The Biomarkers of Key Mirnas and Target Genes Associated with Acute Myocardial Infarction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Individual Protomers of a G Protein-Coupled Receptor Dimer Integrate Distinct Functional Modules
OPEN Citation: Cell Discovery (2015) 1, 15011; doi:10.1038/celldisc.2015.11 © 2015 SIBS, CAS All rights reserved 2056-5968/15 ARTICLE www.nature.com/celldisc Individual protomers of a G protein-coupled receptor dimer integrate distinct functional modules Nathan D Camp1, Kyung-Soon Lee2, Jennifer L Wacker-Mhyre2, Timothy S Kountz2, Ji-Min Park2, Dorathy-Ann Harris2, Marianne Estrada2, Aaron Stewart2, Alejandro Wolf-Yadlin1, Chris Hague2 1Department of Genome Sciences, University of Washington School of Medicine, Seattle, WA, USA; 2Department of Pharmacology, University of Washington School of Medicine, Seattle, WA, USA Recent advances in proteomic technology reveal G-protein-coupled receptors (GPCRs) are organized as large, macromolecular protein complexes in cell membranes, adding a new layer of intricacy to GPCR signaling. We previously reported the α1D-adrenergic receptor (ADRA1D)—a key regulator of cardiovascular, urinary and CNS function—binds the syntrophin family of PDZ domain proteins (SNTA, SNTB1, and SNTB2) through a C-terminal PDZ ligand inter- action, ensuring receptor plasma membrane localization and G-protein coupling. To assess the uniqueness of this novel GPCR complex, 23 human GPCRs containing Type I PDZ ligands were subjected to TAP/MS proteomic analysis. Syntrophins did not interact with any other GPCRs. Unexpectedly, a second PDZ domain protein, scribble (SCRIB), was detected in ADRA1D complexes. Biochemical, proteomic, and dynamic mass redistribution analyses indicate syntrophins and SCRIB compete for the PDZ ligand, simultaneously exist within an ADRA1D multimer, and impart divergent pharmacological properties to the complex. Our results reveal an unprecedented modular dimeric architecture for the ADRA1D in the cell membrane, providing unexpected opportunities for fine-tuning receptor function through novel protein interactions in vivo, and for intervening in signal transduction with small molecules that can stabilize or disrupt unique GPCR:PDZ protein interfaces. -

Literature Mining Sustains and Enhances Knowledge Discovery from Omic Studies
LITERATURE MINING SUSTAINS AND ENHANCES KNOWLEDGE DISCOVERY FROM OMIC STUDIES by Rick Matthew Jordan B.S. Biology, University of Pittsburgh, 1996 M.S. Molecular Biology/Biotechnology, East Carolina University, 2001 M.S. Biomedical Informatics, University of Pittsburgh, 2005 Submitted to the Graduate Faculty of School of Medicine in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2016 UNIVERSITY OF PITTSBURGH SCHOOL OF MEDICINE This dissertation was presented by Rick Matthew Jordan It was defended on December 2, 2015 and approved by Shyam Visweswaran, M.D., Ph.D., Associate Professor Rebecca Jacobson, M.D., M.S., Professor Songjian Lu, Ph.D., Assistant Professor Dissertation Advisor: Vanathi Gopalakrishnan, Ph.D., Associate Professor ii Copyright © by Rick Matthew Jordan 2016 iii LITERATURE MINING SUSTAINS AND ENHANCES KNOWLEDGE DISCOVERY FROM OMIC STUDIES Rick Matthew Jordan, M.S. University of Pittsburgh, 2016 Genomic, proteomic and other experimentally generated data from studies of biological systems aiming to discover disease biomarkers are currently analyzed without sufficient supporting evidence from the literature due to complexities associated with automated processing. Extracting prior knowledge about markers associated with biological sample types and disease states from the literature is tedious, and little research has been performed to understand how to use this knowledge to inform the generation of classification models from ‘omic’ data. Using pathway analysis methods to better understand the underlying biology of complex diseases such as breast and lung cancers is state-of-the-art. However, the problem of how to combine literature- mining evidence with pathway analysis evidence is an open problem in biomedical informatics research. -
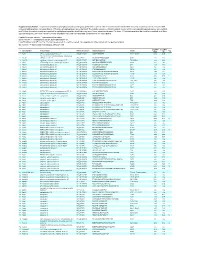
Supplementary Table 1
Supplementary Table 1. Large-scale quantitative phosphoproteomic profiling was performed on paired vehicle- and hormone-treated mTAL-enriched suspensions (n=3). A total of 654 unique phosphopeptides corresponding to 374 unique phosphoproteins were identified. The peptide sequence, phosphorylation site(s), and the corresponding protein name, gene symbol, and RefSeq Accession number are reported for each phosphopeptide identified in any one of three experimental pairs. For those 414 phosphopeptides that could be quantified in all three experimental pairs, the mean Hormone:Vehicle abundance ratio and corresponding standard error are also reported. Peptide Sequence column: * = phosphorylated residue Site(s) column: ^ = ambiguously assigned phosphorylation site Log2(H/V) Mean and SE columns: H = hormone-treated, V = vehicle-treated, n/a = peptide not observable in all 3 experimental pairs Sig. column: * = significantly changed Log 2(H/V), p<0.05 Log (H/V) Log (H/V) # Gene Symbol Protein Name Refseq Accession Peptide Sequence Site(s) 2 2 Sig. Mean SE 1 Aak1 AP2-associated protein kinase 1 NP_001166921 VGSLT*PPSS*PK T622^, S626^ 0.24 0.95 PREDICTED: ATP-binding cassette, sub-family A 2 Abca12 (ABC1), member 12 XP_237242 GLVQVLS*FFSQVQQQR S251^ 1.24 2.13 3 Abcc10 multidrug resistance-associated protein 7 NP_001101671 LMT*ELLS*GIRVLK T464, S468 -2.68 2.48 4 Abcf1 ATP-binding cassette sub-family F member 1 NP_001103353 QLSVPAS*DEEDEVPVPVPR S109 n/a n/a 5 Ablim1 actin-binding LIM protein 1 NP_001037859 PGSSIPGS*PGHTIYAK S51 -3.55 1.81 6 Ablim1 actin-binding -

