Neurobiology of Visceral Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Sympathetic and the Parasympathetic Nervous System
The sympathetic and the parasympathetic nervous system Zsuzsanna Tóth, PhD Institute of Anatomy, Histology and Embryology Semmelweis University The role of the autonomic nervous system Claude Bernard • „milieu intérieur” concept; every organism lives in its internal environment that is constant and independent form the external environment Walter Bradford Cannon homeostasis; • an extension of the “milieu interieur” concept • consistence in an open system requires mechanisms that act to maintain that consistency • steady-state conditions require that any tendency toward change automatically meets with factors that resist that change • regulating systems that determine the homeostatic state : o autonomic nervous system ( sympathetic, parasympathetic, enteral) o endocrine system General structure of the autonomic nervous system craniosacral thoracolumbar Anatomy Neurotransmittersof the gut autonomic nervous system. symp. gangl pregangl. fiber pregangl. postgangl. fiber fiber (PoR) PoR enteral ganglion PoR PoR smooth muscle smooth muscle Kuratani S Development 2009;136:1585-1589 Sympathetic activation: Fight or flight reaction • energy mobilization • preparation for escape, or fight vasoconstriction • generalized Parasympathetic activation: adrenal • energy saving and restoring • „rest and digest” system • more localized vasoconstriction Paravertebral ganglia and the sympathetic chains pars cervicalis superius ganglion medium cervicale stellatum pars vertebrae • from the base of the skull to the caudal end thoracalis thoracalis of the sacrum • paravertebral ganglia (ganglia trunci sympathici) • rami interganglionares pars vertebrae • the two chains fuses at the ganglion impar abdominalis lumbalis sacrum pars pelvina foramen sacralia anteriora ganglion impar Anatomy of the cervical part of the sympathetic trunk superior cervical ganglion • behind the seath of the carotid, fusiform ggl. cervicale superius • IML T1-3 vegetative motoneurons- preganglionic fibers truncus symp. -
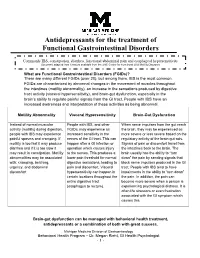
Antidepressants for Functional Gastrointestinal Disorders
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

Managing Cancer Pain
The British Pain Society's Managing cancer pain - information for patients From the British Pain Society, supported by the Association of Palliative Medicine and the Royal College of General Practitioners January 2010 To be reviewed January 2013 2 Cancer Pain Management Published by: The British Pain Society 3rd floor Churchill House 35 Red Lion Square London WC1R 4SG Website: www.britishpainsociety.org ISBN: 978-0-9551546-8-3 © The British Pain Society 2010 Information for Patients 3 Contents Page What can be done for people with cancer pain 4 Understanding cancer pain 4 Knowing what to expect 6 Options for pain control – most pain can be controlled 6 Coping with cancer pain 8 Describing pain – communicating with your doctors 9 Talking to others with cancer pain 12 Finding help managing cancer pain 12 References 12 Methods 12 Competing Interests 13 Membership of the group and expert contributors 13 4 Cancer Pain Management What can be done for people with cancer pain? There are medicines and expertise available that can help to control cancer pain. However, surveys show that cancer pain is still poorly controlled in many cases. As a result, patients must know what is available, what they have a right to and how to ask for it. Cancer itself and the treatments for cancer, including both medicines and surgery, can cause pain. Treatments can be directed either at the cause of the pain (for example, the tumour itself) or at the pain itself. Understanding cancer pain Cancer pain can be complicated, involving pain arising from inflammation (swelling), nerve damage and tissue damage from many sites around the body. -

