Differential Diagnosis of Chest Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Musculoskeletal Diagnosis Utilizing History and Physical Examination: Focus on Spine
NYU Long Island School of Medicine MUSCULOSKELETAL DIAGNOSIS UTILIZING HISTORY AND PHYSICAL EXAMINATION: FOCUS ON SPINE Ralph K. Della Ratta, MD, FACP Kevin J. Curley, MD, FACP Division of General Internal Medicine, NYU Winthrop Hospital NYU Long Island School of Medicine, SUNY Stony Brook School of Medicine Board Certified in IM and Primary Care Sports Medicine Learning Objectives 1. Identify components of the focused history and physical examination that will guide musculoskeletal diagnosis 2. Utilize musculoskeletal examination provocative maneuvers to aide differential diagnosis 3. Review the evidence base (likelihood ratios etc.) that is known about musculoskeletal physical examination 2 NYU Long Island School of Medicine * ¾ of medical diagnoses are still made on history and exam despite technological Musculoskeletal Physical Exam advances of modern medicine • Physical examination is key to musculoskeletal diagnosis • Unlike many other organ systems, the diagnostic standard for many musculoskeletal disorders is the exam finding (e.g. diagnosis of epicondylitis, see below) • “You may think you have not seen it, but it has seen you!” Lateral Epicondylitis confirmed on exam by reproducing pain at lateral epicondyle with resisted dorsiflexion at wrist **not diagnosed with imaging** 3 NYU Long Island School of Medicine Musculoskeletal Physical Exam 1. Inspection – symmetry, swelling, redness, deformity 2. Palpation – warmth, tenderness, crepitus, swelling 3. Range of motion *most sensitive for joint disease Bates Pocket Guide to Physical -

EPA Quick Reference Guide
EPA Quick Reference Guide EPAs 1 & 2 – Professionalism Unacceptable • Unreliable • Dishonest • Avoids responsibility • Commitment uncertain • Dresses inappropriately • Unexplained absences • Verbal and non-verbal disrespect towards preceptor • Does not recognize own limitations and the need to seek assistance • Unable to comprehend the point of view and emotional state of other people • Judgmental of others • Fails to recognize and respect cross-cultural and gender differences Minimally Competent • Sometimes late • Not consistently able to complete assignments or tasks • Not consistently considerate of the feelings and emotional needs of others • Sometimes judgmental Competent • Punctual • Dependable • Accepts responsibilities • Demonstrates a willingness to accept feedback regarding necessary change(s) • Appropriately shows concern for others’ feelings and interacts accordingly • Recognizes and respects cross-cultural and gender differences Office of Medical Education 306 Liberty View Lane, Lynchburg, Va. 24502 [email protected] EPAs 3 & 4 – Data Gathering / Interviewing & Physical Examination Skills Unacceptable • Inefficient, disorganized • Weak prioritization skills • Misses major findings • Fails to appreciate physical findings and pertinent information • History and/or physical exam incomplete or inaccurate • Insufficient attention to psychosocial issues • Needs to work on establishing rapport with patients • Needs to work on awareness of appropriate boundaries with patients • Needs to improve demonstration of compassion • -
Clinical Reasoning - the Process of Thinking and Decision Making, Consciously & Unconsciously Guide Practice Actions
Diagnostic Reasoning “DR” Toolbox for Hospitalist Faculty Heather Hofmann, MD Department of Medicine 2017-18 2 Goal Increase faculty familiarity with diagnostic reasoning principles and tools so as to improve its teaching. Three Parts: I: Introduction to Diagnostic Reasoning II: DR Toolbox III: Structured Reflection Exercise (SRE) 4 Part I: Introduction to Diagnostic Reasoning Learning Objectives - Understand the “what” and “why” of Diagnostic Reasoning - Recognize dual-process theory’s role in “how” we reason 6 What is Diagnostic Reasoning? - Clinical reasoning - The process of thinking and decision making, consciously & unconsciously guide practice actions 25yo female G1P0, 2m gestation returns from Rio. - Diagnostic reasoning: - The process of collecting & analyzing information establish a diagnosis chest pain STEMI in proximal LAD abdominal pain acute appendicitis 7 Why teach diagnostic reasoning? - Incorrect diagnoses are often at the root of medical errors - DR is a means to apply basic science to clinical problems - Central to being a physician 8 Patient’s perspective What’s wrong with me? Is it bad? What can we do about it? 9 Why now? Never too early for practice 10 From Novice to Expert 11 How do we reason? Information processing theory 12 How do we reason? Information processing theory: Dual process theory. Analytical Non-analytical Conscious Unconscious Type/System 2 Type/System 1 Slow Fast Effortful Automatic Deliberative Involuntary Logical Emotional Requires attention, Executes skilled self-control, time. response and -