Analysis of the Dystrophin Interactome
Analysis of the dystrophin interactome Dissertation In fulfillment of the requirements for the degree “Doctor rerum naturalium (Dr. rer. nat.)” integrated in the International Graduate School for Myology MyoGrad in the Department for Biology, Chemistry and Pharmacy at the Freie Universität Berlin in Cotutelle Agreement with the Ecole Doctorale 515 “Complexité du Vivant” at the Université Pierre et Marie Curie Paris Submitted by Matthew Thorley born in Scunthorpe, United Kingdom Berlin, 2016 Supervisor: Simone Spuler Second examiner: Sigmar Stricker Date of defense: 7th December 2016 Dedicated to My mother, Joy Thorley My father, David Thorley My sister, Alexandra Thorley My fiancée, Vera Sakhno-Cortesi Acknowledgements First and foremost, I would like to thank my supervisors William Duddy and Stephanie Duguez who gave me this research opportunity. Through their combined knowledge of computational and practical expertise within the field and constant availability for any and all assistance I required, have made the research possible. Their overarching support, approachability and upbeat nature throughout, while granting me freedom have made this year project very enjoyable. The additional guidance and supported offered by Matthias Selbach and his team whenever required along with a constant welcoming invitation within their lab has been greatly appreciated. I thank MyoGrad for the collaboration established between UPMC and Freie University, creating the collaboration within this research project possible, and offering research experience in both the Institute of Myology in Paris and the Max Delbruck Centre in Berlin. Vital to this process have been Gisele Bonne, Heike Pascal, Lidia Dolle and Susanne Wissler who have aided in the often complex processes that I am still not sure I fully understand. -

Supplementary Material
Supplementary material: Figure S1. Protein-Protein Interactions of the 127 Dysregulated proteins in brain tissues following IONP exposure. The graph was generated from STRING database. 125 nodes, 183 edges, 2.93 Average node degree, 0.411 Avg. local clustering coefficient, 122 Expected number of edges, PPI enrichment p-value 1.83e-07. 1 Figure S2. Protein-Protein Interactions of the 66 Dysregulated proteins in liver tissues following IONP exposure. The graph was generated from STRING database. 61 nodes, 103 edges, 3.38 Average node degree, 0.412 Avg. local clustering coefficient, 22 Expected number of edges, PPI enrichment p-value < 1.0e-16. 2 Figure S3. Protein-Protein Interactions of the 84 Dysregulated proteins in lung tissues following IONP exposure. The graph was generated from STRING database. 82 nodes, 125 edges, 3.05 Average node degree, 0.422 Avg. local clustering coefficient, 64 Expected number of edges, PPI enrichment p-value 1.07e-11. 3 Table S1. List of all dysregulated proteins in brain tissues following IONP exposure. A) Down regulated proteins and B) Upregulated proteins. Statistically significant iTRAQ ratios (p-value ratio and p-value sample≤0.05) for the 127 proteins that are dysregulated. A) Sequence Peptide Spectral P-Value P-Value Log 10 Accession Name Description Gene Coverage Ratio Count Count Ratio Sample Ratio % P00762 TRY1_RAT Anionic trypsin-1 Prss1 1 8 8.13 0.526 0.001 0.004 -0.279 P08592 A4_RAT Amyloid beta A4 protein App 1 2 1.17 0.546 0.010 0.004 -0.263 Q62696 DLG1_RAT Disks large homolog 1 Dlg1 1 1 1.32 -