Association of Arrhythmia in Patients with Cervical Spondylosis: a Nationwide Population-Based Cohort Study
Journal of Clinical Medicine Article Association of Arrhythmia in Patients with Cervical Spondylosis: A Nationwide Population-Based Cohort Study Shih-Yi Lin 1,2, Wu-Huei Hsu 1,3, Cheng-Chieh Lin 1,4, Cheng-Li Lin 5,6, Chun-Hao Tsai 1,7, Chih-Hsueh Lin 1,4, Der-Cherng Chen 7, Tsung-Chih Lin 8, Chung-Y. Hsu 1 and Chia-Hung Kao 1,9,10,* ID 1 Graduate Institute of Biomedical Sciences and School of Medicine, College of Medicine, China Medical University, No. 2, Yuh-Der Road, Taichung 404, Taiwan; [email protected] (S.-Y.L.); [email protected] (W.-H.H.); [email protected] (C.-C.L.); [email protected] (C.-H.T.); [email protected] (C.-H.L.); [email protected] (C.-Y.H.) 2 Division of Nephrology and Kidney Institute, China Medical University Hospital, Taichung 404, Taiwan 3 Division of Pulmonary and Critical Care Medicine, China Medical University Hospital and China Medical University, Taichung 404, Taiwan 4 Department of Family Medicine, China Medical University Hospital, Taichung 404, Taiwan 5 Management Office for Health Data, China Medical University Hospital, Taichung 404, Taiwan; [email protected] 6 College of Medicine, China Medical University, Taichung 404, Taiwan 7 Department of Orthopedics, China Medical University Hospital, Taichung 404, Taiwan; [email protected] 8 Department of Orthopedics, St. Martin De Porres Hospital, Chiayi 600, Taiwan; [email protected] 9 Department of Nuclear Medicine, China Medical University Hospital, Taichung 404, Taiwan 10 Department of Bioinformatics and Medical Engineering, Asia University, Taichung 413, Taiwan * Correspondence: [email protected]; Tel.: +886-4-2205-2121 (ext. -

THE MAIN PERIPHERAL CONNECTIONS of the HUMAN SYMPATHETIC NERVOUS SYSTEM by T
THE MAIN PERIPHERAL CONNECTIONS OF THE HUMAN SYMPATHETIC NERVOUS SYSTEM By T. K. POTTS, M.B., CH.M. (SYDNEY)1 BIIE recent investigation (5,7) of the functional significance of the sympathetic system by 1)r N. D). itoyle and Professor J. I. Hunter has revealed the necessity for a re-examination of the anatomy of the human sympathetic system. Ini particular the operations of ramisectioni (7, 8) devised by Dr Royle, in collabora- tion with Professor Hunter, call for a more exact determination of the precise position and topographical relations of the sympathetic cord and its ram? cotitnunicantes than at present is available. The dissection described ill this note was undertaken primarily to provide the surgeon with this guidance. In this matter, two regions stand out as having assumed an added interest ill the light of recent research. I refer to those regions associated with the operations known as cervical, and lumbar sympathetic ramisection, which are performed to remove the rigidity of the musculature of the extremities ill spastic paralysis (2,3,4,5, 7, 8, 9,10). As a description of the rari commnunicantes necessarily involves some mention of the arrangement of corresponding ganglia, this will be done in considering the various regions. To facilitate demonstration, the services of Miss D. Harrison were procured and, under my guidance, faithful repro- dluetions of the dissection were made by her. The dissection has been mounted, and placed in the Wilson. Museum of Anatomy, at the Medical School, Uni- versity of Sydney. The cervical portion of the sympathetic is characterized by the absence of segmental ganglia, and of white rami comnimunicantes. -

