OPQRST-AAA One Tool That Some Clinicians Find Helpful Is Using the Mnemonic OPQRST-AAA to Elicit the Details of a Pain Complaint
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Musculoskeletal Diagnosis Utilizing History and Physical Examination: Focus on Spine
NYU Long Island School of Medicine MUSCULOSKELETAL DIAGNOSIS UTILIZING HISTORY AND PHYSICAL EXAMINATION: FOCUS ON SPINE Ralph K. Della Ratta, MD, FACP Kevin J. Curley, MD, FACP Division of General Internal Medicine, NYU Winthrop Hospital NYU Long Island School of Medicine, SUNY Stony Brook School of Medicine Board Certified in IM and Primary Care Sports Medicine Learning Objectives 1. Identify components of the focused history and physical examination that will guide musculoskeletal diagnosis 2. Utilize musculoskeletal examination provocative maneuvers to aide differential diagnosis 3. Review the evidence base (likelihood ratios etc.) that is known about musculoskeletal physical examination 2 NYU Long Island School of Medicine * ¾ of medical diagnoses are still made on history and exam despite technological Musculoskeletal Physical Exam advances of modern medicine • Physical examination is key to musculoskeletal diagnosis • Unlike many other organ systems, the diagnostic standard for many musculoskeletal disorders is the exam finding (e.g. diagnosis of epicondylitis, see below) • “You may think you have not seen it, but it has seen you!” Lateral Epicondylitis confirmed on exam by reproducing pain at lateral epicondyle with resisted dorsiflexion at wrist **not diagnosed with imaging** 3 NYU Long Island School of Medicine Musculoskeletal Physical Exam 1. Inspection – symmetry, swelling, redness, deformity 2. Palpation – warmth, tenderness, crepitus, swelling 3. Range of motion *most sensitive for joint disease Bates Pocket Guide to Physical -

International Journal of Medical and Health Sciences
International Journal of Medical and Health Sciences Journal Home Page: http://www.ijmhs.net ISSN:2277-4505 Review article Examining the liver – Revisiting an old friend Cyriac Abby Philips1*, Apurva Pande2 1Department of Hepatology and Transplant Medicine, PVS Institute of Digestive Diseases, PVS Memorial Hospital, Kaloor, Kochi, Kerala, India, 2Department of Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India. ABSTRACT In the current era of medical practice, super saturated with investigations of choice and development of diagnostic tools, clinical examination is a lost art. In this review we briefly discuss important aspects of examination of the liver, which is much needed in decision making on investigational approach. We urge the new medical student or the newly practicing physician to develop skills in clinical examination for resourceful management of the patient. KEYWORDS: Liver, examination, clinical skills, hepatomegaly, chronic liver disease, portal hypertension, liver span INTRODUCTION respiration, the excursion of liver movement is around 2 to 3 The liver attains its adult size by the age of 15 years. The cm. Castell and Frank has elegantly described normal liver liver weighs 1.2 to 1.4 kg in women and 1.4 to 1.5 kg in span in men and women utilizing the percussion method men. The liver seldom extends more than 5 cm beyond the (Table 1). Accordingly, the mean liver span is 10.5 cm for midline towards the left costal margin. During inspiration, men and 7 cm in women. During examination, a span 2 to 3 the diaphragmatic exertion moves the liver downward with cm larger or smaller than these values is considered anterior surface rotating to the right. -
General Physical Examination Skills for Ahps
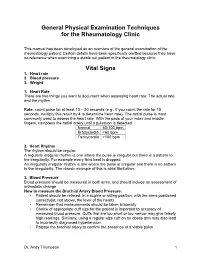
General Physical Examination Techniques for the Rheumatology Clinic This manual has been developed as an overview of the general examination of the rheumatology patient. Certain details have been specifically omitted because they have no relevance when examining a stable out patient in the rheumatology clinic. Vital Signs 1. Heart rate 2. Blood pressure 3. Weight 1. Heart Rate There are two things you want to document when assessing heart rate: The actual rate and the rhythm. Rate: count pulse for at least 15 – 30 seconds (e.g., if you count the rate for 15 seconds, multiply this result by 4 to determine heart rate). The radial pulse is most commonly used to assess the heart rate. With the pads of your index and middle fingers, compress the radial artery until a pulsation is detected. Normal 60-100 bpm Bradycardia <60 bpm Tachycardia >100 bpm 2. Heart Rhythm The rhythm should be regular. A regularly irregular rhythm is one where the pulse is irregular but there is a pattern to the irregularity. For example every third beat is dropped. An irregularly irregular rhythm is one where the pulse is irregular and there is no pattern to the irregularity. The classic example of this is atrial fibrillation. 3. Blood Pressure Blood pressure should be measured in both arms, and should include an assessment of orthostatic change How to measure the Brachial Artery Blood Pressure: • Patient should be relaxed, in a supine or sitting position, with the arms positioned correctly(at, not above, the level of the heart) • Remember that measurements should be taken bilaterally • Choice of appropriate cuff size for the patient is important to accuracy of measured blood pressure. -