Table SII. Significantly Differentially Expressed Mrnas of GSE23558 Data Series with the Criteria of Adjusted P<0.05 And
Table SII. Significantly differentially expressed mRNAs of GSE23558 data series with the criteria of adjusted P<0.05 and logFC>1.5. Probe ID Adjusted P-value logFC Gene symbol Gene title A_23_P157793 1.52x10-5 6.91 CA9 carbonic anhydrase 9 A_23_P161698 1.14x10-4 5.86 MMP3 matrix metallopeptidase 3 A_23_P25150 1.49x10-9 5.67 HOXC9 homeobox C9 A_23_P13094 3.26x10-4 5.56 MMP10 matrix metallopeptidase 10 A_23_P48570 2.36x10-5 5.48 DHRS2 dehydrogenase A_23_P125278 3.03x10-3 5.40 CXCL11 C-X-C motif chemokine ligand 11 A_23_P321501 1.63x10-5 5.38 DHRS2 dehydrogenase A_23_P431388 2.27x10-6 5.33 SPOCD1 SPOC domain containing 1 A_24_P20607 5.13x10-4 5.32 CXCL11 C-X-C motif chemokine ligand 11 A_24_P11061 3.70x10-3 5.30 CSAG1 chondrosarcoma associated gene 1 A_23_P87700 1.03x10-4 5.25 MFAP5 microfibrillar associated protein 5 A_23_P150979 1.81x10-2 5.25 MUCL1 mucin like 1 A_23_P1691 2.71x10-8 5.12 MMP1 matrix metallopeptidase 1 A_23_P350005 2.53x10-4 5.12 TRIML2 tripartite motif family like 2 A_24_P303091 1.23x10-3 4.99 CXCL10 C-X-C motif chemokine ligand 10 A_24_P923612 1.60x10-5 4.95 PTHLH parathyroid hormone like hormone A_23_P7313 6.03x10-5 4.94 SPP1 secreted phosphoprotein 1 A_23_P122924 2.45x10-8 4.93 INHBA inhibin A subunit A_32_P155460 6.56x10-3 4.91 PICSAR P38 inhibited cutaneous squamous cell carcinoma associated lincRNA A_24_P686965 8.75x10-7 4.82 SH2D5 SH2 domain containing 5 A_23_P105475 7.74x10-3 4.70 SLCO1B3 solute carrier organic anion transporter family member 1B3 A_24_P85099 4.82x10-5 4.67 HMGA2 high mobility group AT-hook 2 A_24_P101651 -

Peptidome Analysis of Umbilical Cord Mesenchymal Stem Cell (Huc-MSC
Wang et al. Stem Cell Research & Therapy (2020) 11:414 https://doi.org/10.1186/s13287-020-01931-0 RESEARCH Open Access Peptidome analysis of umbilical cord mesenchymal stem cell (hUC-MSC) conditioned medium from preterm and term infants Yu Wang1,2†, Lin Zhang1†, Yun Wu3, Rongping Zhu1, Yan Wang2, Yan Cao2, Wei Long4, Chenbo Ji2, Huaiyan Wang1* and Lianghui You 2* Abstract Background: The therapeutic role of mesenchymal stem cells (MSCs) has been widely confirmed in several animal models of premature infant diseases. Micromolecule peptides have shown promise for the treatment of premature infant diseases. However, the potential role of peptides secreted from MSCs has not been studied. The purpose of this study is to help to broaden the knowledge of the hUC-MSC secretome at the peptide level through peptidomic profile analysis. Methods: We used tandem mass tag (TMT) labeling technology followed by tandem mass spectrometry to compare the peptidomic profile of preterm and term umbilical cord MSC (hUC-MSC) conditioned medium (CM). Gene Ontology (GO) enrichment analysis and ingenuity pathway analysis (IPA) were conducted to explore the differentially expressed peptides by predicting the functions of their precursor proteins. To evaluate the effect of candidate peptides on human lung epithelial cells stimulated by hydrogen peroxide (H2O2), quantitative real-time PCR (qRT-PCR), western blot analysis, and enzyme-linked immunosorbent assay (ELISA) were, respectively, adopted to detect inflammatory cytokines (TNF-α, IL-1β, and IL-6) expression levels at the mRNA and protein levels. Results: A total of 131 peptides derived from 106 precursor proteins were differentially expressed in the preterm hUC-MSC CM compared with the term group, comprising 37 upregulated peptides and 94 downregulated peptides. -