Sympathetic Tales: Subdivisons of the Autonomic Nervous System and the Impact of Developmental Studies Uwe Ernsberger* and Hermann Rohrer
Ernsberger and Rohrer Neural Development (2018) 13:20 https://doi.org/10.1186/s13064-018-0117-6 REVIEW Open Access Sympathetic tales: subdivisons of the autonomic nervous system and the impact of developmental studies Uwe Ernsberger* and Hermann Rohrer Abstract Remarkable progress in a range of biomedical disciplines has promoted the understanding of the cellular components of the autonomic nervous system and their differentiation during development to a critical level. Characterization of the gene expression fingerprints of individual neurons and identification of the key regulators of autonomic neuron differentiation enables us to comprehend the development of different sets of autonomic neurons. Their individual functional properties emerge as a consequence of differential gene expression initiated by the action of specific developmental regulators. In this review, we delineate the anatomical and physiological observations that led to the subdivision into sympathetic and parasympathetic domains and analyze how the recent molecular insights melt into and challenge the classical description of the autonomic nervous system. Keywords: Sympathetic, Parasympathetic, Transcription factor, Preganglionic, Postganglionic, Autonomic nervous system, Sacral, Pelvic ganglion, Heart Background interplay of nervous and hormonal control in particular The “great sympathetic”... “was the principal means of mediated by the sympathetic nervous system and the ad- bringing about the sympathies of the body”. With these renal gland in adapting the internal -

CVM 6100 Veterinary Gross Anatomy
2010 CVM 6100 Veterinary Gross Anatomy General Anatomy & Carnivore Anatomy Lecture Notes by Thomas F. Fletcher, DVM, PhD and Christina E. Clarkson, DVM, PhD 1 CONTENTS Connective Tissue Structures ........................................3 Osteology .........................................................................5 Arthrology .......................................................................7 Myology .........................................................................10 Biomechanics and Locomotion....................................12 Serous Membranes and Cavities .................................15 Formation of Serous Cavities ......................................17 Nervous System.............................................................19 Autonomic Nervous System .........................................23 Abdominal Viscera .......................................................27 Pelvis, Perineum and Micturition ...............................32 Female Genitalia ...........................................................35 Male Genitalia...............................................................37 Head Features (Lectures 1 and 2) ...............................40 Cranial Nerves ..............................................................44 Connective Tissue Structures Histologic types of connective tissue (c.t.): 1] Loose areolar c.t. — low fiber density, contains spaces that can be filled with fat or fluid (edema) [found: throughout body, under skin as superficial fascia and in many places as deep fascia] -

Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gutlbrain Interaction): a Rome Foundation Working Team Report Douglas A
Gastroenterology 2018;154:1140–1171 SPECIAL REPORT Neuromodulators for Functional Gastrointestinal Disorders (Disorders of GutLBrain Interaction): A Rome Foundation Working Team Report Douglas A. Drossman,1,2 Jan Tack,3 Alexander C. Ford,4,5 Eva Szigethy,6 Hans Törnblom,7 and Lukas Van Oudenhove8 1Center for Functional Gastrointestinal and Motility Disorders, University of North Carolina, Chapel Hill, North Carolina; 2Center for Education and Practice of Biopsychosocial Care and Drossman Gastroenterology, Chapel Hill, North Carolina; 3Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium; 4Leeds Institute of Biomedical and Clinical Sciences, University of Leeds, Leeds, United Kingdom; 5Leeds Gastroenterology Institute, St James’s University Hospital, Leeds, United Kingdom; 6Departments of Psychiatry and Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania; 7Departments of Internal Medicine and Clinical Nutrition, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; and 8Laboratory for BrainÀGut Axis Studies, Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium BACKGROUND & AIMS: Central neuromodulators (antide- summary information and guidelines for the use of central pressants, antipsychotics, and other central nervous neuromodulators in the treatment of chronic gastrointestinal systemÀtargeted medications) are increasingly used for treat- symptoms and FGIDs. Further studies are needed to confirm ment -

