Drug-Induced Diseases: Depression
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -
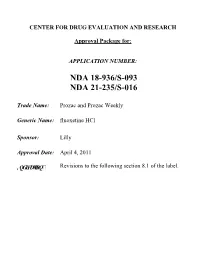
Prozac and Prozac Weekly (Fluoxetine Hcl)
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: NDA 18-936/S-093 NDA 21-235/S-016 Trade Name: Prozac and Prozac Weekly Generic Name: fluoxetine HCl Sponsor: Lilly Approval Date: April 4, 2011 ,QGLFDWLRQ Revisions to the following section 8.1 of the label. CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 18-936/S-093 NDA 21-235/S-016 CONTENTS Reviews / Information Included in this NDA Review. Approval Letter X Other Action Letters X Labeling Summary Review X Officer/Employee List Office Director Memo Cross Discipline Team Leader Review Medical Review(s) X Chemistry Review(s) Pharmacology Review(s) Statistical Review(s) Clinical Pharmacology/Biopharmaceutics Review(s) Other Reviews X Proprietary Name Review(s) Administrative/Correspondence Document(s) X CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 18-936/S-093 NDA 21-235/S-016 APPROVAL LETTER DEPARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 NDA 018936/S-091/S-093/S-095 NDA 021235/S-015/S-016/S-017 SUPPLEMENT APPROVAL Eli Lilly & Company Attention: Kevin C. Sheehan, MS, Pharm.D. Manager, Global Regulatory Affairs - US Lilly Corporate Center Indianapolis, IN 46285 Dear Dr. Sheehan: Please refer to your Supplemental New Drug Applications (sNDA) dated and received May 21, 2009 (018936/S-091 and 021235/S-015), November 6, 2009 (018936/S-093 and 021235/S-016), and April 14, 2010 (018936/S-095 and 021235/S-017), submitted under section 505(b) of the Federal Food, Drug, and Cosmetic Act (FDCA) for Prozac (fluoxetine hydrochloride) 10 mg, 20 mg, and 40 mg capsules and Prozac Weekly (fluoxetine hydrochloride) 90 mg delayed-release capsules. -

PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50 and 75 mg Antidepressant AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road Unit #1 August 29, 2018 Vaughan, ON L4K 4N7 Control No.: 217626 1 PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50, 75 mg THERAPEUTIC CLASSIFICATION Antidepressant ACTIONS AND CLINICAL PHARMACOLOGY Amitriptyline hydrochloride is a tricyclic antidepressant with sedative properties. Its mechanism of action in man is not known. Amitriptyline inhibits the membrane pump mechanism responsible for the re-uptake of transmitter amines, such as norepinephrine and serotonin, thereby increasing their concentration at the synaptic clefts of the brain. Amitriptyline has pronounced anticholinergic properties and produces EKG changes and quinidine-like effects on the heart (See ADVERSE REACTIONS). It also lowers the convulsive threshold and causes alterations in EEG and sleep patterns. Orally administered amitriptyline is readily absorbed and rapidly metabolized. Steady-state plasma concentrations vary widely and this variation may be genetically determined. Amitriptyline is primarily excreted in the urine, mostly in the form of metabolites, with some excretion also occurring in the feces. INDICATIONS AND CLINICAL USE ELAVIL® (amitriptyline hydrochloride) is indicated in the drug management of depressive illness. ELAVIL® may be used in depressive illness of psychotic or endogenous nature and in selected patients with neurotic depression. Endogenous depression is more likely to be alleviated than are other depressive states. ELAVIL® ®, because of its sedative action, is also of value in alleviating the anxiety component of depression. As with other tricyclic antidepressants, ELAVIL® may precipitate hypomanic episodes in patients with bipolar depression. These drugs are not indicated in mild depressive states and depressive reactions. -

Management of Major Depressive Disorder Clinical Practice Guidelines May 2014
Federal Bureau of Prisons Management of Major Depressive Disorder Clinical Practice Guidelines May 2014 Table of Contents 1. Purpose ............................................................................................................................................. 1 2. Introduction ...................................................................................................................................... 1 Natural History ................................................................................................................................. 2 Special Considerations ...................................................................................................................... 2 3. Screening ........................................................................................................................................... 3 Screening Questions .......................................................................................................................... 3 Further Screening Methods................................................................................................................ 4 4. Diagnosis ........................................................................................................................................... 4 Depression: Three Levels of Severity ............................................................................................... 4 Clinical Interview and Documentation of Risk Assessment............................................................... -

