denaturant SDS, but United Kingdom). easily detectable with strong chaotropic protein denaturants. The finding Filter Assay for in Vitro Topoisomerase-DNA Cross-links. The GF/C that detection of topoisomerase poisoning can be so dependent on the filter assay for protein-SV40 DNA cross-links is used to measure topoisomer- protein denaturant used in the assay has implications for drug discovery ase poisoning in vitro with purified enzymes and DNA substrates (9). -

Tetracycline and Sulfonamide Antibiotics in Soils: Presence, Fate and Environmental Risks
processes Review Tetracycline and Sulfonamide Antibiotics in Soils: Presence, Fate and Environmental Risks Manuel Conde-Cid 1, Avelino Núñez-Delgado 2 , María José Fernández-Sanjurjo 2 , Esperanza Álvarez-Rodríguez 2, David Fernández-Calviño 1,* and Manuel Arias-Estévez 1 1 Soil Science and Agricultural Chemistry, Faculty Sciences, University Vigo, 32004 Ourense, Spain; [email protected] (M.C.-C.); [email protected] (M.A.-E.) 2 Department Soil Science and Agricultural Chemistry, Engineering Polytechnic School, University Santiago de Compostela, 27002 Lugo, Spain; [email protected] (A.N.-D.); [email protected] (M.J.F.-S.); [email protected] (E.Á.-R.) * Correspondence: [email protected] Received: 30 October 2020; Accepted: 13 November 2020; Published: 17 November 2020 Abstract: Veterinary antibiotics are widely used worldwide to treat and prevent infectious diseases, as well as (in countries where allowed) to promote growth and improve feeding efficiency of food-producing animals in livestock activities. Among the different antibiotic classes, tetracyclines and sulfonamides are two of the most used for veterinary proposals. Due to the fact that these compounds are poorly absorbed in the gut of animals, a significant proportion (up to ~90%) of them are excreted unchanged, thus reaching the environment mainly through the application of manures and slurries as fertilizers in agricultural fields. Once in the soil, antibiotics are subjected to a series of physicochemical and biological processes, which depend both on the antibiotic nature and soil characteristics. Adsorption/desorption to soil particles and degradation are the main processes that will affect the persistence, bioavailability, and environmental fate of these pollutants, thus determining their potential impacts and risks on human and ecological health. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -
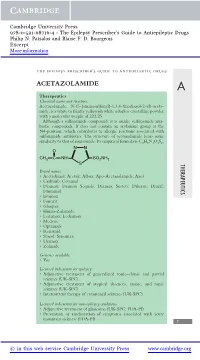
Acetazolamide
Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. Patsalos and Blaise F. D. Bourgeois Excerpt More information the epilepsy prescriber’s guide to antiepileptic drugs ACETAZOLAMIDE A Therapeutics Chemical name and structure: Acetazolamide, N-(5-(aminosulfonyl)-1,3,4-thiadiazol-2-yl)-aceta- mide, is a white to faintly yellowish white odorless crystalline powder with a molecular weight of 222.25. Although a sulfonamide compound, it is unlike sulfonamide anti- biotic compounds. It does not contain an arylamine group at the N4-position, which contributes to allergic reactions associated with sulfonamide antibiotics. The structure of acetazolamide bears some similarity to that of zonisamide. Its empirical formula is C4H6N4O3S2. NN O CH3 CNH SO2NH2 S THERAPEUTICS Brand names: r Acetadiazol; Acetak; Albox; Apo-Acetazolamide; Azol r Carbinib; Cetamid r Diamox; Diamox Sequals; Diamox Sustets; Diluran; Diural; Diuramid r Evamox r Fonurit r Glaupax r Huma-Zolamide r Ledamox; Lediamox r Medene r Optamide r Renamid r Stazol; Synomax r Uramox r Zolmide Generics available: r Yes Licensed indications for epilepsy: r Adjunctive treatment of generalized tonic–clonic and partial seizures (UK-SPC) r Adjunctive treatment of atypical absences, atonic, and tonic seizures (UK-SPC) r Intermittent therapy of catamenial seizures (UK-SPC) Licensed indications for non-epilepsy conditions: r Adjunctive treatment of glaucoma (UK-SPC; FDA-PI) r Prevention or amelioration of symptoms associated with acute mountain sickness (FDA-PI) 1 © in this web service Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. -
Antimicrobial and Anticancer Activity of Some Novel Fluorinated
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Ghorab et al. Chemistry Central Journal (2017) 11:32 DOI 10.1186/s13065-017-0258-4 RESEARCH ARTICLE Open Access Antimicrobial and anticancer activity of some novel fuorinated thiourea derivatives carrying sulfonamide moieties: synthesis, biological evaluation and molecular docking Mostafa M. Ghorab1,2*, Mansour S. Alsaid1, Mohamed S. A. El‑Gaby3*, Mahmoud M. Elaasser4 and Yassin M. Nissan5 Abstract Background: Various thiourea derivatives have been used as starting materials for compounds with better biological activities. Molecular modeling tools are used to explore their mechanism of action. Results: A new series of thioureas were synthesized. Fluorinated pyridine derivative 4a showed the highest anti‑ microbial activity (with MIC values ranged from 1.95 to 15.63 µg/mL). Interestingly, thiadiazole derivative 4c and coumarin derivative 4d exhibited selective antibacterial activities against Gram positive bacteria. Fluorinated pyridine derivative 4a was the most active against HepG2 with IC50 value of 4.8 μg/mL. Molecular docking was performed on the active site of MK-2 with good results. Conclusion: Novel compounds were obtained with good anticancer and antibacterial activity especially fuorinated pyridine derivative 4a and molecular docking study suggest good activity as mitogen activated protein kinase-2 inhibitor. Keywords: Isothiocyanate, Sulfonamide, Fluorinated thiourea, Antimicrobial and anticancer activity Background the increased hydrophobicity, and (v) the second small- Fluorinated compounds are intriguing for the develop- est atomic radius of the fuorine atom. Tese factors are ment of pharmaceuticals, agrochemicals, and materials, operative singly or sometimes cooperatively to afect the and thus, much efort has been exerted to develop more pharmacological properties of the fuorinated molecules general and efcient approaches for introducing fuorine [5]. -

