(12) Patent Application Publication (10) Pub. No.: US 2010/0210567 A1 Bevec (43) Pub
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FROGLOG Newsletter of the Declining Amphibian Populations Task Force
Salamandra salamandra by Franco Andreone ISSN 1026-0269 FROGLOG Newsletter of the Declining Amphibian Populations Task Force August 2004, Number 64. Meteyer et al. (2000) and Ouellet very low number of abnormalities. We (2000). only found one L. kuhlii, which may We examined a total of 4,331 have strayed from a nearby stream. frogs of 23 species and found 20 A third of abnormalities were types of deformities in 9 species of due to trauma; these included digit frogs. We divided deformities into two amputations (16% of all general types: developmental abnormalities), limb amputations (2%), abnormalities and trauma (injuries). fractured limbs (7%) and skin wounds Morphological Abnormalities in We distinguished trauma (4%). The most common Frogs of West Java, Indonesia abnormalities based on the developmental abnormalities were appearance of old scars or, if they digital (43%) and, of these, By Mirza D. Kusrini, Ross A. Alford, involved digits, the occurrence of brachydactyly (16.3%), syndactyly Anisa Fitri, Dede M. Nasir, Sumantri digital re-growth. Developmental (14.6%) and ectrodactyly (11.4%) Rahardyansah abnormalities occurred in limbs were the three most common. In recent decades, amphibian (amelia, micromelia, brachymelia, The oldest specimen of F. deformities have generated public hemimelia, ectromelia, taumelia, cuta- limnocharis stored in the MZB that interest as high incidences have been neous fusions), digits (ectrodactyly, exhibited abnormalities was a juvenile found in several locations, notably in brachydactyly, syndactyly, polydactyly, frog captured on 16 November 1921 North America (Helgen et al., 1998; clinodactyly), the back-bone (scoli- from Bogor without one leg (amelia) Ouellet, 2000). The only report on the osis), the eyes (anophthalmy) and the (ID057.10). -
2016 IES Annual Meeting Final Programme
ROYAL ACADEMY OF MEDICINE IN IRELAND IRISH JOURNAL OF MEDICAL SCIENCE Irish Endocrine Society 40th Annual Meeting 14th and 15th October 2016 Stormont Hotel, Belfast Local Organiser: Doctor Hamish Courtney, REVISEDRoyal Victoria Hospital, PROOF Belfast Irish Journal of Medical Science Volume XXX Supplement X DOI 10.1007/s11845-016-1482-y 123 123 Journal : Large 11845 Dispatch : 17-8-2016 Pages : 57 Article No. : 1482 h LE h TYPESET MS Code : 1482 h44CP h DISK Ir J Med Sci Disclosure statement This supplement is paid for by the Irish Endocrine Society. However the meeting costs are supported by the following commercial sponsors: Abbott Amgen Astra Zeneca Besins Healthcare BMS Boehringer Ingleheim Consilient Ipsen Janssen-Cilag Kyowa Kirin Lilly Menarini Merck Serono MSD Novartis Novo Nordisk Pfizer Sanofi REVISED PROOF 123 Journal : Large 11845 Dispatch : 17-8-2016 Pages : 57 Article No. : 1482 h LE h TYPESET MS Code : 1482 h44CP h DISK Ir J Med Sci Novo Lecture Nordisk Lecture 1976 D.K. O’Donovan 1977 S. Bloom 1978 J.H.S. Robertson 1979 A.G. Cudworth 1980 D.A.D. Montgomery 1981 Peter Watkins 1982 G. Joplin 1983 D.R. London 1984 A.X. Bertagna 1985 Malcolm Nattrass Laurence Kennedy 1986 Brian Frier JB Ferriss 1987 Maurice Scanlon TJ McKenna 1988 D.A. Heath AB Atkinson 1989 J. Ward GH Tomkin 1990 R. Volpe KD Buchanan 1991 Michael Besser PPA Smyth 1992 R.V. Ragontte DH Hadden 1993 Bruce Weintraub David Powell 1994 Oscar Croffard Patrick Bell 1995 Robert Lindsay Brian Sheridan 1996 C.R.W. Edwards Rosemary Freaney 1997 Stephanie Amiel David McCance 1998 Robert Turner Randle Hayes 1999 Ian Hay Sean K Cunningham 2000 Stephen O’Rahilly Michael Cullen 2001 Andre Lacroix Daphne Owens 2002 J. -