Tactile Stimulation on Adulthood Modifies the HPA Axis, Neurotrophic Factors, and GFAP Signaling Reverting Depression-Like Behavior in Female Rats
Molecular Neurobiology (2019) 56:6239–6250 https://doi.org/10.1007/s12035-019-1522-5 Tactile Stimulation on Adulthood Modifies the HPA Axis, Neurotrophic Factors, and GFAP Signaling Reverting Depression-Like Behavior in Female Rats Kr. Roversi1 & Caren Tatiane de David Antoniazzi1 & L. H. Milanesi1 & H. Z. Rosa1 & M. Kronbauer1 & D. R. Rossato2 & T. Duarte1 & M. M. Duarte3 & Marilise E. Burger1 Received: 9 October 2018 /Accepted: 30 January 2019 /Published online: 11 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Depression is a common psychiatric disease which pharmacological treatment relieves symptoms, but still far from ideal. Tactile stimulation (TS) has shown beneficial influences in neuropsychiatric disorders, but the mechanism of action is not clear. Here, we evaluated the TS influence when applied on adult female rats previously exposed to a reserpine-induced depression-like animal model. Immediately after reserpine model (1 mg/kg/mL, 1×/day, for 3 days), female Wistar rats were submitted to TS (15 min, 3×/day, for 8 days) or not (unhandled). Imipramine (10 mg/kg/mL) was used as positive control. After behavioral assessments, animals were euthanized to collect plasma and prefrontal cortex (PFC). Behavioral observations in the forced swimming test, splash test, and sucrose preference confirmed the reserpine-induced depression-like behavior, which was reversed by TS. Our findings showed that reserpine increased plasma levels of adrenocorticotropic hormone and corticosterone, decreased brain- derived neurotrophic factor (BDNF) and tropomyosin receptor kinase B, and increased proBDNF immunoreactivity in the PFC, which were also reversed by TS. Moreover, TS reestablished glial fibrillary acidic protein and glucocorticoid receptor levels, decreased by reserpine in PFC, while glial cell line–derived neurotrophic factor was increased by TS per se. -

Q 2: How Long Should Treatment with Antidepressants Continue in Adults with Depressive Episode/Disorder?
Duration of antidepressant treatment Q 2: How long should treatment with antidepressants continue in adults with depressive episode/disorder? Background Short-term therapy with antidepressant medication is considered standard treatment for acute treatment of moderate to severe depressive episode/disorder. However, because of the long-term nature of depressive disorders, with many patients at substantial risk of later recurrence, there is a need to establish how long, in general, such patients should stay on antidepressants if they have responded to the treatment. Population/Intervention(s)/Comparison/Outcome(s) (PICO) Population: individuals with depressive episode/disorder Interventions: antidepressant medications: tricyclic antidepressants (TCA) and related, selective serotonin reuptake inhibitors (SSRI) Comparison: placebo Outcomes: o treatment effectiveness in terms of reduction symptoms o treatment effectiveness in terms of improvement in functioning o acceptability profile List of the systematic reviews identified by the search process INCLUDED IN GRADE TABLES OR FOOTNOTES Deshauer D et al (2008). Selective serotonin reuptake inhibitors for unipolar depression: a systematic review of classic long-term randomized controlled trials. Canadian Medical Association Journal, 178:293-1301. 1 Duration of antidepressant treatment Geddes JR et al (2003). Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet, 361:653-61. Hansen R et al (2008). Meta-analysis of major depressive disorder relapse and recurrence with second-generation antidepressants. Psychiatric Services, 59:1121-30. Kaymaz N et al (2008). Evidence that patients with single versus recurrent depressive episodes are differentially sensitive to treatment discontinuation: a meta- analysis of placebo-controlled randomized trials. Journal of Clinical Psychiatry, 69:1423-36. -

Drug Repurposing for the Management of Depression: Where Do We Stand Currently?
life Review Drug Repurposing for the Management of Depression: Where Do We Stand Currently? Hosna Mohammad Sadeghi 1,†, Ida Adeli 1,† , Taraneh Mousavi 1,2, Marzieh Daniali 1,2, Shekoufeh Nikfar 3,4,5 and Mohammad Abdollahi 1,2,* 1 Toxicology and Diseases Group (TDG), Pharmaceutical Sciences Research Center (PSRC), The Institute of Pharmaceutical Sciences (TIPS), Tehran University of Medical Sciences, Tehran 1417614411, Iran; [email protected] (H.M.S.); [email protected] (I.A.); [email protected] (T.M.); [email protected] (M.D.) 2 Department of Toxicology and Pharmacology, School of Pharmacy, Tehran University of Medical Sciences, Tehran 1417614411, Iran 3 Personalized Medicine Research Center, Endocrinology and Metabolism Research Institute, Tehran University of Medical Sciences, Tehran 1417614411, Iran; [email protected] 4 Pharmaceutical Sciences Research Center (PSRC) and the Pharmaceutical Management and Economics Research Center (PMERC), Evidence-Based Evaluation of Cost-Effectiveness and Clinical Outcomes Group, The Institute of Pharmaceutical Sciences (TIPS), Tehran University of Medical Sciences, Tehran 1417614411, Iran 5 Department of Pharmacoeconomics and Pharmaceutical Administration, School of Pharmacy, Tehran University of Medical Sciences, Tehran 1417614411, Iran * Correspondence: [email protected] † Equally contributed as first authors. Citation: Mohammad Sadeghi, H.; Abstract: A slow rate of new drug discovery and higher costs of new drug development attracted Adeli, I.; Mousavi, T.; Daniali, M.; the attention of scientists and physicians for the repurposing and repositioning of old medications. Nikfar, S.; Abdollahi, M. Drug Experimental studies and off-label use of drugs have helped drive data for further studies of ap- Repurposing for the Management of proving these medications. -

