MED12 Mutation in Two Families with X-Linked Ohdo Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

New Microdeletion and Microduplication Syndromes: a Comprehensive Review
Genetics and Molecular Biology, 37, 1 (suppl), 210-219 (2014) Copyright © 2014, Sociedade Brasileira de Genética. Printed in Brazil www.sbg.org.br Review Article New microdeletion and microduplication syndromes: A comprehensive review Julián Nevado1,2*, Rafaella Mergener3*, María Palomares-Bralo1,2, Karen Regina Souza3, Elena Vallespín1,2, Rocío Mena1,2, Víctor Martínez-Glez1,2, María Ángeles Mori1,2, Fernando Santos1,4, Sixto García-Miñaur1,4, Fé García-Santiago1,5, Elena Mansilla1,5, Luis Fernández1,6, María Luisa de Torres1,5, Mariluce Riegel3,7$ and Pablo Lapunzina1,4,8$ 1Centro de Investigación Biomédica en Red de Enfermedades Raras, Instituto de Salud Carlos III, Madrid, Spain. 2Section of Functional and Structural Genomics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 3Programa de Pós-graduação em Genética e Biologia Molecular, Universidade Federal do Rio Grande do Sul, Porto Alegre,RS, Brazil. 4Section of Clinical Genetics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 5Section of Cytogenetics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 6Section of Preanalytics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 7Serviço de Genética Médica, Hospital de Clínicas de Porto Alegre, Porto Alegre ,RS, Brazil. 8Section of Molecular Endocrinology, Overgrowth Disordes Laboratory, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. Abstract Several new microdeletion and microduplication syndromes are emerging as disorders that have been proven to cause multisystem pathologies frequently associated with intellectual disability (ID), multiple congenital anomalies (MCA), autistic spectrum disorders (ASD) and other phenotypic findings. In this paper, we review the “new” and emergent microdeletion and microduplication syndromes that have been described and recognized in recent years with the aim of summarizing their main characteristics and chromosomal regions involved. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

Level Estimates of Maternal Smoking and Nicotine Replacement Therapy During Pregnancy
Using primary care data to assess population- level estimates of maternal smoking and nicotine replacement therapy during pregnancy Nafeesa Nooruddin Dhalwani BSc MSc Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy November 2014 ABSTRACT Background: Smoking in pregnancy is the most significant preventable cause of poor health outcomes for women and their babies and, therefore, is a major public health concern. In the UK there is a wide range of interventions and support for pregnant women who want to quit. One of these is nicotine replacement therapy (NRT) which has been widely available for retail purchase and prescribing to pregnant women since 2005. However, measures of NRT prescribing in pregnant women are scarce. These measures are vital to assess its usefulness in smoking cessation during pregnancy at a population level. Furthermore, evidence of NRT safety in pregnancy for the mother and child’s health so far is nebulous, with existing studies being small or using retrospectively reported exposures. Aims and Objectives: The main aim of this work was to assess population- level estimates of maternal smoking and NRT prescribing in pregnancy and the safety of NRT for both the mother and the child in the UK. Currently, the only population-level data on UK maternal smoking are from repeated cross-sectional surveys or routinely collected maternity data during pregnancy or at delivery. These obtain information at one point in time, and there are no population-level data on NRT use available. As a novel approach, therefore, this thesis used the routinely collected primary care data that are currently available for approximately 6% of the UK population and provide longitudinal/prospectively recorded information throughout pregnancy. -

