Towards Understanding Mode-Of-Action of Traditional Medicines by Using in Silico Target Prediction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
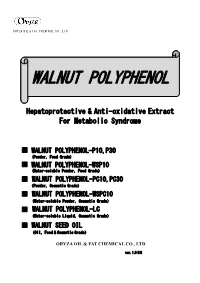
Walnut Polyphenol
ORYZA OIL & FAT CHEMICAL CO., L TD. WALNUT POLYPHENOL Hepatoprotective & Anti-oxidative Extract For Metabolic Syndrome ■ WALNUT POLYPHENOL-P10,P30 (Powder,Food Grade) ■ WALNUT POLYPHENOL-WSP10 (Water-soluble Powder,Food Grade) ■ WALNUT POLYPHENOL-PC10,PC30 (Powder,Cosmetic Grade) ■ WALNUT POLYPHENOL-WSPC10 (Water-soluble Powder,Cosmetic Grade) ■ WALNUT POLYPHENOL-LC (Water-soluble Liquid,Cosmetic Grade) ■ WALNUT SEED OIL (Oil,Food & Cosmetic Grade) ORYZA OIL & FAT CHEMICAL CO., LTD ver. 1.0 HS WALNUT POLYPHENOL ver.1.0 HS WALNUT POLYPHENOL Hepatoprotective & Anti-oxidative Extract For Metabolic Syndrome 1. Introduction Recently, there is an increased awareness on metabolic syndrome – a condition characterized by a group of metabolic risk factors in one person. They include abdominal obesity, atherogenic dyslipidemia, elevated blood pressure, insulin resistance, prothrombotic state & proinflammatory state. The dominant underlying risk factors appear to be abdominal obesity and insulin resistance. In addition, non-alcoholic fatty liver disease (NAFLD) is the most commonly associated “liver” manifestation of metabolic syndrome which can progress to advance liver disease (e.g. cirrhosis) with associated morbidity and mortality. Lifestyle therapies such as weight loss significantly improve all aspects of metabolic syndrome, as well as reducing progression of NAFLD and cardiovascular mortality. Walnut (Juglans regia L. seed) is one the most popular nuts consumed in the world. It is loaded in polyunsaturated fatty acids – linoleic acid (LA), oleic acid and α-linolenic acid (ALA), an ω3 fatty acid. It has been used since ancient times and epidemiological studies have revealed that incorporating walnuts in a healthy diet reduces the risk of cardiovascular diseases. Recent investigations reported that walnut diet improves the function of blood vessels and lower serum cholesterol. -

Tannins: Current Knowledge of Food Sources, Intake, Bioavailability and Biological Effects
S310 DOI 10.1002/mnfr.200900039 Mol. Nutr. Food Res. 2009, 53, S310 – S329 Review Tannins: Current knowledge of food sources, intake, bioavailability and biological effects Jos Serrano1, Riitta Puupponen-Pimi2, Andreas Dauer3, Anna-Marja Aura2 and Fulgencio Saura-Calixto4 1 Universidad Complutense de Madrid, Depto. Nutricin y Bromatologa I, Madrid, Spain 2 VTT Technical Research Center of Finland 3 Hexal AG, Holzkirchen, Germany 4 Consejo Superior de Investigaciones Cientficas, Instituto del Frio, Depto. Metabolismo y Nutricin, Madrid, Spain Tannins are a unique group of phenolic metabolites with molecular weights between 500 and 30000 Da, which are widely distributed in almost all plant foods and beverages. Proanthocyanidins and hydrolysable tannins are the two major groups of these bioactive compounds, but complex tannins containing structural elements of both groups and specific tannins in marine brown algae have also been described. Most literature data on food tannins refer only to oligomeric compounds that are extracted with aqueous-organic solvents, but a significant number of non-extractable tannins are usu- ally not mentioned in the literature. The biological effects of tannins usually depend on their grade of polymerisation and solubility. Highly polymerised tannins exhibit low bioaccessibility in the small intestine and low fermentability by colonic microflora. This review summarises a new approach to analysis of extractable and non-extractable tannins, major food sources, and effects of storage and processing on tannin content and bioavailability. Biological properties such as antioxidant, antimicro- bial and antiviral effects are also described. In addition, the role of tannins in diabetes mellitus has been discussed. Keywords: Bioavailability / Diet / Hydrolysable tannins / Proanthocyanidins / Tannins / Received: November 27, 2007; revised: January 25, 2009; accepted: February 9, 2009 1 Introduction weight having the ability to complex strongly with carbohy- drates and proteins [9]. -