The Axatomy of the Autonomic Nervous System in the Dog1
THE AXATOMY OF THE AUTONOMIC NERVOUS SYSTEM IN THE DOG1 NICHOLAS JAMES AIIZERES Ucpartnitiit of Aiintoiiry, Cnzvemtty of Xtclizgaii Scliool of ;2/cdicmc. Ann Arbor, Mtclatgan ELEVEN FIGURES INTRODUCTTOX I<iiowledgc clerivccl from cmprimeiits on tlie clog has not infrequently been applied to man without considering dif- fcmnccs in aiiatoniy. This is c~spcciallytrue of the autonomic nervous systeni, oiily parts of which have b:mi described in the adult clog. The cardiac ncli'vcs \\'ere described by Sc1iuran.- Iew ( '27) ant1 Soniclez ( '39), the gcw~alplan of the abrloniirial ancl sacral regions by Trumble ( '34), tlic lunibosacral trunk by Alehler, Fisclier and Alexander ( '52), the vagi lsy Hilsa- beck aid Hill ( '50) and BIcC'rca and D'hrcy ( '%), ant1 the urogenital plexuses by Schal~adasch( '26) aiicl Ncdowar ( '2.3. The present study was undertaken to fill gaps in previous clescriptions ancl to present an over-all view of the autonomic iierrous system in the (log, esclutliiig the cephalic region. In the pi-c~seiitiiivcstigation the XI< terminology has been used iiistpad of the usual RNA familiar in human anatomy loccause tlic study was based on the clog. Sincc a dog is a pronograde niamnial the terms cranial aiid caudal seeni nior(t appropriat r tliaii the ESA terms superior and inferior. Tiiis paper is n condensation of a clissei t:ition snbniittctl in paytial fulfillmc.~it of tlrc rcqiiireiiieuts for the drgrce of Doctor of Pliilosopliy in the University of Rlicliigaii. I wish to tlimik Dr. It. T. Wootlhuine for Ills interest and aclriec. For the supply of nlatciial tlie author vihlies to e\-pr('\s his appreciatioir to mcmbc~is of the 1)ep:irtiiiciits of P1iTsiolog.y :iiiil PIiar~u:~cologrof tlic Viiirersity of hliclrigan. -

Abdominal Visceral Pain: Clinical Aspect*
Rev Dor. São Paulo, 2013 out-dez;14(4):311-4 ARTIGO DE REVISÃO Abdominal visceral pain: clinical aspects* Dor visceral abdominal: aspectos clínicos Telma Mariotto Zakka1, Manoel Jacobsen Teixeira1, Lin Tchia Yeng1 *Recebido do Centro Interdisciplinar de Dor do Hospital de Clínicas da Faculdade de Medicina / Universidade de São Paulo. São Paulo, SP, Brasil. ABSTRACT CONTEÚDO: Como as doenças viscerais podem determinar dores de vários tipos e, habitualmente, desafiam os médicos no seu diagnós- BACKGROUND AND OBJECTIVES: Abdomen is the most fre- tico e tratamento, os autores descreveram de forma prática, as carac- quent site for acute or chronic painful syndromes, for referred pain terísticas dolorosas e as associações com as doenças mais incidentes. from distant structures or for pain caused by systemic injuries. Ab- CONCLUSÃO: O tratamento interdisciplinar com a associação das dominal visceral pain is induced by hollow viscera or parenchymal medidas farmacológicas aos procedimentos de medicina física e rea- viscera walls stretching or by peritoneal stretching. Complex diag- bilitação e ao acompanhamento psicológico diminui o sofrimento e nosis and treatment have motivated this study. Patients with chronic as incapacidades e melhora a qualidade de vida. abdominal pain are usually undertreated and underdiagnosed. The Descritores: Dor abdominal, Dor miofascial, Dor visceral, Trata- interdisciplinary treatment aims at minimizing patients’ distress, re- mento interdisciplinar. lieving pain and improving their quality of life. CONTENTS: Since visceral diseases may determine pain of different INTRODUÇÃO types and, usually, challenge physicians with regard to their diagnosis and treatment, the authors have described in a practical way painful A dor visceral pode decorrer por tensão ou estiramento da parede characteristics and associations with more common diseases. -