Determination of Salivary Efavirenz by Liquid Chromatography Coupled with Tandem Mass Spectrometry
G Model CHROMB-17040; No. of Pages 5 ARTICLE IN PRESS Journal of Chromatography B, xxx (2010) xxx–xxx Contents lists available at ScienceDirect Journal of Chromatography B journal homepage: www.elsevier.com/locate/chromb Determination of salivary efavirenz by liquid chromatography coupled with tandem mass spectrometry Anri Theron a, Duncan Cromarty b, Malie Rheeders a, Michelle Viljoen a,∗ a Pharmacology, School of Pharmacy & Unit for Drug Research and Development North-West University, Private Bag X6001, Building G16, Room 113, Potchefstroom 2520, South Africa b Department of Pharmacology, Medical School, University of Pretoria, PO Box 2034, Pretoria 0001, South Africa article info abstract Article history: A novel and robust screening method for the determination of the non-nucleoside reverse transcriptase Received 12 May 2010 inhibitor, efavirenz (EFV), in human saliva has been developed and validated based on high perfor- Accepted 31 August 2010 mance liquid chromatography tandem mass spectrometry (LC–MS/MS). Sample preparation of the saliva Available online xxx involved solid-phase extraction (SPE) on C18 cartridges. The analytes were separated by high perfor- mance liquid chromatography (Phenomenex Kinetex C18, 150 mm × 3 mm internal diameter, 2.6 m Keywords: particle size) and detected with tandem mass spectrometry in electrospray positive ionization mode Efavirenz with multiple reaction monitoring. Gradient elution with increasing methanol (MeOH) concentration Saliva LC–MS/MS was used to elute the analytes, at a flow-rate of 0.4 mL/min. The total run time was 8.4 min and the retention times for the internal standard (reserpine) was 5.4 min and for EFV was 6.5 min. -

Quinidine, Beta-Blockers, Diphenylhydantoin, Bretylium *
Pharmacology of Antiarrhythmics: Quinidine, Beta-Blockers, Diphenylhydantoin, Bretylium * ALBERT J. WASSERMAN, M.D. Professor of Medicine, Chairman, Division of Clinical Pharmacology, Medical College of Virginia, Health Sciences Division of Virginia Commonwealth University, Richmond, Virginia JACK D. PROCTOR, M.D. Assistant Professor of Medicine, Medical College of Virginia, Health Sciences Division of Virginia Commonwealth University, Richmond, Virginia The electrophysiologic effects of the antiar adequate, controlled clinical comparisons are virtu rhythmic drugs, presented elsewhere in this sym ally nonexistent. posium, form only one of the bases for the selec A complete presentation of the non-electro tion of a therapeutic agent in any given clinical physiologic pharmacology would include the follow situation. The final choice depends at least on the ing considerations: following factors: 1. Absorption and peak effect times 1. The specific arrhythmia 2. Biotransformation 2. Underlying heart disease, if any 3. Rate of elimination or half-life (t1d 3. The degree of compromise of the circula 4. Drug interactions tion, if any 5. Toxicity 4. The etiology of the arrhythmia 6. Clinical usefulness 5. The efficacy of the drug for that arrhythmia 7. Therapeutic drug levels due to that etiology 8. Dosage schedules 6. The toxicity of the drug, especially in the As all of the above data cannot be presented in given patient with possible alterations in the limited space available, only selected items will volume of distribution, biotransformation, be discussed. Much of the preceding information and excretion is available, however, in standard texts ( 1 7, 10). 7. The electrophysiologic effects of the drug (See Addendum 1) 8. The routes and frequency of administration Quinidine. -