Respiratory Mechanics and Breathing Pattern T Jacopo P
Respiratory Physiology & Neurobiology 261 (2019) 48–54 Contents lists available at ScienceDirect Respiratory Physiology & Neurobiology journal homepage: www.elsevier.com/locate/resphysiol How to breathe? Respiratory mechanics and breathing pattern T Jacopo P. Mortola Department of Physiology, McGill University, 3655 Promenade Sir William Osler, room 1121, Montreal, Quebec, H3G 1Y6, Canada ARTICLE INFO ABSTRACT Keywords: On theoretical grounds any given level of pulmonary or alveolar ventilation can be obtained at various absolute Allometry lung volumes and through many combinations of tidal volume, breathing frequency and inspiratory and ex- Breathing frequency piratory timing. However, inspection of specific cases of newborn and adult mammals at rest indicates thatthe Human infant breathing pattern reflects a principle of economy oriented toward minimal respiratory work. The mechanisms Neonatal respiration that permit optimization of respiratory cost are poorly understood; yet, it is their efficiency and coordination that Work of breathing permits pulmonary ventilation at rest to require only a minimal fraction of resting metabolism. The sensitivity of the breathing pattern to the mechanical properties implies that tidal volume, breathing rate, mean inspiratory flow or other ventilatory parameters cannot be necessarily considered indicators proportional to thecentral neural respiratory ‘drive’. The broad conclusion is that the breathing pattern adopted by newborn and adult mammals is the one that produces the adequate alveolar ventilation -

Sleep Apnea Sleep Apnea
Health and Safety Guidelines 1 Sleep Apnea Sleep Apnea Normally while sleeping, air is moved at a regular rhythm through the throat and in and out the lungs. When someone has sleep apnea, air movement becomes decreased or stops altogether. Sleep apnea can affect long term health. Types of sleep apnea: 1. Obstructive sleep apnea (narrowing or closure of the throat during sleep) which is seen most commonly, and, 2. Central sleep apnea (the brain is causing a change in breathing control and rhythm) Obstructive sleep apnea (OSA) About 25% of all adults are at risk for sleep apnea of some degree. Men are more commonly affected than women. Other risk factors include: 1. Middle and older age 2. Being overweight 3. Having a small mouth and throat Down syndrome Because of soft tissue and skeletal alterations that lead to upper airway obstruction, people with Down syndrome have an increased risk of obstructive sleep apnea. Statistics show that obstructive sleep apnea occurs in at least 30 to 75% of people with Down syndrome, including those who are not obese. In over half of person’s with Down syndrome whose parents reported no sleep problems, sleep studies showed abnormal results. Sleep apnea causing lowered oxygen levels often contributes to mental impairment. How does obstructive sleep apnea occur? The throat is surrounded by muscles that are active controlling the airway during talking, swallowing and breathing. During sleep, these muscles are much less active. They can fall back into the throat, causing narrowing. In most people this doesn’t affect breathing. However in some the narrowing can cause snoring. -