Prenatal Diagnosis of Frequently Seen Fetal Syndromes (AZ)
Prenatal diagnosis of frequently seen fetal syndromes (A-Z) Ibrahim Bildirici,MD Professor of OBGYN ACIBADEM University SOM Attending Perinatologist ACIBADEM MASLAK Hospital Amniotic band sequence: Amniotic band sequence refers to a highly variable spectrum of congenital anomalies that occur in association with amniotic bands The estimated incidence of ABS ranges from 1:1200 to 1:15,000 in live births, and 1:70 in stillbirths Anomalies include: Craniofacial abnormalities — eg, encephalocele, exencephaly, clefts, which are often in unusual locations; anencephaly. Body wall defects (especially if not in the midline), abdominal or thoracic contents may herniate through a body wall defect and into the amniotic cavity. Limb defects — constriction rings, amputation, syndactyly, clubfoot, hand deformities, lymphedema distal to a constriction ring. Visceral defects — eg, lung hypoplasia. Other — Autotransplanted tissue on skin tags, spinal defects, scoliosis, ambiguous genitalia, short umbilical cord due to restricted motion of the fetus Arthrogryposis •Multiple congenital joint contractures/ankyloses involving two or more body areas •Pena Shokeir phenotype micrognathia, multiple contractures, camptodactyly (persistent finger flexion), polyhydramnios *many are AR *Lethal due to pulmonary hypoplasia • Distal arthrogryposis Subset of non-progressive contractures w/o associated primary neurologic or muscle disease Beckwith Wiedemannn Syndrome Macrosomia Hemihyperplasia Macroglossia Ventral wall defects Predisposition to embryonal tumors Neonatal hypoglycemia Variable developmental delay 85% sporadic with normal karyotype 10-15% autosomal dominant inheritance 10-20% with paternal uniparental disomy (Both copies of 11p15 derived from father) ***Imprinting related disorder 1/13 000. Binder Phenotype a flat profile and depressed nasal bridge. Short nose, short columella, flat naso-labial angle and perialar flattening Isolated Binder Phenotype transmission would be autosomal dominant Binder Phenotype can also be an important sign of chondrodysplasia punctata (CDDP) 1. -

MED12 Mutations Link Intellectual Disability Syndromes with Dysregulated GLI3-Dependent Sonic Hedgehog Signaling
MED12 mutations link intellectual disability syndromes with dysregulated GLI3-dependent Sonic Hedgehog signaling Haiying Zhoua, Jason M. Spaethb, Nam Hee Kimb, Xuan Xub, Michael J. Friezc, Charles E. Schwartzc, and Thomas G. Boyerb,1 aDepartment of Molecular and Cell Biology, Howard Hughes Medical Institute, University of California, Berkeley, CA 94270; bDepartment of Molecular Medicine, Institute of Biotechnology, University of Texas Health Science Center at San Antonio, San Antonio, TX 78229; and cGreenwood Genetic Center, Greenwood, SC 29646 Edited by Robert G. Roeder, The Rockefeller University, New York, NY, and approved September 13, 2012 (received for review December 20, 2011) Recurrent missense mutations in the RNA polymerase II Mediator divergent “tail” and “kinase” modules through which most activa- subunit MED12 are associated with X-linked intellectual disability tors and repressors target Mediator. The kinase module, compris- (XLID) and multiple congenital anomalies, including craniofacial, ing MED12, MED13, CDK8, and cyclin C, has been ascribed both musculoskeletal, and behavioral defects in humans with FG (or activating and repressing functions and exists in variable association Opitz-Kaveggia) and Lujan syndromes. However, the molecular with Mediator, implying that its regulatory role is restricted to a mechanism(s) underlying these phenotypes is poorly understood. subset of RNA polymerase II transcribed genes. Here we report that MED12 mutations R961W and N1007S causing Within the Mediator kinase module, MED12 is a critical trans- FG and Lujan syndromes, respectively, disrupt a Mediator-imposed ducer of regulatory information conveyed by signal-activated transcription factors linked to diverse developmental pathways, constraint on GLI3-dependent Sonic Hedgehog (SHH) signaling. We including the EGF, Notch, Wnt, and Hedgehog pathways (10–12). -