Role of PDZ-Binding Motif from West Nile Virus NS5 Protein on Viral
www.nature.com/scientificreports OPEN Role of PDZ‑binding motif from West Nile virus NS5 protein on viral replication Emilie Giraud1*, Chloé Otero del Val2, Célia Caillet‑Saguy2, Nada Zehrouni2, Cécile Khou5, Joël Caillet4, Yves Jacob3, Nathalie Pardigon5 & Nicolas Wolf2 West Nile virus (WNV) is a Flavivirus, which can cause febrile illness in humans that may progress to encephalitis. Like any other obligate intracellular pathogens, Flaviviruses hijack cellular protein functions as a strategy for sustaining their life cycle. Many cellular proteins display globular domain known as PDZ domain that interacts with PDZ‑Binding Motifs (PBM) identifed in many viral proteins. Thus, cellular PDZ‑containing proteins are common targets during viral infection. The non‑structural protein 5 (NS5) from WNV provides both RNA cap methyltransferase and RNA polymerase activities and is involved in viral replication but its interactions with host proteins remain poorly known. In this study, we demonstrate that the C‑terminal PBM of WNV NS5 recognizes several human PDZ‑ containing proteins using both in vitro and in cellulo high‑throughput methods. Furthermore, we constructed and assayed in cell culture WNV replicons where the PBM within NS5 was mutated. Our results demonstrate that the PBM of WNV NS5 is important in WNV replication. Moreover, we show that knockdown of the PDZ‑containing proteins TJP1, PARD3, ARHGAP21 or SHANK2 results in the decrease of WNV replication in cells. Altogether, our data reveal that interactions between the PBM of NS5 and PDZ‑containing proteins afect West Nile virus replication. Arboviruses include numerous human and animal pathogens that are important global health threats responsible for arboviroses. -

Keep Your Fingers Off My DNA: Protein-Protein Interactions
1 2 Keep your fingers off my DNA: 3 protein-protein interactions mediated by C2H2 zinc finger domains 4 5 6 a scholarly review 7 8 9 10 11 Kathryn J. Brayer1 and David J. Segal2* 12 13 14 15 16 17 1Department of Pharmacology and Toxicology, College of Pharmacy, University of Arizona, 18 Tucson, AZ, 85721. 19 2Genome Center and Department of Pharmacology, University of California, Davis, CA, 95616. 20 21 22 23 24 *To whom correspondence should be addressed: 25 David J. Segal, Ph.D. 26 University of California, Davis 27 Genome Center/Pharmacology 28 4513 GBSF 29 451 E. Health Sciences Dr. 30 Davis, CA 95616 31 Tel: 530-754-9134 32 Fax: 530-754-9658 33 Email: [email protected] 34 35 36 Running header: C2H2 ZF interactions with proteins 37 38 Keywords: transcription factors, protein-DNA interactions, protein chemistry, structural biology, 39 functional annotations 40 41 Abstract: 154 words 42 Body Text: 5863 words 43 Figures: 9 44 Tables: 5 45 References: 165 46 C2H2 ZF interactions with proteins Brayer and Segal - review 46 ABSTRACT 47 Cys2-His2 (C2H2) zinc finger domains were originally identified as DNA binding 48 domains, and uncharacterized domains are typically assumed to function in DNA binding. 49 However, a growing body of evidence suggests an important and widespread role for these 50 domains in protein binding. There are even examples of zinc fingers that support both DNA and 51 protein interactions, which can be found in well-known DNA-binding proteins such as Sp1, 52 Zif268, and YY1. C2H2 protein-protein interactions are proving to be more abundant than 53 previously appreciated, more plastic than their DNA-binding counterparts, and more variable and 54 complex in their interactions surfaces. -