Respiratory Issues in Rett Syndrome Dr. Marianna Sockrider, Pediatric
RettEd Q&A: Respiratory Issues in Rett Syndrome Dr. Marianna Sockrider, Pediatric Pulmonologist, Texas Children's Hospital Webcast 02/13/2018 Facilitator: Paige Nues, Rettsyndrome.org Recording link: https://register.gotowebinar.com/recording/1810253924903738120 Attendee Questions Response Breathing Irregularities Why is breathing so funny when our girls/ A behavioral arousal can trigger breathing abnormalities in Rett boys wake up, almost as if startled? syndrome. A person goes through stages of sleep and particularly if aroused from a deep sleep state (REM) may be more disoriented or startled. This can trigger the irregular breathing. Could she address the stereotypical You may observe breathing abnormalities like breath holding breathing abnormalities such as gasping and hyperventilation more with the stress of an acute and breath holding and how they play a respiratory illness. Breath holding and hyperventilation do not part in respiratory illness? directly cause respiratory illness. If a person has difficulty with swallowing and has these breathing episodes while trying to eat or drink, aspiration could occur which can cause respiratory symptoms. If one has very shallow breathing, especially when there is more mucus from acute infection, it may be more likely to build up in the lower lungs causing airway obstruction and atelectasis (collapse of some air sacs). Is there any evidence (even anecdotal) Frequent breath-holding and hyperventilation has been Reference 1 that breathing patterns change in Rett reported to become less evident with increasing age though it is patients over time? not certain whether this could be that families are used to the irregular breathing and don’t report it as much or that it is the people who live longer who are less symptomatic. -
Dyspnoea and Its Measurement
REVIEW Key points Dyspnoea is the sensation of breathing discom- fort that can be described with different terms according to different pathophysiological mechanisms that vary in intensity. The mechanisms of dyspnoea are complex. In COPD, whilst the intensity and quality of dys- pnoea during activity correlates with the magni- tude of lung hyperinflation and inspiratory events, it correlates poorly with FEV1. Valid, reliable and responsive instruments are available to measure the severity of dyspnoea in patients with respiratory disease. 100 Breathe | December 2004 | Volume 1 | No 2 REVIEW N. Ambrosino1 Dyspnoea and its G. Scano2 measurement 1 Pulmonary Unit, Cardio-Thoracic Dept, University-Hospital Pisa, Pisa, and 2Clinica Medica, University-Hospital Careggi, CME article: educational aims Firenze, Italy. To introduce dyspnoea and explain its mechanisms. Correspondence: To present dyspnoea descriptors, which may help in the understanding of the language of N. Ambrosino dyspnoea, and to relate these to specific diseases. Pulmonary Unit To describe some of the methods available for the measurement of dyspnoea. Cardio-Thoracic Dept Azienda Ospedaliera-Universitaria Pisana Via Paradisa 2, Cisanello Summary 56124 Pisa Italy Fax: 39 50996786 Dyspnoea, a term used to characterise a subjective experience of breathing discomfort, is E-mail: perhaps the most important symptom in cardiorespiratory disease. Receptors in the air- [email protected] ways, lung parenchyma, respiratory muscles and chemoreceptors provide sensory feed- back via vagal, phrenic and intercostal nerves to the spinal cord, medulla and higher cen- tres. Knowledge of dyspnoea descriptors can help in understanding the language of dys- pnoea and these are presented here. It is important to appreciate that differences in lan- guage, race, culture, sex and previous experience can all change the perception of and the manner in which the feeling of being dyspnoeic is expressed to others. -
Antidepressants for Functional Gastrointestinal Disorders
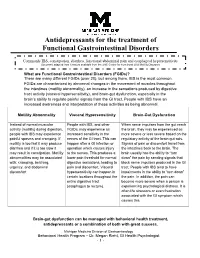
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

Managing Cancer Pain
The British Pain Society's Managing cancer pain - information for patients From the British Pain Society, supported by the Association of Palliative Medicine and the Royal College of General Practitioners January 2010 To be reviewed January 2013 2 Cancer Pain Management Published by: The British Pain Society 3rd floor Churchill House 35 Red Lion Square London WC1R 4SG Website: www.britishpainsociety.org ISBN: 978-0-9551546-8-3 © The British Pain Society 2010 Information for Patients 3 Contents Page What can be done for people with cancer pain 4 Understanding cancer pain 4 Knowing what to expect 6 Options for pain control – most pain can be controlled 6 Coping with cancer pain 8 Describing pain – communicating with your doctors 9 Talking to others with cancer pain 12 Finding help managing cancer pain 12 References 12 Methods 12 Competing Interests 13 Membership of the group and expert contributors 13 4 Cancer Pain Management What can be done for people with cancer pain? There are medicines and expertise available that can help to control cancer pain. However, surveys show that cancer pain is still poorly controlled in many cases. As a result, patients must know what is available, what they have a right to and how to ask for it. Cancer itself and the treatments for cancer, including both medicines and surgery, can cause pain. Treatments can be directed either at the cause of the pain (for example, the tumour itself) or at the pain itself. Understanding cancer pain Cancer pain can be complicated, involving pain arising from inflammation (swelling), nerve damage and tissue damage from many sites around the body. -
Diagnosis and Management of Chlamydia: a Guide for Gps
■ PRESCRIBING IN PRACTICE Diagnosis and management of chlamydia: a guide for GPs ELEANOR DRAEGER SPL Chlamydia is a common sexually- transmitted infection caused by Chlamydia trachomatis bacteria. This article discusses its diagnosis and treatment, and considers the GP’s role in management. hlamydia is the most common sexually-transmitted infection C(STI) in the UK, with 203,116 new diagnoses in England in 2017, of which 126,828 (62%) were in young people aged 15–24 years.1 Chlamydia is transmitted primarily through penetrative sex and infects the urethra and endocervix. It can also infect the throat and the rectum, and in some cases the conjunctiva. It is very infectious, with a concordance of up to 75% between sexual partners. There are many risk factors for chlamydia infection, including being under the age of 25 years, having a new sexual partner and inconsistent use of condoms. If a woman contracts chlamydia during pregnancy it can be transmitted to the baby at delivery, causing conjunctivitis or pneumonia. Classification of chlamydia infections There are three species of chlamydia bacteria that can cause disease in humans: • Chlamydia psittaci – the natural host is birds, especially par- rots, but it can be transmitted to humans, causing psittacosis • Chlamydia pneumoniae – causes respiratory disease in humans • Chlamydia trachomatis – several different serovars can cause disease (including STIs) in humans, as detailed in Figure 1. Symptoms The majority of genital chlamydia infections are asymptomatic, but they can cause significant symptoms. In women, chlamydia can cause vaginal discharge, dysuria, abdominal and pelvic pain, post-coital and intermenstrual bleeding, and deep dys- pareunia. -