In Vitro Fungistatic Activity of 36 Traditional Oriental Medicines and Their Synergistic Effect Against Trichophyton Rubrume Young Soo Kim, Jin Yeul Ma
Asian Pacific Journal of Tropical Medicine 2018; 11(2): 109-115 109 IF: 0.925 Asian Pacific Journal of Tropical Medicine journal homepage: www.apjtm.org doi: 10.4103/1995-7645.225017 ©2018 by the Asian Pacific Journal of Tropical Medicine. All rights reserved. In vitro fungistatic activity of 36 traditional oriental medicines and their synergistic effect against Trichophyton rubrume Young Soo Kim, Jin Yeul Ma Korean Medicine Application Center, Korea Institute of Oriental Medicine, 70 Cheomdan-ro, Dong-gu, Daegu, 41062, Republic of Korea ARTICLE INFO ABSTRACT Article history: Objective: To investigate the fungistatic activity and synergistic effects of natural products Received 12 October 2017 and their constituents, including traditional oriental medicines (TOMs). Methods: Fungistatic Received in revised form 17 November 2017 activities of TOMs prepared by hot-water (115 ) or ethanol (70%; 40 ) extraction were Accepted 4 December 2017 曟 曟 Available online 2 February 2018 determined by their minimum inhibitory concentration. To assess possible synergistic effects, minimum inhibitory concentrations of various combinations were evaluated. Results: By Keywords: evaluating antifungal susceptibility of Trichophyton rubrum, which is a major causative fungus Fungistatic activity for several types of dermatophytosis, we confirmed that ethanol extracts were more active Hot-water and ethanol extracts than hot-water extracts in 25 of the 36 TOMs, suggesting that the constituents with high Traditional oriental medicine hydrophobicity tend to contribute significantly to fungistatic activity. We selected four TOMs Tinea with high fungistatic activity, including Aucklandiae radix, Gentianae macrophyllae radix, Trichophyton rubrum Synergistic effect Scutellariae radix, and Galla rhois, and their synergistic effects were investigated through the combination studies between TOMs or TOM-conventional drug terbinafine. -

Raspberry Pomace - Composition, Properties and Application
View metadata, citation and similar papers at core.ac.uk brought to you by CORE European Journal ISSN 2449-8955 Review Article of Biological Research Raspberry pomace - composition, properties and application Agnieszka Joanna Brodowska Institute of General Food Chemistry, Faculty of Biotechnology and Food Sciences, Łódź University of Technology, Stefanowskiego 4/10, 90-924 Łódź, Poland * Corresponding author: Agnieszka Brodowska; E-mail: [email protected] Received: 19 February 2017; Revised submission: 24 March 2017; Accepted: 03 April 2017 Copyright: © The Author(s) 2017. European Journal of Biological Research © T.M.Karpi ński 2017. This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited. DOI : http://dx.doi.org/10.5281/zenodo.495190 ABSTRACT industry by-product, is considered as a potential food ingredient. Its pomace contains plenty of Raspberry pomace can be valorised due to its valuable components such as carbohydrates, nutritionally favourable effect on human health. proteins, fats, fibre, flavours, pectins, vitamins, It is an important source of polyphenols, ellagic similar to the composition of whole raspberries [2]. acid, ellagitannins, tocopherols, unsaturated fatty Moreover, raspberry pomace is rich in a large group acids, and dietary fibre. Thus, raspberry pomace of various phenolics especially ellagitannins, can be considered as a potential raw material to proanthocyanidins, anthocyanins, flavonols, and receive products rich in polyphenols or dietary phenolic acids (especially, ellagic acid) which are fibre, which can provide healthy properties to food also predominant in berries [3]. -