New Microdeletion and Microduplication Syndromes: a Comprehensive Review
Genetics and Molecular Biology, 37, 1 (suppl), 210-219 (2014) Copyright © 2014, Sociedade Brasileira de Genética. Printed in Brazil www.sbg.org.br Review Article New microdeletion and microduplication syndromes: A comprehensive review Julián Nevado1,2*, Rafaella Mergener3*, María Palomares-Bralo1,2, Karen Regina Souza3, Elena Vallespín1,2, Rocío Mena1,2, Víctor Martínez-Glez1,2, María Ángeles Mori1,2, Fernando Santos1,4, Sixto García-Miñaur1,4, Fé García-Santiago1,5, Elena Mansilla1,5, Luis Fernández1,6, María Luisa de Torres1,5, Mariluce Riegel3,7$ and Pablo Lapunzina1,4,8$ 1Centro de Investigación Biomédica en Red de Enfermedades Raras, Instituto de Salud Carlos III, Madrid, Spain. 2Section of Functional and Structural Genomics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 3Programa de Pós-graduação em Genética e Biologia Molecular, Universidade Federal do Rio Grande do Sul, Porto Alegre,RS, Brazil. 4Section of Clinical Genetics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 5Section of Cytogenetics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 6Section of Preanalytics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 7Serviço de Genética Médica, Hospital de Clínicas de Porto Alegre, Porto Alegre ,RS, Brazil. 8Section of Molecular Endocrinology, Overgrowth Disordes Laboratory, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. Abstract Several new microdeletion and microduplication syndromes are emerging as disorders that have been proven to cause multisystem pathologies frequently associated with intellectual disability (ID), multiple congenital anomalies (MCA), autistic spectrum disorders (ASD) and other phenotypic findings. In this paper, we review the “new” and emergent microdeletion and microduplication syndromes that have been described and recognized in recent years with the aim of summarizing their main characteristics and chromosomal regions involved. -

Differential Diagnosis of Oromandibular Limb Hypogenesis Syndromes Ole Junga,B, Ralf Smeetsb, Henning Hankenb, Reinhard E
Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2016 Jun; 160(2):310-315. A patient with Charlie M Syndrome: Differential diagnosis of Oromandibular Limb Hypogenesis Syndromes Ole Junga,b, Ralf Smeetsb, Henning Hankenb, Reinhard E. Friedrichb, Max Heilandb, Amir Tagnihaa, Brian Labowa Aim. In order to provide adequate treatment to a patient with a subtype of Oromandibular Limb Hypogenesis Syndromes (OLHS), this study aimed to review and to analyze the current literature and treatment options of OLHS. Methods. Literature review in PubMed and Sciencedirect. Due to the small number of results, all available references were analyzed precisely. Results. Cases of OLHS are formerly rare and often incomplete. There are various classifications available, which, however, often seem confusing and are of little practical relevance. Furthermore, we present a complete case report of a patient with Charlie M syndrome, a type IV (Chicarilli)/ V (Hall) OLHS malformation. We also describe embryologic pathogenesis and differential diagnoses. Conclusion. As a result of our literature review, we recommend an adjusted classification for OLHS. Key words: Oromandibular Limb Hypogenesis Syndromes (OLHS), Charlie M Syndrome, Oromandibular and limb hypogenesis malformations (OLHM) Received: August 1, 2015; Accepted with revision: April 8, 2016; Available online: April 27, 2016 http://dx.doi.org/10.5507/bp.2016.020 aDepartment of Plastic and Oral Surgery, Children´s Hospital Boston, Harvard Medical School, Boston, USA bDepartment of Oral and Maxillofacial Surgery, University Medical Center Hamburg, Hamburg, Germany Corresponding author: Ole Jung, e-mail: [email protected] INTRODUCTION CASE REPORT Oromandibular Limb Hypogenesis Syndromes A twenty-three-year-old male with severe oroman- (OLHS) describe a group of heterogeneous malforma- dibular and limb deformities presented for mandibular tions of the face and body. -