HEENT EXAMINIATION ______HEENT Exam Exam Overview
HEENT EXAMINIATION ____________________________________________________________ HEENT Exam Exam Overview I. Head A. Visual inspection B. Palpation of scalp II. Eyes A. Visual Acuity B. Visual Fields C. Extraocular Movements/Near Response D. Inspection of sclera & conjunctiva E. Pupils F. Ophthalmoscopy III. Ears A. External Inspection B. Otoscopy C. Hearing Acuity D. Weber/Rinne IV. Nose A. External Inspection B. Speculum/otoscope C. Sinus areas V. Throat/Mouth A. Mouth Examination B. Pharynx Examination C. Bimanual Palpation VI. Neck A. Lymph nodes B. Thyroid gland 29 HEENT EXAMINIATION ____________________________________________________________ HEENT Terms Acuity – (ehk-yu-eh-tee) sharpness, clearness, and distinctness of perception or vision. Accommodation - adjustment, especially of the eye for seeing objects at various distances. Miosis – (mi-o-siss) constriction of the pupil of the eye, resulting from a normal response to an increase in light or caused by certain drugs or pathological conditions. Conjunctiva – (kon-junk-ti-veh) the mucous membrane lining the inner surfaces of the eyelids and anterior part of the sclera. Sclera – (sklehr-eh) the tough fibrous tunic forming the outer envelope of the eye and covering all of the eyeball except the cornea. Cornea – (kor-nee-eh) clear, bowl-shaped structure at the front of the eye. It is located in front of the colored part of the eye (iris). The cornea lets light into the eye and partially focuses it. Glaucoma – (glaw-ko-ma) any of a group of eye diseases characterized by abnormally high intraocular fluid pressure, damaged optic disk, hardening of the eyeball, and partial to complete loss of vision. Conductive hearing loss - a hearing impairment of the outer or middle ear, which is due to abnormalities or damage within the conductive pathways leading to the inner ear. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

EPA Quick Reference Guide
EPA Quick Reference Guide EPAs 1 & 2 – Professionalism Unacceptable • Unreliable • Dishonest • Avoids responsibility • Commitment uncertain • Dresses inappropriately • Unexplained absences • Verbal and non-verbal disrespect towards preceptor • Does not recognize own limitations and the need to seek assistance • Unable to comprehend the point of view and emotional state of other people • Judgmental of others • Fails to recognize and respect cross-cultural and gender differences Minimally Competent • Sometimes late • Not consistently able to complete assignments or tasks • Not consistently considerate of the feelings and emotional needs of others • Sometimes judgmental Competent • Punctual • Dependable • Accepts responsibilities • Demonstrates a willingness to accept feedback regarding necessary change(s) • Appropriately shows concern for others’ feelings and interacts accordingly • Recognizes and respects cross-cultural and gender differences Office of Medical Education 306 Liberty View Lane, Lynchburg, Va. 24502 [email protected] EPAs 3 & 4 – Data Gathering / Interviewing & Physical Examination Skills Unacceptable • Inefficient, disorganized • Weak prioritization skills • Misses major findings • Fails to appreciate physical findings and pertinent information • History and/or physical exam incomplete or inaccurate • Insufficient attention to psychosocial issues • Needs to work on establishing rapport with patients • Needs to work on awareness of appropriate boundaries with patients • Needs to improve demonstration of compassion • -
Clinical Reasoning - the Process of Thinking and Decision Making, Consciously & Unconsciously Guide Practice Actions
Diagnostic Reasoning “DR” Toolbox for Hospitalist Faculty Heather Hofmann, MD Department of Medicine 2017-18 2 Goal Increase faculty familiarity with diagnostic reasoning principles and tools so as to improve its teaching. Three Parts: I: Introduction to Diagnostic Reasoning II: DR Toolbox III: Structured Reflection Exercise (SRE) 4 Part I: Introduction to Diagnostic Reasoning Learning Objectives - Understand the “what” and “why” of Diagnostic Reasoning - Recognize dual-process theory’s role in “how” we reason 6 What is Diagnostic Reasoning? - Clinical reasoning - The process of thinking and decision making, consciously & unconsciously guide practice actions 25yo female G1P0, 2m gestation returns from Rio. - Diagnostic reasoning: - The process of collecting & analyzing information establish a diagnosis chest pain STEMI in proximal LAD abdominal pain acute appendicitis 7 Why teach diagnostic reasoning? - Incorrect diagnoses are often at the root of medical errors - DR is a means to apply basic science to clinical problems - Central to being a physician 8 Patient’s perspective What’s wrong with me? Is it bad? What can we do about it? 9 Why now? Never too early for practice 10 From Novice to Expert 11 How do we reason? Information processing theory 12 How do we reason? Information processing theory: Dual process theory. Analytical Non-analytical Conscious Unconscious Type/System 2 Type/System 1 Slow Fast Effortful Automatic Deliberative Involuntary Logical Emotional Requires attention, Executes skilled self-control, time. response and -