(12) Patent Application Publication (10) Pub. No.: US 2010/0210567 A1 Bevec (43) Pub
US 2010O2.10567A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0210567 A1 Bevec (43) Pub. Date: Aug. 19, 2010 (54) USE OF ATUFTSINASATHERAPEUTIC Publication Classification AGENT (51) Int. Cl. A638/07 (2006.01) (76) Inventor: Dorian Bevec, Germering (DE) C07K 5/103 (2006.01) A6IP35/00 (2006.01) Correspondence Address: A6IPL/I6 (2006.01) WINSTEAD PC A6IP3L/20 (2006.01) i. 2O1 US (52) U.S. Cl. ........................................... 514/18: 530/330 9 (US) (57) ABSTRACT (21) Appl. No.: 12/677,311 The present invention is directed to the use of the peptide compound Thr-Lys-Pro-Arg-OH as a therapeutic agent for (22) PCT Filed: Sep. 9, 2008 the prophylaxis and/or treatment of cancer, autoimmune dis eases, fibrotic diseases, inflammatory diseases, neurodegen (86). PCT No.: PCT/EP2008/007470 erative diseases, infectious diseases, lung diseases, heart and vascular diseases and metabolic diseases. Moreover the S371 (c)(1), present invention relates to pharmaceutical compositions (2), (4) Date: Mar. 10, 2010 preferably inform of a lyophilisate or liquid buffersolution or artificial mother milk formulation or mother milk substitute (30) Foreign Application Priority Data containing the peptide Thr-Lys-Pro-Arg-OH optionally together with at least one pharmaceutically acceptable car Sep. 11, 2007 (EP) .................................. O7017754.8 rier, cryoprotectant, lyoprotectant, excipient and/or diluent. US 2010/0210567 A1 Aug. 19, 2010 USE OF ATUFTSNASATHERAPEUTIC ment of Hepatitis BVirus infection, diseases caused by Hepa AGENT titis B Virus infection, acute hepatitis, chronic hepatitis, full minant liver failure, liver cirrhosis, cancer associated with Hepatitis B Virus infection. 0001. The present invention is directed to the use of the Cancer, Tumors, Proliferative Diseases, Malignancies and peptide compound Thr-Lys-Pro-Arg-OH (Tuftsin) as a thera their Metastases peutic agent for the prophylaxis and/or treatment of cancer, 0008. -

11 Selected Syndromes and Associations
11 Selected Syndromes and Associations ĭ Apert Syndrome Definition: Also known as acrocephalic syndac- Other anomalies of the cardiac, renal, and tyly syndrome. It is characterized by a “tower- gastrointestinal systems may also be present. shaped” head, facial dysmorphism, and sym- metrical syndactyly of the fingers and toes. Ultrasound findings: The earliest prenatal diag- nosis was possible at 12 weeks of gestation with Incidence: about one in 100 000 births. nuchal translucency measurements. Syndactyly First described in 1906 by Apert. could also be detected at this stage. At a later stage, an unusual shape of the head resulting Etiology/genetics: Partly autosomal-dominant from premature closure of the cranial sutures inheritance, but frequently sporadic occurrence (tower-shaped head) and facial dysmorphism (new mutation). Advanced paternal age is a fac- (hypoplasia of the midfacial region) are charac- tor favoring its occurrence. Gene defect in the fi- teristic features. Detailed scanning may also re- broblast growth factor receptor-2 gene (FGFR2), veal deep-set ears, unusual shape of the nose, gene locus: 10q26. exophthalmos, and hypertelorism. Clinical features: “Tower-shaped” head, early Differential diagnosis: Carpenter syndrome, closure of cranial sutures, anomalies of the cervi- Crouzon syndrome, cloverleaf skull anomaly, cal vertebral column. Facial anomalies: denting Pfeiffer syndrome, thanatophoric dysplasia, of the forehead in the supraorbital region, hyper- achondrogenesis, Cornelia de Lange syndrome, telorism, flat orbital bone, exophthalmos, squint, EEC syndrome, Fryns syndrome, Joubert syn- deep-set ears, small, beak-shaped nose, syndac- drome, multiple pterygium syndrome, Noonan tyly (as extreme as “spoon hands”), fusion of the syndrome, Roberts syndrome, Smith–Lemli– bony parts of fingers II–IV, short fingers, possibly Opitz syndrome, trisomy 21. -