Adult Depression Clinical Practice Guidelines
NATIONAL CLINICAL PRACTICE GUIDELINE Adult Depression Clinical Practice Guideline This guideline is informational only. It is not intended or designed as a substitute for the reasonable exercise of independent clinical judgment by practitioners, considering each patient’s needs on an individual basis. Guideline recommendations apply to populations of patients. Clinical judgment is necessary to design treatment plans for individual patients. Approved by the National Guideline Directors February 2012 Table of Contents Introduction................................................................................................................................... 1 Guideline Summary...................................................................................................................... 5 Rationale Statements .................................................................................................................. 12 1. First-Line Treatment of Major Depressive Disorder (MDD) .............................................. 12 2. Hypericum (St. John’s Wort) for MDD............................................................................... 38 3. Antidepressants In Patients With MDD Expressing Suicidal Ideation, Intent, Or Plan...... 44 4. Second-Line Treatment Of MDD ........................................................................................ 48 5. Length Of Treatment With Antidepressants In Patients With MDD................................... 63 6. Follow-Up For Patients In The Acute Phase of Treatment For MDD................................ -

Treatment Considerations for Depression in Patients with Significant Medical Comorbidity
Treatment Considerations for Depression in Patients with Significant Medical Comorbidity David M. McCoy, MD Nashville, Tennessee In addition to being a strong psychological stressor in favors the use of selective serotonin reuptake inhibitors itself, medical illness is associated with risk factors that and other new antidepressants because they have fewer predispose patients to develop coexisting depression. anticholinergic, cardiac, or cognitive adverse effects. Patients with conditions such as cancer, cardiovascular Depressed medically ill patients clearly benefit from anti disease, and neurologic disorders are particularly prone depressant therapy. Because mental health influences to depression because these illnesses are severe, prognosis and treatment outcome, primary care physi chronic, and often fatal. Because an antidepressant may cians should maintain a high index of suspicion for exacerbate an underlying illness, leading to more seri depression in patients with significant medical illness ous side effects, agents with a poor tolerability profile or and aggressively treat the condition when indicated. that act at multiple receptor sites should be avoided. In many cases, this precludes the use of tricyclic antide KEY WORDS. Depression; comorbidity; drug therapy. J pressants and monoamine oxidase inhibitors, and Fam Pract 1996; 43(suppl):S35-S44 ajor depression is responsible for and treatment of depression in the family medicine more days in nonpsychiatric hospitals setting. and more days home from work than any other chronic illness except for RISK FACTORS severe, unstable coronary artery dis ease.1M Even though at least 8 million people in the Some medical disorders have clearly been associat United States become depressed in any given year,2 ed with higher incidences of depression. -

Phase I Safety, Pharmacokinetics, and Pharmacogenetics Study of the Antituberculosis Drug PA-824 with Concomitant Lopinavir-Ritonavir, Efavirenz, Or Rifampin
Phase I Safety, Pharmacokinetics, and Pharmacogenetics Study of the Antituberculosis Drug PA-824 with Concomitant Lopinavir-Ritonavir, Efavirenz, or Rifampin Kelly E. Dooley,a Anne F. Luetkemeyer,b Jeong-Gun Park,c Reena Allen,d Yoninah Cramer,c Stephen Murray,e Deborah Sutherland,f Francesca Aweeka,b Susan L. Koletar,g Florence Marzan,b Jing Bao,h Rada Savic,b David W. Haas,f the AIDS Clinical Trials Group A5306 Study Team Johns Hopkins University School of Medicine, Baltimore, Maryland, USAa; University of California, San Francisco, California, USAb; Statistical and Data Analysis Center, Harvard School of Public Health, Boston, Massachusetts, USAc; Social & Scientific Systems, Inc., Silver Spring, Maryland, USAd; Global Alliance for TB Drug Development, New York, New York, USAe; Vanderbilt University School of Medicine, Nashville, Tennessee, USAf; Ohio State University, Columbus, Ohio, USAg; Henry M. Jackson Foundation, Division of AIDS, National Institutes of Health, Bethesda, Maryland, USAh There is an urgent need for new antituberculosis (anti-TB) drugs, including agents that are safe and effective with concomitant antiretrovirals (ARV) and first-line TB drugs. PA-824 is a novel antituberculosis nitroimidazole in late-phase clinical develop- ment. Cytochrome P450 (CYP) 3A, which can be induced or inhibited by ARV and antituberculosis drugs, is a minor (ϳ20%) metabolic pathway for PA-824. In a phase I clinical trial, we characterized interactions between PA-824 and efavirenz (arm 1), lopinavir/ritonavir (arm 2), and rifampin (arm 3) in healthy, HIV-uninfected volunteers without TB disease. Participants in arms 1 and 2 were randomized to receive drugs via sequence 1 (PA-824 alone, washout, ARV, and ARV plus PA-824) or sequence 2 (ARV, ARV with PA-824, washout, and PA-824 alone).