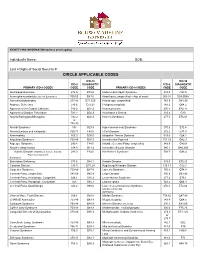
Circle Applicable Codes
IDENTIFYING INFORMATION (please print legibly) Individual’s Name: DOB: Last 4 Digits of Social Security #: CIRCLE APPLICABLE CODES ICD-10 ICD-10 ICD-9 DIAGNOSTIC ICD-9 DIAGNOSTIC PRIMARY ICD-9 CODES CODE CODE PRIMARY ICD-9 CODES CODE CODE Abetalipoproteinemia 272.5 E78.6 Hallervorden-Spatz Syndrome 333.0 G23.0 Acrocephalosyndactyly (Apert’s Syndrome) 755.55 Q87.0 Head Injury, unspecified – Age of onset: 959.01 S09.90XA Adrenaleukodystrophy 277.86 E71.529 Hemiplegia, unspecified 342.9 G81.90 Arginase Deficiency 270.6 E72.21 Holoprosencephaly 742.2 Q04.2 Agenesis of the Corpus Callosum 742.2 Q04.3 Homocystinuria 270.4 E72.11 Agenesis of Septum Pellucidum 742.2 Q04.3 Huntington’s Chorea 333.4 G10 Argyria/Pachygyria/Microgyria 742.2 Q04.3 Hurler’s Syndrome 277.5 E76.01 or 758.33 Aicardi Syndrome 333 G23.8 Hyperammonemia Syndrome 270.6 E72.4 Alcohol Embryo and Fetopathy 760.71 F84.5 I-Cell Disease 272.2 E77.0 Anencephaly 655.0 Q00.0 Idiopathic Torsion Dystonia 333.6 G24.1 Angelman Syndrome 759.89 Q93.5 Incontinentia Pigmenti 757.33 Q82.3 Asperger Syndrome 299.8 F84.5 Infantile Cerebral Palsy, unspecified 343.9 G80.9 Ataxia-Telangiectasia 334.8 G11.3 Intractable Seizure Disorder 345.1 G40.309 Autistic Disorder (Childhood Autism, Infantile 299.0 F84.0 Klinefelter’s Syndrome 758.7 Q98.4 Psychosis, Kanner’s Syndrome) Biotinidase Deficiency 277.6 D84.1 Krabbe Disease 333.0 E75.23 Canavan Disease 330.0 E75.29 Kugelberg-Welander Disease 335.11 G12.1 Carpenter Syndrome 759.89 Q87.0 Larsen’s Syndrome 755.8 Q74.8 Cerebral Palsy, unspecified 343.69 G80.9 -

2018 Etiologies by Frequencies
2018 Etiologies in Order of Frequency by Category Hereditary Syndromes and Disorders Count CHARGE Syndrome 958 Down syndrome (Trisomy 21 syndrome) 308 Usher I syndrome 252 Stickler syndrome 130 Dandy Walker syndrome 119 Cornelia de Lange 102 Goldenhar syndrome 98 Usher II syndrome 83 Wolf-Hirschhorn syndrome (Trisomy 4p) 68 Trisomy 13 (Trisomy 13-15, Patau syndrome) 60 Pierre-Robin syndrome 57 Moebius syndrome 55 Trisomy 18 (Edwards syndrome) 52 Norrie disease 38 Leber congenital amaurosis 35 Chromosome 18, Ring 18 31 Aicardi syndrome 29 Alstrom syndrome 27 Pfieffer syndrome 27 Treacher Collins syndrome 27 Waardenburg syndrome 27 Marshall syndrome 25 Refsum syndrome 21 Cri du chat syndrome (Chromosome 5p- synd) 16 Bardet-Biedl syndrome (Laurence Moon-Biedl) 15 Hurler syndrome (MPS I-H) 15 Crouzon syndrome (Craniofacial Dysotosis) 13 NF1 - Neurofibromatosis (von Recklinghausen dis) 13 Kniest Dysplasia 12 Turner syndrome 11 Usher III syndrome 10 Cockayne syndrome 9 Apert syndrome/Acrocephalosyndactyly, Type 1 8 Leigh Disease 8 Alport syndrome 6 Monosomy 10p 6 NF2 - Bilateral Acoustic Neurofibromatosis 6 Batten disease 5 Kearns-Sayre syndrome 5 Klippel-Feil sequence 5 Hereditary Syndromes and Disorders Count Prader-Willi 5 Sturge-Weber syndrome 5 Marfan syndrome 3 Hand-Schuller-Christian (Histiocytosis X) 2 Hunter Syndrome (MPS II) 2 Maroteaux-Lamy syndrome (MPS VI) 2 Morquio syndrome (MPS IV-B) 2 Optico-Cochleo-Dentate Degeneration 2 Smith-Lemli-Opitz (SLO) syndrome 2 Wildervanck syndrome 2 Herpes-Zoster (or Hunt) 1 Vogt-Koyanagi-Harada -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