Advanced Interpretation of Adult Vital Signs in Trauma William D
Advanced Interpretation of Adult Vital Signs in Trauma William D. Hampton, DO Emergency Physician 26 March 2015 Learning Objectives 1. Better understand vital signs for what they can tell you (and what they can’t) in the assessment of a trauma patient. 2. Appreciate best practices in obtaining accurate vital signs in trauma patients. 3. Learn what teaching about vital signs is evidence-based and what is not. 4. Explain the importance of vital signs to more accurately triage, diagnose, and confidently disposition our trauma patients. 5. Apply the monitoring (and manipulation of) vital signs to better resuscitate trauma patients. Disclosure Statement • Faculty/Presenters/Authors/Content Reviewers/Planners disclose no conflict of interest relative to this educational activity. Successful Completion • To successfully complete this course, participants must attend the entire event and complete/submit the evaluation at the end of the session. • Society of Trauma Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Vital Signs Vital Signs Philosophy: “View vital signs as compensatory to the illness/complaint as opposed to primary.” Crowe, Donald MD. “Vital Sign Rant.” EMRAP: Emergency Medicine Reviews and Perspectives. February, 2010. Vital Signs Truth over Accuracy: • Document the true status of the patient: sick or not? • Complete vital signs on every patient, every time, regardless of the chief complaint. • If vital signs seem misleading or inaccurate, repeat them! • Beware sending a patient home with abnormal vitals (especially tachycardia)! •Treat vital signs the same as any other diagnostics— review them carefully prior to disposition. The Mother’s Vital Sign: Temperature Case #1 - 76-y/o homeless ♂ CC: 76-y/o homeless ♂ brought to the ED by police for eval. -

The Older Adult 20
CHAPTER The Older Adult 20 Older adults now number more than 25 million people in the United States and are expected to reach 80 million by 2050.1 These seniors will live longer than previous generations: life span at birth is currently 79 years for women and 74 years for men. Those older than 85 years are projected to increase to 5% of the U.S. population within 40 years. Hence, the “demographic im- perative” is to maximize not only the life span but also the “health span” of our older population, so that seniors maintain full function for as long as possible, enjoying rich and active lives in their homes and communities. Clinicians now recognize frailty as one of society’s common myths about aging—more than 95% of Americans older than 65 years live in the commu- nity, and only 5% reside in long-term care facilities.1,2 Over the past 20 years, seniors actually have become more active and less disabled. These changes call for new goals for clinical care—“an informed activated patient inter- acting with a prepared proactive team, resulting in high quality satisfying en- counters and improved outcomes”3—and a distinct set of clinical attitudes and skills. CHAPTER 20 I THE OLDER ADULT 839 ANATOMY AND PHYSIOLOGY Assessing the older adult presents special opportunities and special challenges. Many of these are quite different from the disease-oriented approach of his- tory taking and physical examination for younger patients: the focus on healthy or “successful” aging; the need to understand and mobilize family, social, and community supports; the importance of skills directed to func- tional assessment, “the sixth vital sign”; and the opportunities for promoting the older adult’s long-term health and safety. -

Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -

Blood Pressure Year 1 Year 2 Core Clinical/Year 3+
Blood Pressure Year 1 Year 2 Core Clinical/Year 3+ Do Do • Patient at rest for 5 minutes • Measure postural BP and pulse in patients with a • Arm at heart level history suggestive of volume depletion or • Correct size cuff- bladder encircles 80% of arm syncope • Center of cuff aligns with brachial artery -Measure BP and pulse in supine position • Cuff wrapped snugly on bare arm with lower -Slowly have patient rise and stand (lie them down edge 2-3 cm above antecubital fossa promptly if symptoms of lightheadedness occur) • Palpate radial artery, inflate cuff to 70 mmHg, -Measure BP and pulse after 1 minute of standing then increase in 10 mmHg increments to 30 mmHg above point where radial pulse disappears. Know Deflate slowly until pulse returns; this is the • Normally when a person stands fluid shifts to approximate systolic pressure. lower extremities causing a compensatory rise in • Auscultate the Korotkoff sounds pulse by up to 10 bpm with BP dropping slightly -place bell lightly in antecubital fossa • Positive postural vital signs are defined as -inflate BP to 20-30mmHg above SBP as determined symptoms of lightheadedness and/or a drop in by palpation SBP of 20 mmHg with standing -deflate cuff at rate 2mmHg/second while auscultating • Know variations in BP cuff sizes -first faint tapping (Phase I Korotkoff) = SBP; • A lack of rise in pulse in a patient with an Disappearance of sound (Phase V Korotkoff)=DBP orthostatic drop in pressure is a clue that the Know cause is neurologic or related or related to -Korotkoff sounds are lower pitch, better heard by bell medications (eg. -

Wilderness First Aid Reference Cards
Pulse/Pressure Points Wilderness First Aid Reference Cards Carotid Brachial Prepared by: Andrea Andraschko, W-EMT Radial October 2006 Femoral Posterior Dorsalis Tibial Pedis Abdominal Quadrants Airway Anatomy (Looking at Patient) RIGHT UPPER: LEFT UPPER: ANTERIOR: ANTERIOR: GALL BLADDER STOMACH LIVER SPLEEN POSTERIOR: POSTERIOR: R. KIDNEY PANCREAS L. KIDNEY RIGHT LOWER: ANTERIOR: APPENDIX CENTRAL AORTA BLADDER Tenderness in a quadrant suggests potential injury to the organ indicated in the chart. Patient Assessment System SOAP Note Information (Focused Exam) Scene Size-up BLS Pt. Information Physical (head to toe) exam: DCAP-BTLS, MOI Respiratory MOI OPQRST • Major trauma • Air in and out Environmental conditions • Environmental • Adequate Position pt. found Normal Vitals • Medical Nervous Initial Px: ABCs, AVPU Pulse: 60-90 Safety/Danger • AVPU Initial Tx Respiration: 12-20, easy Skin: Pink, warm, dry • Move/rescue patient • Protect spine/C-collar SAMPLE LOC: alert and oriented • Body substance isolation Circulatory Symptoms • Remove from heat/cold exposure • Pulse Allergies Possible Px: Trauma, Environmental, Medical • Consider safety of rescuers • Check for and Stop Severe Bleeding Current Px Medications Resources Anticipated Px → Past/pertinent Hx • # Patients STOP THINK: Field Tx ast oral intake • # Trained rescuers A – Continue with detailed exam L S/Sx to monitor VPU EVAC NOW Event leading to incident • Available equipment (incl. Pt’s) – Evac level Patient Level of Consciousness (LOC) Shock Assessment Reliable Pt: AVPU Hypovolemic – Low fluid (Tank) Calm A+ Awake and Cooperative Cardiogenic – heart problem (Pump) Comment: Cooperative A- Awake and lethargic or combative Vascular – vessel problem (Hose) If a pulse drops but does not return Sober V+ Responds with sound to verbal to ‘normal’ (60-90 bpm) within 5-25 Alert stimuli Volume Shock (VS) early/compensated minutes, an elevated pulse is likely caused by VS and not ASR.