Staphylococcus Aureus (Staph)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Family Practice
THE JOURNAL OF FAMILY ONLINE EXCLUSIVE PRACTICE Paul K. Carlton, Jr, MD, Brown recluse spider bite? FACS The Texas A&M University Consider this uniquely Health Science Center College Station, Tex conservative treatment [email protected] An antihistamine and observation work as well— and often better—than more intensive therapies. Practice recommendations oped it in 4 phases, which I describe in • Be concerned about brown recluse this article. Not only does this conser- envenomation when a patient vative approach consistently heal con- reports intensifying localized firmed brown recluse bite wounds, but pain disproportionate to physical should a bite be mistakenly attributed findings after a “bite” (C). to the brown recluse (or one of its rela- tives in the Loxosceles genus of spider), • Prescribe an oral antihistamine there is no harm to the patient, nor any alone to control symptoms, even big expense. with a necrotic wound, and mark the IN THIS ARTICLE patient’s progress over 24 hours (C). z Spider bite z Is a brown recluse • If the patient improves dramatically, to blame? or MRSA? continue the antihistamine; with little Due to limited experience among the Page E6 or no improvement, consider giving an wider medical community in identifying antibiotic with the antihistamine (C). spider envenomation,1-4 bite recognition and selection of appropriate therapy can Strength of recommendation (SOR) be difficult. A Good-quality patient-oriented evidence Early findings can be confusing. B Inconsistent or limited-quality patient-oriented evidence C Consensus, usual practice, opinion, disease-oriented Brown recluse bites typically feel like a evidence, case series pin prick. -

Drug-Resistant Streptococcus Pneumoniae and Methicillin
NEWS & NOTES Conference Summary pneumoniae can vary among popula- conference sessions was that statically tions and is influenced by local pre- sound methods of data collection that Drug-resistant scribing practices and the prevalence capture valid, meaningful, and useful of resistant clones. Conference pre- data and meet the financial restric- Streptococcus senters discussed the role of surveil- tions of state budgets are indicated. pneumoniae and lance in raising awareness of the Active, population-based surveil- Methicillin- resistance problem and in monitoring lance for collecting relevant isolates is the effectiveness of prevention and considered the standard criterion. resistant control programs. National- and state- Unfortunately, this type of surveil- Staphylococcus level epidemiologists discussed the lance is labor-intensive and costly, aureus benefits of including state-level sur- making it an impractical choice for 1 veillance data with appropriate antibi- many states. The challenges of isolate Surveillance otic use programs designed to address collection, packaging and transport, The Centers for Disease Control the antibiotic prescribing practices of data collection, and analysis may and Prevention (CDC) convened a clinicians. The potential for local sur- place an unacceptable workload on conference on March 12–13, 2003, in veillance to provide information on laboratory and epidemiology person- Atlanta, Georgia, to discuss improv- the impact of a new pneumococcal nel. ing state-based surveillance of drug- vaccine for children was also exam- Epidemiologists from several state resistant Streptococcus pneumoniae ined; the vaccine has been shown to health departments that have elected (DRSP) and methicillin-resistant reduce infections caused by resistance to implement enhanced antimicrobial Staphylococcus aureus (MRSA). -

What Is Staphylococcus Aureus (Staph)?