VACTERL/VATER Association Benjamin D Solomon
Solomon Orphanet Journal of Rare Diseases 2011, 6:56 http://www.ojrd.com/content/6/1/56 REVIEW Open Access VACTERL/VATER Association Benjamin D Solomon Abstract VACTERL/VATER association is typically defined by the presence of at least three of the following congenital malformations: vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities. In addition to these core component features, patients may also have other congenital anomalies. Although diagnostic criteria vary, the incidence is estimated at approximately 1 in 10,000 to 1 in 40,000 live-born infants. The condition is ascertained clinically by the presence of the above-mentioned malformations; importantly, there should be no clinical or laboratory-based evidence for the presence of one of the many similar conditions, as the differential diagnosis is relatively large. This differential diagnosis includes (but is not limited to) Baller-Gerold syndrome, CHARGE syndrome, Currarino syndrome, deletion 22q11.2 syndrome, Fanconi anemia, Feingold syndrome, Fryns syndrome, MURCS association, oculo-auriculo-vertebral syndrome, Opitz G/BBB syndrome, Pallister- Hall syndrome, Townes-Brocks syndrome, and VACTERL with hydrocephalus. Though there are hints regarding causation, the aetiology has been identified only in a small fraction of patients to date, likely due to factors such as a high degree of clinical and causal heterogeneity, the largely sporadic nature of the disorder, and the presence of many similar conditions. New genetic research methods offer promise that the causes of VACTERL association will be better defined in the relatively near future. Antenatal diagnosis can be challenging, as certain component features can be difficult to ascertain prior to birth. -

Craniosynostosis Precision Panel Overview Indications Clinical Utility
Craniosynostosis Precision Panel Overview Craniosynostosis is defined as the premature fusion of one or more cranial sutures, often resulting in abnormal head shape. It is a developmental craniofacial anomaly resulting from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). As well, craniosynostosis can be simple when only one suture fuses prematurely or complex/compound when there is a premature fusion of multiple sutures. Complex craniosynostosis are usually associated with other body deformities. The main morbidity risk is the elevated intracranial pressure and subsequent brain damage. When left untreated, craniosynostosis can cause serious complications such as developmental delay, facial abnormality, sensory, respiratory and neurological dysfunction, eye anomalies and psychosocial disturbances. In approximately 85% of the cases, this disease is isolated and nonsyndromic. Syndromic craniosynostosis usually present with multiorgan complications. The Igenomix Craniosynostosis Precision Panel can be used to make a directed and accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Craniosynostosis Precision Panel is indicated for those patients with a clinical diagnosis or suspicion with or without the following manifestations: ‐ Microcephaly ‐ Scaphocephaly (elongated head) ‐ Anterior plagiocephaly ‐ Brachycephaly ‐ Torticollis ‐ Frontal bossing Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. - Early initiation of treatment in the form surgical procedures to relieve fused sutures, midface advancement, limited phase of orthodontic treatment and combined 1 orthodontics/orthognathic surgery treatment. -

Malformation Syndromes: a Review of Mouse/Human Homology
J Med Genet: first published as 10.1136/jmg.25.7.480 on 1 July 1988. Downloaded from Joalrn(ll of Medical Genetics 1988, 25, 480-487 Malformation syndromes: a review of mouse/human homology ROBIN M WINTER Fromii the Kennetivdy Galton Centre, Clinlicail Research Centre, Northiwick Park Hospital, Harrow, Middlesex HAI 3UJ. SUMMARY The purpose of this paper is to review the known and possible homologies between mouse and human multiple congenital anomaly syndromes. By identifying single gene defects causing similar developmental abnormalities in mouse and man, comparative gene mapping can be carried out, and if the loci in mouse and man are situated in homologous chromosome segments, further molecular studies can be performed to show that the loci are identical. This paper puts forward tentative homologies in the hope that some will be investigated and shown to be true homologies at the molecular level, thus providing mouse models for complex developmental syndromes. The mouse malformation syndromes are reviewed according to their major gene effects. X linked syndromes are reviewed separately because of the greater ease of establishing homology for these conditions. copyright. The purpose of this paper is to review the known even phenotypic similarity would be no guarantee and possible homologies between mouse and human that such genes in man and mouse are homologous". genetic malformation syndromes. Lalley and By identifying single gene defects causing similar following criteria for developmental abnormalities in mouse and man, McKusick' recommend the http://jmg.bmj.com/ identifying gene homologies between species: comparative gene mapping can be carried out, and if (1) Similar nucleotide or amino acid sequence. -