Roles of Fungal Endophytes and Viruses in Mediating Drought Stress Tolerance in Plants
INTERNATIONAL JOURNAL OF AGRICULTURE & BIOLOGY ISSN Print: 1560–8530; ISSN Online: 1814–9596 20–0504/2020/24–6–1497–1512 DOI: 10.17957/IJAB/15.1588 http://www.fspublishers.org Review Article Roles of Fungal Endophytes and Viruses in Mediating Drought Stress Tolerance in Plants Khondoker Mohammad Golam Dastogeer1,2*, Anindita Chakraborty3,4, Mohammad Saiful Alam Sarker5 and Mst Arjina Akter1 1Department of Plant Pathology, Bangladesh Agricultural University, Mymensingh, Bangladesh 2Institute of Agriculture, Tokyo University of Agriculture and Technology, Fuchu, Tokyo 183-8509, Japan 3Department of Genetic Engineering and Biotechnology, Shahjalal University of Science & Technology, Sylhet, Bangladesh 4WA State Agricultural Biotechnology Centre (SABC) Murdoch University, Perth, Western Australia 5Basic & Applied Research on Jute Project, Bangladesh Jute Research Institute (BJRI), Bangladesh *For correspondence: [email protected] Received 28 March 2020; Accepted 03 July 2020; Published 10 October 2020 Abstract Various biotic and abiotic stresses can hamper crop productivity and thus pose threats to global food security. Sustainable agricultural production demands for the use of safer and eco-friendly tools and inputs in farm production. In addition to plant growth-promoting bacteria and mycorrhizal fungi, endophytic fungi can also help plant mitigate or reduce the effect of stresses. Another less well-known is the use of viruses that provide benefit to plants facing growth challenges due to stress. Studies suggest that fungal endophyte and virus could be important candidate and economically and ecologically sustainable means for protecting plants from stress condition. To exploit their benefits, a thorough understanding of the interaction of host- beneficial microbes obtained by scientifically sound experiments with robust statistical analysis is crucial. -

Molecular Systematics of Genus Atractylodes (Compositae, Cardueae): Evidence from Internal Transcribed Spacer (ITS) and Trnl-F Sequences
Int. J. Mol. Sci. 2012, 13, 14623-14633; doi:10.3390/ijms131114623 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Article Molecular Systematics of Genus Atractylodes (Compositae, Cardueae): Evidence from Internal Transcribed Spacer (ITS) and trnL-F Sequences Hua-Sheng Peng 1,2, Qing-Jun Yuan 1, Qian-Quan Li 1 and Lu-Qi Huang 1,* 1 Institute of Chinese Materia Medica, China Academy of Chinese Medical Science, Beijing 100700, China; E-Mails: [email protected] (H.-S.P.); [email protected] (Q.-J.Y.); [email protected] (Q.-Q.L.) 2 Department of Pharmacy, Anhui University of Traditional Chinese Medicine, Hefei 230031, China * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +86-10-8404-4340. Received: 13 August 2012; in revised form: 26 October 2012 / Accepted: 30 October 2012 / Published: 9 November 2012 Abstract: To determine the evolutionary relationships among all members of the genus Atractylodes (Compositae, Cardueae), we conducted molecular phylogenetic analyses of one nuclear DNA (nrDNA) region (internal transcribed spacer, ITS) and one chloroplast DNA (cpDNA) region (intergenic spacer region of trnL-F). In ITS and ITS + trnL-F trees, all members of Atractylodes form a monophyletic clade. Atractylodes is a sister group of the Carlina and Atractylis branch. Atractylodes species were distributed among three clades: (1) A. carlinoides (located in the lowest base of the Atractylodes phylogenetic tree), (2) A. macrocephala, and (3) the A. lancea complex, including A. japonica, A. coreana, A. lancea, A. lancea subsp. luotianensis, and A. chinensis. The taxonomic controversy over the classification of species of Atractylodes is mainly concentrated in the A. -