What is Staphylococcus aureus (staph)? Staphylococcus aureus, often referred to simply as "staph," are bacteria commonly carried on the skin or in the nose of healthy people. Approximately 25% to 30% of the population is colonized (when bacteria are present, but not causing an infection) in the nose with staph bacteria. Sometimes, staph can cause an infection. Staph bacteria are one of the most common causes of skin infections in the United States. Most of these skin infections are minor (such as pimples and boils) and can be treated without antibiotics (also known as antimicrobials or antibacterials). However, staph bacteria also can cause serious infections (such as surgical wound infections, bloodstream infections, and pneumonia). What is MRSA (methicillin-resistant Staphylococcus aureus)? Some staph bacteria are resistant to antibiotics. MRSA is a type of staph that is resistant to antibiotics called beta-lactams. Beta-lactam antibiotics include methicillin and other more common antibiotics such as oxacillin, penicillin and amoxicillin. While 25% to 30% of the population is colonized with staph, approximately 1% is colonized with MRSA. Who gets staph or MRSA infections? Staph infections, including MRSA, occur most frequently among persons in hospitals and healthcare facilities (such as nursing homes and dialysis centers) who have weakened immune systems. These healthcare-associated staph infections include surgical wound infections, urinary tract infections, bloodstream infections, and pneumonia. Are people who are positive for the human immune deficiency virus (HIV) at increased risk for MRSA? Should they be taking special precautions? People with weakened immune systems, which include some patients with HIV infection, may be at risk for more severe illness if they get infected with MRSA. -
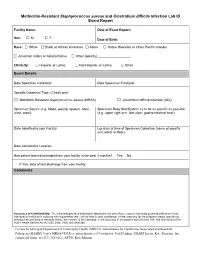
Methicillin-Resistant Staphylococcus Aureus and Clostridium Difficile Infection Lab ID Event Report
Methicillin-Resistant Staphylococcus aureus and Clostridium difficile Infection Lab ID Event Report Facility Name: Date of Event Report: Sex: M F □ □ Date of Birth: Race: □ White □ Black or African American □ Asian □ Native Hawaiian or Other Pacific Islander □ American Indian or Alaska Native □ Other [specify] __________________ Ethnicity: □ Hispanic or Latino □ Not Hispanic or Latino □ Other Event Details Date Specimen Collected: Date Specimen Finalized: Specific Organism Type: (Check one) □ Methicillin-Resistant Staphylococcus aureus (MRSA) □ Clostridium difficile Infection (CDI) Specimen Source (e.g. blood, wound, sputum, bone, Specimen Body Site/System try to be as specific as possible urine, stool): (e.g. upper right arm, foot ulcer, gastrointestinal tract): Date Admitted to your Facility: Location at time of Specimen Collection (name of specific unit, ward, or floor): Date Admitted to Location: Has patient been discharged from your facility in the past 3 months? Yes No If Yes, date of last discharge from your facility: Comments Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)). For use by Michigan Department of Community Health (MDCH), Surveillance for Healthcare-Associated and Resistant Pathogens (SHARP) Unit’s MRSA/CDI Prevention Initiative (Coordinator: Gail Denkins, SHARP Intern: Kate Manton); fax completed forms to (517) 335-8263, ATTN: Kate Manton. -
Staphylococcus Aureus (Staph Infection)
Staphylococcus aureus (Staph Infection) This sheet talks about exposure to Staphylococcus aureus and Staph infections in a pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare provider. What is Staphylococcus aureus / a Staph infection? Staphylococcus aureus (Staph) are a type of bacteria (germ). Staph bacteria are commonly found on the skin or in the nose. Most of the time, people will not have problems with these bacteria. However, if Staph gets inside the body through a cut or sore, this could lead to a Staph infection. Staph infection can cause boils or blisters on the skin; or infections in the lungs (pneumonia), bloodstream (sepsis), or in a wound. People with a higher chance of getting a Staph infection include sick people in hospitals, people recovering from surgeries or other medical procedures, people living in over-crowded conditions (shelters or prisons), children in daycare, intravenous (IV) drug users, people with weakened immune systems, people with chronic health conditions (like diabetes or cancer), athletes, and military personnel. Eating food that has been contaminated with Staph bacteria can also cause food poisoning. Symptoms can be severe vomiting and diarrhea with stomach pain that will start within a few hours after exposure. This type of infection with Staph bacteria usually is not serious and generally does not last for more than a day. I am pregnant. If my partner, other family member, or friend has a confirmed Staph skin infection, what can I do to reduce my chances of getting the infection? Do not touch the person’s sores, cuts, or bandages. -