Genetics of Congenital Hand Anomalies
G. C. Schwabe1 S. Mundlos2 Genetics of Congenital Hand Anomalies Die Genetik angeborener Handfehlbildungen Original Article Abstract Zusammenfassung Congenital limb malformations exhibit a wide spectrum of phe- Angeborene Handfehlbildungen sind durch ein breites Spektrum notypic manifestations and may occur as an isolated malforma- an phänotypischen Manifestationen gekennzeichnet. Sie treten tion and as part of a syndrome. They are individually rare, but als isolierte Malformation oder als Teil verschiedener Syndrome due to their overall frequency and severity they are of clinical auf. Die einzelnen Formen kongenitaler Handfehlbildungen sind relevance. In recent years, increasing knowledge of the molecu- selten, besitzen aber aufgrund ihrer Häufigkeit insgesamt und lar basis of embryonic development has significantly enhanced der hohen Belastung für Betroffene erhebliche klinische Rele- our understanding of congenital limb malformations. In addi- vanz. Die fortschreitende Erkenntnis über die molekularen Me- tion, genetic studies have revealed the molecular basis of an in- chanismen der Embryonalentwicklung haben in den letzten Jah- creasing number of conditions with primary or secondary limb ren wesentlich dazu beigetragen, die genetischen Ursachen kon- involvement. The molecular findings have led to a regrouping of genitaler Malformationen besser zu verstehen. Der hohe Grad an malformations in genetic terms. However, the establishment of phänotypischer Variabilität kongenitaler Handfehlbildungen er- precise genotype-phenotype correlations for limb malforma- schwert jedoch eine Etablierung präziser Genotyp-Phänotyp- tions is difficult due to the high degree of phenotypic variability. Korrelationen. In diesem Übersichtsartikel präsentieren wir das We present an overview of congenital limb malformations based Spektrum kongenitaler Malformationen, basierend auf einer ent- 85 on an anatomic and genetic concept reflecting recent molecular wicklungsbiologischen, anatomischen und genetischen Klassifi- and developmental insights. -

Level Estimates of Maternal Smoking and Nicotine Replacement Therapy During Pregnancy
Using primary care data to assess population- level estimates of maternal smoking and nicotine replacement therapy during pregnancy Nafeesa Nooruddin Dhalwani BSc MSc Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy November 2014 ABSTRACT Background: Smoking in pregnancy is the most significant preventable cause of poor health outcomes for women and their babies and, therefore, is a major public health concern. In the UK there is a wide range of interventions and support for pregnant women who want to quit. One of these is nicotine replacement therapy (NRT) which has been widely available for retail purchase and prescribing to pregnant women since 2005. However, measures of NRT prescribing in pregnant women are scarce. These measures are vital to assess its usefulness in smoking cessation during pregnancy at a population level. Furthermore, evidence of NRT safety in pregnancy for the mother and child’s health so far is nebulous, with existing studies being small or using retrospectively reported exposures. Aims and Objectives: The main aim of this work was to assess population- level estimates of maternal smoking and NRT prescribing in pregnancy and the safety of NRT for both the mother and the child in the UK. Currently, the only population-level data on UK maternal smoking are from repeated cross-sectional surveys or routinely collected maternity data during pregnancy or at delivery. These obtain information at one point in time, and there are no population-level data on NRT use available. As a novel approach, therefore, this thesis used the routinely collected primary care data that are currently available for approximately 6% of the UK population and provide longitudinal/prospectively recorded information throughout pregnancy. -