Ellagitannin–Lipid Interaction by HR-MAS NMR Spectroscopy
molecules Article Ellagitannin–Lipid Interaction by HR-MAS NMR Spectroscopy Valtteri Virtanen * , Susanna Räikkönen, Elina Puljula and Maarit Karonen Natural Chemistry Research Group, Department of Chemistry, University of Turku, FI-20014 Turku, Finland; [email protected] (S.R.); [email protected] (E.P.); maarit.karonen@utu.fi (M.K.) * Correspondence: vtjvir@utu.fi; Tel.: +358-29-450-3205 Abstract: Ellagitannins have antimicrobial activity, which might be related to their interactions with membrane lipids. We studied the interactions of 12 different ellagitannins and pentagalloylglucose with a lipid extract of Escherichia coli by high-resolution magic angle spinning NMR spectroscopy. The nuclear Overhauser effect was utilized to measure the cross relaxation rates between ellagitannin and lipid protons. The shifting of lipid signals in 1H NMR spectra of ellagitannin–lipid mixture due to ring current effect was also observed. The ellagitannins that showed interaction with lipids had clear structural similarities. All ellagitannins that had interactions with lipids had glucopy- ranose cores. In addition to the central polyol, the most important structural feature affecting the interaction seemed to be the structural flexibility of the ellagitannin. Even dimeric and trimeric ellagitannins could penetrate to the lipid bilayers if their structures were flexible with free galloyl and hexahydroxydiphenoyl groups. Keywords: E. coli; HR-MAS-NMR; interaction; lipid membrane; tannins; UPLC-DAD-MS Citation: Virtanen, V.; Räikkönen, S.; Puljula, E.; Karonen, M. 1. Introduction Ellagitannin–Lipid Interaction by HR-MAS NMR Spectroscopy. Tannins are a group of specialized plant metabolites, which, when included in the di- Molecules 2021, 26, 373. etary feed of ruminants, have been shown to induce many beneficial effects such as increas- https://doi.org/10.3390/ ing their effective amino acid absorption, lowering their methane production, and acting as molecules26020373 anthelmintics [1–6]. -

Characteristic Odor Components of Essential Oil from Scutellaria Laeteviolacea
Journal of Oleo Science Copyright ©2013 by Japan Oil Chemists’ Society J. Oleo Sci. 62, (1) 51-56 (2013) Characteristic Odor Components of Essential Oil from Scutellaria laeteviolacea Mitsuo Miyazawa1* , Machi Nomura1, 2, Shinsuke Marumoto1 and Kiyoshige Mori2 1 Department of Applied Chemistry, Faculty of Science and Engineering, Kinki University 3-4-1 Kowakae, Higashiosakashi, Osaka 577-8502, Japan 2 Ohsugi Pharmaceutical Co., Ltd, 1-1-2 Abeno-ku Tennoji-cho minami, Osaka 545-0002, Japan Abstract: The essential oils from aerial parts of Scutellaria laeteviolacea was analyzed by gas chromatography (GC) and gas chromatography-mass spectrometry (GC-MS). The characteristic odor components were also detected in the oil using gas chromatography-olfactometry (GC-O) analysis and aroma extraction dilution analysis (AEDA). As a result, 100 components (accounting for 99.11 %) of S. laeteviolacea, were identified. The major components of S. laeteviolacea oil were found to be 1-octen-3-ol (27.72 %), germacrene D (21.67 %),and β-caryophyllene (9.18 %). The GC-O and AEDA results showed that 1-octen-3-ol, germacrene D, germacrene B, and β-caryophyllene were the most characteristic odor components of the oil. These compounds are thought to contribute to the unique flavor of this plant. Key words: essential oil, Scutellaria laeteviolacea, 1-octen-3-ol, aroma extraction dilution analysis, relative flavor activity 1 INTRODUCTION particular, gas chromatography-olfactometry(GC-O)analy- Scutellaria laeteviolacea is a perennial plant belonging sis, including aroma extract dilution analysi(s AEDA)and to the family Lamiaceae. In recent years, this aromatic CharmAnalysis, has been used to identify the potent odor- plant of the aerial parts has been used as a herb in Japan. -