Farrukh Javaid Malik
I Farrukh Javaid Malik THESIS PRESENTED TO OBTAIN THE GRADE OF DOCTOR OF THE UNIVERSITY OF BORDEAUX Doctoral School, SP2: Society, Politic, Public Health Specialization Pharmacoepidemiology and Pharmacovigilance By Farrukh Javaid Malik “Analysis of the medicines panorama in Pakistan – The case of antimicrobials: market offer width and consumption.” Under the direction of Prof. Dr. Albert FIGUERAS Defense Date: 28th November 2019 Members of Jury M. Francesco SALVO, Maître de conférences des universités – praticien hospitalier, President Université de Bordeaux M. Albert FIGUERAS, Professeur des universités – praticien hospitalier, Director Université Autonome de Barcelone Mme Antonia AGUSTI, Professeure, Vall dʹHebron University Hospital Referee Mme Montserrat BOSCH, Praticienne hospitalière, Vall dʹHebron University Hospital Referee II Abstract A country’s medicines market is an indicator of its healthcare system, the epidemiological profile, and the prevalent practices therein. It is not only the first logical step to study the characteristics of medicines authorized for marketing, but also a requisite to set up a pharmacovigilance system, thus promoting rational drug utilization. The three medicines market studies presented in the present document were conducted in Pakistan with the aim of describing the characteristics of the pharmaceutical products available in the country as well as their consumption at a national level, with a special focus on antimicrobials. The most important cause of antimicrobial resistance is the inappropriate consumption of antimicrobials. The results of the researches conducted in Pakistan showed some market deficiencies which could be addressed as part of the national antimicrobial stewardship programmes. III Résumé Le marché du médicament d’un pays est un indicateur de son système de santé, de son profil épidémiologique et des pratiques [de prescription] qui y règnent. -

Topiramate Is More Effective Than Acetazolamide at Lowering
University of Birmingham Topiramate is more effective than acetazolamide at lowering intracranial pressure Scotton, William J; Botfield, Hannah F; Westgate, Connar Sj; Mitchell, James L; Yiangou, Andreas; Uldall, Maria S; Jensen, Rigmor H; Sinclair, Alex J DOI: 10.1177/0333102418776455 License: Creative Commons: Attribution (CC BY) Document Version Publisher's PDF, also known as Version of record Citation for published version (Harvard): Scotton, WJ, Botfield, HF, Westgate, CS, Mitchell, JL, Yiangou, A, Uldall, MS, Jensen, RH & Sinclair, AJ 2018, 'Topiramate is more effective than acetazolamide at lowering intracranial pressure', Cephalalgia. https://doi.org/10.1177/0333102418776455 Link to publication on Research at Birmingham portal Publisher Rights Statement: William J Scotton, Hannah F Botfield, Connar SJ Westgate, James L Mitchell, Andreas Yiangou, Maria S Uldall, Rigmor H Jensen, and Alex J Sinclair, Topiramate is more effective than acetazolamide at lowering intracranial pressure, Cephalalgia, First Published June 13, 2018; https://doi.org/10.1177/0333102418776455. Checked 02/07/2018. General rights Unless a licence is specified above, all rights (including copyright and moral rights) in this document are retained by the authors and/or the copyright holders. The express permission of the copyright holder must be obtained for any use of this material other than for purposes permitted by law. •Users may freely distribute the URL that is used to identify this publication. •Users may download and/or print one copy of the publication from the University of Birmingham research portal for the purpose of private study or non-commercial research. •User may use extracts from the document in line with the concept of ‘fair dealing’ under the Copyright, Designs and Patents Act 1988 (?) •Users may not further distribute the material nor use it for the purposes of commercial gain.