Association Between Carriage of Streptococcus Pneumoniae and Staphylococcus Aureus in Children
BRIEF REPORT Association Between Carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children Gili Regev-Yochay, MD Context Widespread pneumococcal conjugate vaccination may bring about epidemio- Ron Dagan, MD logic changes in upper respiratory tract flora of children. Of particular significance may Meir Raz, MD be an interaction between Streptococcus pneumoniae and Staphylococcus aureus, in view of the recent emergence of community-acquired methicillin-resistant S aureus. Yehuda Carmeli, MD, MPH Objective To examine the prevalence and risk factors of carriage of S pneumoniae Bracha Shainberg, PhD and S aureus in the prevaccination era in young children. Estela Derazne, MSc Design, Setting, and Patients Cross-sectional surveillance study of nasopharyn- geal carriage of S pneumoniae and nasal carriage of S aureus by 790 children aged 40 Galia Rahav, MD months or younger seen at primary care clinics in central Israel during February 2002. Ethan Rubinstein, MD Main Outcome Measures Carriage rates of S pneumoniae (by serotype) and S aureus; risk factors associated with carriage of each pathogen. TREPTOCOCCUS PNEUMONIAE AND Results Among 790 children screened, 43% carried S pneumoniae and 10% car- Staphylococcus aureus are com- ried S aureus. Staphylococcus aureus carriage among S pneumoniae carriers was 6.5% mon inhabitants of the upper vs 12.9% in S pneumoniae noncarriers. Streptococcus pneumoniae carriage among respiratory tract in children and S aureus carriers was 27.5% vs 44.8% in S aureus noncarriers. Only 2.8% carried both Sare responsible for common infec- pathogens concomitantly vs 4.3% expected dual carriage (P=.03). Risk factors for tions. Carriage of S aureus and S pneu- S pneumoniae carriage (attending day care, having young siblings, and age older than moniae can result in bacterial spread and 3 months) were negatively associated with S aureus carriage. -
Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Clostridium difficile infection: How to deal with the problem DH INFORMATION RE ADER B OX Policy Estates HR / Workforce Commissioning Management IM & T Planning / Finance Clinical Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 9833 Title Clostridium difficile infection: How to deal with the problem Author DH and HPA Publication Date December 2008 Target Audience PCT CEs, NHS Trust CEs, SHA CEs, Care Trust CEs, Medical Directors, Directors of PH, Directors of Nursing, PCT PEC Chairs, NHS Trust Board Chairs, Special HA CEs, Directors of Infection Prevention and Control, Infection Control Teams, Health Protection Units, Chief Pharmacists Circulation List Description This guidance outlines newer evidence and approaches to delivering good infection control and environmental hygiene. It updates the 1994 guidance and takes into account a national framework for clinical governance which did not exist in 1994. Cross Ref N/A Superseded Docs Clostridium difficile Infection Prevention and Management (1994) Action Required CEs to consider with DIPCs and other colleagues Timing N/A Contact Details Healthcare Associated Infection and Antimicrobial Resistance Department of Health Room 528, Wellington House 133-155 Waterloo Road London SE1 8UG For Recipient's Use Front cover image: Clostridium difficile attached to intestinal cells. Reproduced courtesy of Dr Jan Hobot, Cardiff University School of Medicine. Clostridium difficile infection: How to deal with the problem Contents Foreword 1 Scope and purpose 2 Introduction 3 Why did CDI increase? 4 Approach to compiling the guidance 6 What is new in this guidance? 7 Core Guidance Key recommendations 9 Grading of recommendations 11 Summary of healthcare recommendations 12 1. -

Activation of the Bile Acid Pathway and No Observed Antimicrobial Peptide Sequences in the Skin of a Poison Frog