Metabolic Changes of Aflatoxin B1 to Become an Active Carcinogen And
ome Re un se m a rc Im h Immunome Research Carvajal-Moreno M, Immunome Res 2015, 11:2 ISSN: 1745-7580 DOI: 10.4172/1745-7580.10000104 Review Article Open Access Metabolic Changes of Aflatoxin B1 to become an Active Carcinogen and the Control of this Toxin Magda Carvajal-Moreno Departamento de Botánica, Instituto de Biología, Universidad Nacional Autónoma de México. Ciudad Universitaria, Coyoacán, 04510 México DF Corresponding author: Magda Carvajal-Moreno, Departamento de Botánica, Instituto de Biología, Universidad Nacional Autónoma de México. Ciudad Universitaria, Coyoacán, 04510 México DF, Tel: +52 55 5622 1332; E-mail: [email protected] Received date: November 07, 2015; Accepted date: December 18, 2015; Published date: December 22, 2015 Copyright: © 2015 Carvajal-Moreno M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Although aflatoxins are unavoidable toxins of food, many methods are available to control them, ranging from natural detoxifying methods to more sophisticated ones. The present review englobes the main characteristics of Aflatoxins as mutagens and carcinogens for humans, their physicochemical properties, the producing fungi, susceptible crops, effects and metabolism. In the metabolism of Aflatoxins the role of cytochromes and isoenzymes, epigenetics, glutathione-S-transferase enzymes, oncogenes and the role of aflatoxins -

Use of the Psba-Trnh Region to Authenticate Medicinal Species of Fabaceae
December 2013 Regular Article Biol. Pharm. Bull. 36(12) 1975–1979 (2013) 1975 Use of the psbA-trnH Region to Authenticate Medicinal Species of Fabaceae Ting Gao,a Xinye Ma,b and Xunzhi Zhu*,c a Key Laboratory of Plant Biotechnology in Universities of Shandong Province, College of Life Sciences, Qingdao Agricultural University; Qingdao, Shandong 266109, P.R. China: b Research Center of Chinese Herbal Resource Science and Engineering, Key Laboratory of Chinese Medicinal Resource from Lingnan, Ministry of Education, Guangzhou University of Chinese Medicine; Guangzhou, Guangdong 510006, P.R. China: and c School of Biology and Chemical Engineering, Jiangsu University of Science and Technology; Zhenjiang, Jiangsu 212018, P.R. China. Received August 3, 2013; accepted October 3, 2013; advance publication released online October 8, 2013 Fabaceae is a huge family that contains a large number of medicinal plants, many of which are com- monly used in Chinese traditional medicine. However, traditional taxonomy has not been able to meet the complicated demands of species discrimination within Fabaceae. Thus, we employed a famous DNA barcode, the psbA-trnH region, to discriminate commonly used medicinal species of the family Fabaceae. Here, the psbA-trnH regions derived from 152 samples were amplified. These samples represented 104 Fabaceae me- dicinal species from 60 genera, including 25 authentic Fabaceae species listed in the Chinese pharmacopoeia and common adulterant species. The results indicate that the psbA-trnH region performed well in terms of its universality and high variability in length and composition. Species discriminative power analysis of the psbA-trnH region showed that 91.3% of species could be identified successfully by the BLAST1 method in conjunction with the nearest distance method. -