Influence of Exercise and C02 on Breathing Pattern in Patients with Chronic Obstructive Lung Disease (COLD)
Eur Respir J 1988, 1, 139-144 Influence of exercise and C02 on breathing pattern in patients with chronic obstructive lung disease (COLD) G. Scano*, F. Gigliotti*, A. van Meerhaeghe**, A. De Coster**, R. Sergysels** Influence of exercise and C02 on breathing pattern in patients with chronic • Clinica Medica III, Universita di Firenze, obstructive lung disease (COLD). G. Scano, F. Gigliotti, A. van Meerhaeghe. Italy. A. De Coster, R. Sergyse/s. •• Pulmonary Division, Hopital Universitaire ABSTRACT: In ten eucapnic patients with chronic obstructive lung disease St. Pierre (ULB), Brussels, Belgium. (COLD) we evaluated the breathing pattern during induced progressive Keywords: Breathing pattern; exercise; COPD; hypercapnia (C0 rebreathing) and progressive exercise on an ergometric 1 col rebreathing. bicycle (30 W /3 min). The time and volume components of the respiratory cycle were measured breath by breath. When compared to hypercapnia, the increase Received: January 30, 1987; accepted after in ventilation (VE) during exercise was associated with a smaDer increase in revision: September 17, 1987. tidal volume (VT) and a greater increase in respiratory frequency (fl). Plots of tidal volume (VT) against both inspiratory time (Tt) and expiratory time (TE) showed a greater decrease in both TI and TE during exercise than with hypercapnia. Analysis of YE in terms of flow (VT/TI) and timing (Tt/'I'r) showed VE to increase by a similar increase to that in VT/TI during both exerci.se and hypercapnia, while Tt/TT did not change significantly. When the patients were matched for a given VE (28 I· min -J ), exercise induced a smaller increase in VT (p < 0.05), a greater increase in fl (p < 0.025); Tl (p < 0.025) and TE (p < 0.01) were found to be smaller during exercise than hypercapnia. -

The Contribution of the Medical History for the Diagnosis of Simulated Cases by Medical Students
International Journal of Medical Education. 2012;3:78-82 ISSN: 2042-6372 DOI: 10.5116/ijme.4f8a.e48c The contribution of the medical history for the diagnosis of simulated cases by medical students Tomoko Tsukamoto, Yoshiyuki Ohira, Kazutaka Noda, Toshihiko Takada, Masatomi Ikusaka Department of General Medicine, Chiba University Hospital, Japan Correspondence: Tomoko Tsukamoto, Department of General Medicine, Chiba University Hospital, 1-8-1 Inohana, Chuo-ku, Chiba city, Chiba, 260-8677 Japan. Email: [email protected] Accepted: April 15, 2012 Abstract Objectives: The case history is an important part of diag- rates were compared using analysis of the χ2-test. nostic reasoning. The patient management problem method Results: Sixty students (63.8%) made a correct diagnosis, has been used in various studies, but may not reflect the which was based on the history in 43 students (71.7%), actual reasoning process because a list of choices is given to physical findings in 11 students (18.3%), and laboratory the subjects in advance. This study investigated the contri- data in 6 students (10.0%). Compared with students who bution of the history to making the correct diagnosis by considered the correct diagnosis in their differential diagno- using clinical case simulation, in which students obtained sis after taking a history, students who failed to do so were clinical information by themselves. 5.0 times (95%CI = 2.5-9.8) more likely to make a final Methods: A prospective study was conducted. Ninety-four misdiagnosis (χ2(1) = 30.73; p<0.001). fifth-year medical students from Chiba University who Conclusions: History taking is especially important for underwent supervised clinical clerkships in 2009 were making a correct diagnosis when students perform clinical surveyed.