INVESTIGATION Activation of the Bile Acid Pathway and No Observed Antimicrobial Peptide Sequences in the Skin of a Poison Frog Megan L. Civitello,* Robert Denton,* Michael A. Zasloff,† and John H. Malone*,1 *Institute of Systems Genomics, Department of Molecular and Cell Biology, University of Connecticut, Storrs, Connecticut 06269 and †Georgetown University School of Medicine, MedStar Georgetown Transplant Institute, Washington D.C. 20057 ORCID IDs: 0000-0002-8629-1376 (R.D.); 0000-0003-1369-3769 (J.H.M.) ABSTRACT The skin secretions of many frogs have genetically-encoded, endogenous antimicrobial KEYWORDS peptides (AMPs). Other species, especially aposematic poison frogs, secrete exogenously derived alkaloids Anti-microbial that serve as potent defense molecules. The origins of these defense systems are not clear, but a novel bile- peptides acid derived metabolite, tauromantellic acid, was recently discovered and shown to be endogenous in defensive poison frogs (Mantella, Dendrobates, and Epipedobates). These observations raise questions about the secretions evolutionary history of AMP genetic elements, the mechanism and function of tauromatellic acid produc- phylogenetic tion, and links between these systems. To understand the diversity and expression of AMPs among frogs, history we assembled skin transcriptomes of 13 species across the anuran phylogeny. Our analyses revealed a bile acid pathway diversity of AMPs and AMP expression levels across the phylogenetic history of frogs, but no observations of AMPs in Mantella. We examined genes expressed in the bile-acid metabolic pathway and found that CYP7A1 (Cytochrome P450), BAAT (bile acid-CoA: amino acid N-acyltransferase), and AMACR (alpha- methylacyl-CoA racemase) were highly expressed in the skin of M. -

Note on Suspected Brown Recluse Spiders (Araneae: Sicariidae) in South Carolina
Faculty Research Note Note on Suspected Brown Recluse Spiders (Araneae: Sicariidae) in South Carolina Robert J. Wolff* South University, 9 Science Court, Columbia, SC 29203 The general public believes that brown recluse spiders (Loxosceles Filistatidae (Kukulcania hibernalis) 22 specimens reclusa) are widespread where they live and that these spiders are Lycosidae 21 (3 in one package, 5 in another) frequent causes of bites resulting in dermonecrosis. Research over the Pholcidae 17 past twenty years shows these reports to be unfounded. Vetter (2005) Miturgidae 8 examined 1,773 specimens sent in from across the U.S. as brown recluse Theridiidae 8 spiders and no specimens were found from areas outside the species Agelenidae 7 range, with the exception of a specimen from California. Araneidae 6 Clubionidae 6 The reported range of the brown recluse spider includes all or major Thomisidae 6 portions of Arkansas, Oklahoma, Texas, Louisiana, Alabama, Tennessee, Gnaphosidae 4 Kentucky, Illinois, Missouri and Kansas. Minor portions of the brown Corinnidae 3 recluse range were previously reported in Iowa, Indiana, Ohio, New Philodromidae 3 Mexico, North Carolina, Georgia, and South Carolina. The most recent Amaurobiidae 1 map (Vetter, 2015) does not include South Carolina, and only the far Pisauridae 1 western tip of North Carolina and northwestern corner of Georgia. Scytodidae (Scytodes thoracica) 1 Unidentifiable 4 Schuman and Caldwell (1991) found that South Carolina physicians reported treating 478 cases of brown recluse spider envenomations in 1990 alone. This seems like a very high number, unfortunately all or No brown recluses were identified from the specimens obtained in this almost all of these are probably not brown recluse spider bites. -

Methicillin-Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) Over the past several decades, the incidence of resistant gram-positive organisms has risen in the United States. MRSA strains, first identified in the 1960s in England, were first observed in the U.S. in the mid 1980s.1 Resistance quickly developed, increasing from 2.4% in 1979 to 29% in 1991.2 The current prevalence for MRSA in hospitals and other facilities ranges from <10% to 65%. In 1999, MRSA accounted for more than 50% of all Staphylococcus aureus isolates within U.S. intensive care units.3, 4 The past years, however, outbreaks of MRSA have also been seen in the community setting, particularly among preschool-age children, some of whom have attended day-care centers.5, 6, 7 MRSA does not appear to be more virulent than methicillin-sensitive Staphylococcus aureus, but certainly poses a greater treatment challenge. MRSA also has been associated with higher hospital costs and mortality.8 Within a decade of its development, methicillin resistance to Staphylococcus aureus emerged.9 MRSA strains generally are now resistant to other antimicrobial classes including aminoglycosides, beta-lactams, carbapenems, cephalosporins, fluoroquinolones and macrolides.10,11 Most of the resistance was secondary to production of beta-lactamase enzymes or intrinsic resistance with alterations in penicillin-binding proteins. Staphylococcus aureus is the most frequent cause of nosocomial pneumonia and surgical- wound infections and the second most common cause of nosocomial bloodstream infections.12 Long-term care facilities (LTCFs) have developed rates of MRSA ranging from 25%-35%. MRSA rates may be higher in LTCFs if they are associated with hospitals that have higher rates.13 Transmission of MRSA generally occurs through direct or indirect contact with a reservoir. -