In Vitro Propagation and Cytological Analysis of Sophora Mollis Royle: an Endangered Medicinal Shrub
Bhandari et al. Journal of Genetic Engineering and Biotechnology (2021) 19:40 Journal of Genetic Engineering https://doi.org/10.1186/s43141-021-00140-3 and Biotechnology RESEARCH Open Access In vitro propagation and cytological analysis of Sophora mollis Royle: an endangered medicinal shrub Aakriti Bhandari1, Harminder Singh1,2, Amber Srivastava1, Puneet Kumar1, G. S. Panwar1* and A. A. Mao3 Abstract Background: Sophora mollis Royle (family Fabaceae, subfamily-Papilionaceae) is a multipurpose legume distributed in plains and foothills of the North-West Himalaya to Nepal and is facing high risk of extinction due to habitat loss and exploitation by the local people for its fuel and fodder values. Therefore, the present study was conducted to standardize a micropropagation protocol for Sophora mollis by using shoot tip explants and to study the meiotic chromosome count in the species. Results: Multiple shoots were induced in shoot tip explants of Sophora mollis in Murashige and Skoog medium supplemented with different concentrations of cytokinins alone (BAP, TDZ, and Kinetin) and in combination with varying concentrations of NAA. MS medium supplemented with BAP (8.9 μM) was observed to be the optimal medium for multiple shoot induction and maximum 25.32 shoots per explant was obtained with average length of 4.5 ± 0.8 cm. In vitro developed shoots were transferred onto rooting media supplemented with different concentrations of auxin (IAA, IBA, and NAA). Maximum 86% rooting was observed in half-strength MS medium supplemented with 21.20 μM NAA with an average of 21.26 roots per culture. In vitro raised plantlets were adapted to greenhouse for better acclimatization and 60% plants were successfully transferred to the open environment. -

1 Universidade Federal Do Rio De Janeiro Instituto De
UNIVERSIDADE FEDERAL DO RIO DE JANEIRO INSTITUTO DE QUÍMICA PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIA DE ALIMENTOS Ana Beatriz Neves Martins DEVELOPMENT AND STABILITY OF JABUTICABA (MYRCIARIA JABOTICABA) JUICE OBTAINED BY STEAM EXTRACTION RIO DE JANEIRO 2018 1 Ana Beatriz Neves Martins DEVELOPMENT AND STABILITY OF JABUTICABA (MYRCIARIA JABOTICABA) JUICE OBTAINED BY STEAM EXTRACTION Dissertação de Mestrado apresentada ao Programa de Pós-graduação em Ciência de Alimentos do Instituto de Química, da Universidade Federal do Rio de Janeiro como parte dos requisitos necessários à obtenção do título de Mestre em Ciência de Alimentos. Orientadores: Prof.ª Mariana Costa Monteiro Prof. Daniel Perrone Moreira RIO DE JANEIRO 2018 2 3 Ana Beatriz Neves Martins DEVELOPMENT AND STABILITY OF JABUTICABA (MYRCIARIA JABOTICABA) JUICE OBTAINED BY STEAM EXTRACTION Dissertação de Mestrado apresentada ao Programa de Pós-graduação em Ciência de Alimentos do Instituto de Química, da Universidade Federal do Rio de Janeiro como parte dos requisitos necessários à obtenção do título de Mestre em Ciência de Alimentos. Aprovada por: ______________________________________________________ Presidente, Profª. Mariana Costa Monteiro, INJC/UFRJ ______________________________________________________ Profª. Maria Lúcia Mendes Lopes, INJC/UFRJ ______________________________________________________ Profª. Lourdes Maria Correa Cabral, EMPBRAPA RIO DE JANEIRO 2018 4 ACKNOLEDGEMENTS Ninguém passa por essa vida sem alguém pra dividir momentos, sorrisos ou choros. Então, se eu cheguei até aqui, foi porque jamais estive sozinha, e não poderia deixar de agradecer aqueles que estiveram comigo, fisicamente ou em pensamento. Primeiramente gostaria de agradecer aos meus pais, Claudia e Ricardo, por tudo. Pelo amor, pela amizade, pela incansável dedicação, pelos valores passados e por todo esforço pra que eu pudesse ter uma boa educação.