Approach to the Genetic Diagnosis of Autism Why Genetics? Why
11/2/2013 Approach to the Genetic Diagnosis of Autism Margaret Rieley, MD November 2, 2013 Why Genetics? 1:2500 (1980s) 1:88 to 1:100 (current) >500% increase over the last 20 years Declared “epidemic” 4-5 times more prevalent in boys Present in all racial, ethnic, social groups High heritability MZ twins 60-90% concordance DZ twins 0-10% concordance Why Genetics? Examine and evaluate patient and family members Determine etiology Definitive diagnosis helps patient acquire services Provide information on prognosis Screen and potentially prevent morbidity Counsel on recurrence risk Targeted therapies (metabolic disorders, FXS) Empower the family by knowledge of underlying cause 1 11/2/2013 Evaluation Scheme (ACMG) Pre-evaluation ◦ Accurate ASD diagnosis ◦ Sensory screening: complete audiogram ◦ Cognitive testing ◦ EEG (if seizures suspected) ◦ Verify newborn screening results ◦ Prenatal history (GA, Wt, parental ages, exposures) ◦ Karyotype ◦ Fragile X (AAP recommendations) Tier 1 - Physical Exam Evaluation for known syndromes or associated conditions Intellectual disability (ID) (75%) Dysmorphic features and epilepsy (25%) MRI and EEG abnormalities (less common) Microceppyhaly (()10%) Macrocephaly (20–40%) Congenital anomaly (6% vs. 3% in gen pop) ◦ Congenital anomalies double risk of autism (0.4% vs. 0.2% in gen pop) ◦ Brain and eye more likely to be associated with autism Majority are nondysmorphic with no other medical features suggestive of a syndrome 1st Tier, continued Woods lamp exam Targeted testing if specific diagnosis is considered ◦ Rubella titers Rare (<10 cases/yr) Sensorineural deafness (58%) Eye abnormalities—retinopathy, cataract and microphthalmia (43%) Congenital heart disease (50%) ◦ “Standard” metabolic screening clinical indicators present suspected condition not screened for on NB screening ◦ Urine mucopolysaccharides and organic acids ◦ Serum lacate, amino acids, ammonia, acyl-carnitine profile, CK, LFTs. -
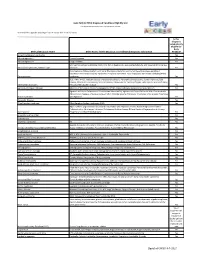
Early ACCESS Diagnosed Conditions List
Iowa Early ACCESS Diagnosed Conditions Eligibility List List adapted with permission from Early Intervention Colorado To search for a specific word type "Ctrl F" to use the "Find" function. Is this diagnosis automatically eligible for Early Medical Diagnosis Name Other Names for the Diagnosis and Additional Diagnosis Information ACCESS? 6q terminal deletion syndrome Yes Achondrogenesis I Parenti-Fraccaro Yes Achondrogenesis II Langer-Saldino Yes Schinzel Acrocallosal syndrome; ACLS; ACS; Hallux duplication, postaxial polydactyly, and absence of the corpus Acrocallosal syndrome, Schinzel Type callosum Yes Acrodysplasia; Arkless-Graham syndrome; Maroteaux-Malamut syndrome; Nasal hypoplasia-peripheral dysostosis-intellectual disability syndrome; Peripheral dysostosis-nasal hypoplasia-intellectual disability (PNM) Acrodysostosis syndrome Yes ALD; AMN; X-ALD; Addison disease and cerebral sclerosis; Adrenomyeloneuropathy; Siemerling-creutzfeldt disease; Bronze schilder disease; Schilder disease; Melanodermic Leukodystrophy; sudanophilic leukodystrophy; Adrenoleukodystrophy Pelizaeus-Merzbacher disease Yes Agenesis of Corpus Callosum Absence of the corpus callosum; Hypogenesis of the corpus callosum; Dysplastic corpus callosum Yes Agenesis of Corpus Callosum and Chorioretinal Abnormality; Agenesis of Corpus Callosum With Chorioretinitis Abnormality; Agenesis of Corpus Callosum With Infantile Spasms And Ocular Anomalies; Chorioretinal Anomalies Aicardi syndrome with Agenesis Yes Alexander Disease Yes Allan Herndon syndrome Allan-Herndon-Dudley