Genome-Wide Insights on Gastrointestinal Nematode
www.nature.com/scientificreports OPEN Genome‑wide insights on gastrointestinal nematode resistance in autochthonous Tunisian sheep A. M. Ahbara1,2, M. Rouatbi3,4, M. Gharbi3,4, M. Rekik1, A. Haile1, B. Rischkowsky1 & J. M. Mwacharo1,5* Gastrointestinal nematode (GIN) infections have negative impacts on animal health, welfare and production. Information from molecular studies can highlight the underlying genetic mechanisms that enhance host resistance to GIN. However, such information often lacks for traditionally managed indigenous livestock. Here, we analysed 600 K single nucleotide polymorphism genotypes of GIN infected and non‑infected traditionally managed autochthonous Tunisian sheep grazing communal natural pastures. Population structure analysis did not fnd genetic diferentiation that is consistent with infection status. However, by contrasting the infected versus non‑infected cohorts using ROH, LR‑GWAS, FST and XP‑EHH, we identifed 35 candidate regions that overlapped between at least two methods. Nineteen regions harboured QTLs for parasite resistance, immune capacity and disease susceptibility and, ten regions harboured QTLs for production (growth) and meat and carcass (fatness and anatomy) traits. The analysis also revealed candidate regions spanning genes enhancing innate immune defence (SLC22A4, SLC22A5, IL‑4, IL‑13), intestinal wound healing/repair (IL‑4, VIL1, CXCR1, CXCR2) and GIN expulsion (IL‑4, IL‑13). Our results suggest that traditionally managed indigenous sheep have evolved multiple strategies that evoke and enhance GIN resistance and developmental stability. They confrm the importance of obtaining information from indigenous sheep to investigate genomic regions of functional signifcance in understanding the architecture of GIN resistance. Small ruminants (sheep and goats) make immense socio-economic and cultural contributions across the globe. -

Entrez ID 1 Symbol 1 Entrez ID 2 Symbol 2 Data Source (R
Supporting Information Table 4. List of human protein-protein interactons. Entrez ID 1 Symbol 1 Entrez ID 2 Symbol 2 Data Source (R: Rual et al; S: Stelzl et al; L: Literature curation) 1 A1BG 10321 CRISP3 L 2 A2M 259 AMBP L 2 A2M 348 APOE L 2 A2M 351 APP L 2 A2M 354 KLK3 L 2 A2M 567 B2M L 2 A2M 1508 CTSB L 2 A2M 1990 ELA1 L 2 A2M 3309 HSPA5 L 2 A2M 3553 IL1B L 2 A2M 3586 IL10 L 2 A2M 3931 LCAT L 2 A2M 3952 LEP L 2 A2M 4035 LRP1 L 2 A2M 4803 NGFB L 2 A2M 5047 PAEP L 2 A2M 7045 TGFBI L 2 A2M 8728 ADAM19 L 2 A2M 9510 ADAMTS1 L 2 A2M 10944 SMAP S 2 A2M 55729 ATF7IP L 9 NAT1 8260 ARD1A L 12 SERPINA3 351 APP L 12 SERPINA3 354 KLK3 L 12 SERPINA3 1215 CMA1 L 12 SERPINA3 1504 CTRB1 L 12 SERPINA3 1506 CTRL L 12 SERPINA3 1511 CTSG L 12 SERPINA3 1990 ELA1 L 12 SERPINA3 1991 ELA2 L 12 SERPINA3 2064 ERBB2 L 12 SERPINA3 2153 F5 L 12 SERPINA3 3817 KLK2 L 12 SERPINA3 4035 LRP1 L 12 SERPINA3 4485 MST1 L 12 SERPINA3 5422 POLA L 12 SERPINA3 64215 DNAJC1 L 14 AAMP 51497 TH1L S 15 AANAT 7534 YWHAZ L 18 ABAT 7915 ALDH5A1 L 19 ABCA1 335 APOA1 L 19 ABCA1 6645 SNTB2 L 19 ABCA1 8772 FADD L 20 ABCA2 55755 CDK5RAP2 L 22 ABCB7 2235 FECH L 23 ABCF1 3692 ITGB4BP S 24 ABCA4 1258 CNGB1 L 25 ABL1 27 ABL2 L 25 ABL1 472 ATM L 25 ABL1 613 BCR L 25 ABL1 718 C3 L 25 ABL1 867 CBL L 25 ABL1 1501 CTNND2 L 25 ABL1 2048 EPHB2 L 25 ABL1 2547 XRCC6 L 25 ABL1 2876 GPX1 L 25 ABL1 2885 GRB2 L 25 ABL1 3055 HCK L 25 ABL1 3636 INPPL1 L 25 ABL1 3716 JAK1 L 25 ABL1 4193 MDM2 L 25 ABL1 4690 NCK1 L 25 ABL1 4914 NTRK1 L 25 ABL1 5062 PAK2 L 25 ABL1 5295 PIK3R1 L 25 ABL1 5335 PLCG1 L 25 ABL1 5591