Methicillin Resistant Staphylococcus Aureus (MRSA)
Methicillin resistant Staphylococcus aureus (MRSA), Clostridium difficile and ESBL-producing Escherichia coli in the home and community: assessing the problem, controlling the spread An expert report commissioned by the International Scientific Forum on Home Hygiene © International Scientific Forum on Home Hygiene, 2006 2 CONTENTS ACKNOWLEDGMENTS 4 SUMMARY 5 1. INTRODUCTION – INFECTIOUS DISEASE AND HYGIENE IN THE 21ST CENTURY 7 2. THE CHAIN OF INFECTION TRANSMISSION IN THE HOME 10 3. METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS (MRSA) 11 3.1 CHARACTERISTICS OF STAPHYLOCOCCUS AUREUS AND METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS 11 3.2 HOSPITAL-ACQUIRED, HEALTHCARE ASSOCIATED AND COMMUNITY ACQUIRED MRSA 11 3.3 UNDERSTANDING THE CHAIN OF INFECTION FOR S. AUREUS AND MRSA IN THE HOME 13 3.4 WHAT ARE THE RISKS ASSOCIATED WITH S. AUREUS AND MRSA IN THE COMMUNITY? 22 4. CLOSTRIDIUM DIFFICILE 24 4.1 CHARACTERISTICS OF CLOSTRIDIUM DIFFICILE 24 4.2 HOSPITAL-ACQUIRED AND COMMUNITY- ACQUIRED C. DIFFICILE 24 4.3 UNDERSTANDING THE CHAIN OF INFECTION FOR C. DIFFICILE IN THE HOME 25 4.4 WHAT ARE THE RISKS ASSOCIATED WITH C. DIFFICILE IN THE HOME AND COMMUNITY 28 5. EXTENDED-SPECTRUM ß-LACTAMASE ESCHERICHIA COLI (ESBLS) 30 5.1 CHARACTERISTICS OF ESCHERICHIA COLI 30 5.2 HOSPITAL AND COMMUNITY-ACQUIRED ESBL-PRODUCING E. COLI INFECTIONS 31 5.3 UNDERSTANDING THE CHAIN OF INFECTION FOR E. COLI AND ESBL-PRODUCING E. COLI IN THE HOME 31 5.4 RISKS ASSOCIATED WITH ESBLS IN THE COMMUNITY 33 6. REDUCING THE RISKS OF TRANSMISSION OF METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS (MRSA), CLOSTRIDIUM DIFFICILE AND ESBL-PRODUCING ESCHERICHIA COLI IN THE HOME AND COMMUNITY - DEVELOPING A RISK-BASED APPROACH TO HOME HYGIENE 35 6.1 BREAKING THE CHAIN OF TRANSMISSION OF INFECTION IN THE HOME 35 6.2 DEVELOPING A RISK-BASED APPROACH TO HOME HYGIENE 35 6.3 INTERRUPTING THE CHAIN OF INFECTION TRANSMISSION IN THE HOME 38 7. -

Staphylococcus Aureus Bloodstream Infection Treatment Guideline
Staphylococcus aureus Bloodstream Infection Treatment Guideline Purpose: To provide a framework for the evaluation and management patients with Methicillin- Susceptible (MSSA) and Methicillin-Resistant Staphylococcus aureus (MRSA) bloodstream infections (BSI). The recommendations below are guidelines for care and are not meant to replace clinical judgment. The initial page includes a brief version of the guidance followed by a more detailed discussion of the recommendations with supporting evidence. Also included is an algorithm describing management of patients with blood cultures positive for gram-positive cocci. Brief Key Points: 1. Don’t ignore it – Staphylococcus aureus isolated from a blood culture is never a contaminant. All patients with S. aureus in their blood should be treated with appropriate antibiotics and evaluated for a source of infection. 2. Control the source a. Removing infected catheters and prosthetic devices – Retention of infected central venous catheters and prosthetic devices in the setting of S. aureus bacteremia (SAB) has been associated with prolonged bacteremia, treatment failure and death. These should be removed if medically possible. i. Retention of prosthetic material is associated with an increased likelihood of SAB relapse and removal should be considered even if not clearly infected b. Evaluate for metastatic infections (endocarditis, osteomyelitis, abscesses, etc.) – Metastatic infections and endocarditis are quite common in SAB (11-31% patients with SAB have endocarditis). i. All patients should have a thorough history taken and exam performed with any new complaint evaluated for possible metastatic infection. ii. Echocardiograms should be strongly considered for all patients with SAB iii. All patients with a prosthetic valve, pacemaker/ICD present, or persistent bacteremia (follow up blood cultures positive) should undergo a transesophageal echocardiogram 3.