Clinical Evidence on Visceral Pain. Systematic Review Evidência Clínica Sobre Dor Visceral
Rev Dor. São Paulo, 2017 jan-mar;18(1):65-71 REVIEW ARTICLE Clinical evidence on visceral pain. Systematic review Evidência clínica sobre dor visceral. Revisão sistemática Durval Campos Kraychete1, José Tadeu Tesseroli de Siqueira2, João Batista Garcia3, Rioko Kimiko Sakata4, Ângela Maria Sousa5, Daniel Ciampi de Andrade6, Telma Regina Mariotto Zakka7, Manoel Jacobsen Teixeira7 and Diretoria da Sociedade Brasileira para o Estudo da Dor de 2015 DOI 10.5935/1806-0013.20170014 ABSTRACT RESUMO BACKGROUND AND OBJECTIVES: Visceral pain is in- JUSTIFICATIVA E OBJETIVOS: A dor visceral é causada por duced by abnormalities of organs such as stomach, kidneys, anormalidades de órgãos como o estômago, rim, bexiga, vesícula bladder, gallbladder, intestines and others and includes disten- biliar, intestinos ou outros e inclui distensão, isquemia, inflama- sion, ischemia, inflammation and mesenteric traction. It is re- ção e tração do mesentério. É responsável por incapacidade física sponsible for physical and psychic incapacity, absenteeism and e psíquica, absenteísmo do trabalho e má qualidade de vida. O poor quality of life. This study aimed at discussing major aspects objetivo deste estudo foi discutir os principais aspectos da dor of visceral pain with regard to prevalence, etiology and diagnosis. visceral relacionados a prevalência, etiologia e diagnóstico. CONTENTS: According to Evidence-Based Medicine concepts, CONTEÚDO: Foram revisados segundo os preceitos da Medic- visceral pain etiology, diagnosis and prognosis were reviewed in ina Baseada em Evidência os enfoques etiológicos, diagnóstico LILACS, EMBASE and Pubmed databases. Therapeutic stud- e prognóstico da dor visceral nas bases de indexações biomédi- ies were not selected. The following terms were used as search cas, LILACS, EMBASE e Pubmed. -

Milnacipran, a Serotonin and Norepinephrine Reuptake Inhibitor: a Novel Treatment for Fibromyalgia
Drug Evaluation Milnacipran, a serotonin and norepinephrine reuptake inhibitor: a novel treatment for fibromyalgia Milnacipran hydrochloride is a serotonin (5-HT) and norepinephrine (NE) reuptake inhibitor that was recently approved by the US FDA for the treatment of fibromyalgia (FM). Evidence has accumulated suggesting that, in animal models, milnacipran may exert pain-mitigating influences involving norepinephrine- and serotonin-related processes at supraspinal, spinal and peripheral levels in pain transmission. Milnacipran has demonstrated efficacy for the reduction of pain as well as improvements in global assessments of well-being and functional capacity among treated FM patients. Its role in addressing comorbidities associated with FM, including visceral pain and migraine, has, as yet, to be investigated. Milnacipran may be of special interest for use in patients for whom hepatic dysfunction precludes the use of other agents, for example, duloxetine. It has a negligible influence on cytochrome metabolism, and therefore may be of particular benefit in patients requiring multiple concurrently prescribed medications. Milnacipran may comprise a reasonable option in the armamentarium of treatments available to manage FM. KEYWORDS: antidepressants n chronic pain n fibromyalgian milnacipran n serotonin Raphael J Leo and norepinephrine reuptake inhibitor Department of Psychiatry, School of Medicine and Fibromyalgia (FM) is a syndrome characterized Several pharmacological approaches have Biomedical Sciences, by chronic, widespread musculoskeletal pain and been advocated for the treatment of FM. State University of New York at tenderness. The prevalence of FM in the general Because of their impact on these presump- Buffalo, Erie County Medical population is estimated to be 2–4%; it tends to tive pathophysiologic processes, antidepres- Center, 462 Grider Street, show a female predilection, and increases with sants have frequently been advocated for Buffalo, NY 14215, USA age [1,2].