CHARGE Syndrome
orphananesthesia Anaesthesia recommendations for CHARGE syndrome Disease name: CHARGE syndrome ICD 10: Q87.8 Synonyms: CHARGE association; Hall-Hittner syndrome Disease summary: CHARGE syndrome was initially defined as a non-random association of anomalies: - Coloboma - Heart defect - Atresia choanae (choanal atresia) - Retarded growth and development - Genital hypoplasia - Ear anomalies/deafness In 1998, an expert group defined the major (the classical 4C´s: Choanal atresia, Coloboma, Characteristic ear and Cranial nerve anomalies) and minor criteria of CHARGE syndrome [1]. In 2004, mutations in the CHD7 gene were identified as the major cause. The inheritance pattern is autosomal dominant with variable expressivity. Almost all mutations occurs de novo, but parent-to-child transmission has occasionally been reported [2]. Clinical criteria for CHARGE syndrome [1] Major criteria: • Coloboma • Choanal Atresia • Cranial nerve anomalies • Abnormalities of the inner, middle, or external ear Minor criteria: • Cardiaovascular malformations • Genital hypoplasia or delayed pubertal development • Cleft lip and/or palate • Tracheoesophageal defects • Distinctive CHARGE facies • Growth retardation • Developmental delay Occasional: • Renal anomalies: duplex system, vesicoureteric reflux • Spinal anomalies: scoliosis, osteoporosis • Hand anomalies 1 • Neck/shoulder anomalies • Immune system disorders Individuals with all four major characteristics or three major and three minor characteristics are highly likely to have CHARGE syndrome [1]. CHARGE syndrome -

CHARGE Factsheet 3 Clinical Diagnosis and Features
The Information Pack CHARGE for Practitioners Factsheet 3 CHARGE syndrome: major and minor medical diagnostic criteria plus later onset features DR JEREMY KIRK, MD, FRCP, FRCPCH, Consultant Paediatric Endocrinologist, Birmingham Children’s Hospital Original diagnostic criteria The initial association of coloboma and choanal atresia with other congenital abnormalities was first described by Hall and separately Hittner et al. in 1979 (Hall, 1979; Hittner et al., 1979). In 1981 there was further description and expansion of the condition (Pagon et al., 1981). It was at this stage that the acronym CHARGE (C–coloboma, H–heart disease, A–atresia choanae, R–retarded growth and retarded development and/or CNS anomalies, G–genital hypoplasia, and E–ear anomalies and/or deafness) was made. In order to make the diagnosis of CHARGE syndrome, historically four out of six of the features of the acronym needed to be fulfilled, although one should be either choanal atresia or a coloboma (Pagon et al., 1981). From association to syndrome been several attempts to refine the diagnostic criteria, Initially CHARGE was described as an association; namely by Blake et al. (1998) and Verloes (2005). Both a nonrandom collection of birth defects, rather than of these use major features which are very specific for a syndrome, which is a more recognisable pattern of CHARGE syndrome, along with other minor features. birth defects (often with a known genetic cause). With the identification of the gene CHD7 in 2004 (Vissers The criteria suggested by Blake et al. consist of four et al., 2004) it has now been renamed a syndrome, major ‘C’s: as CHD7 is mutated in at least 60% of patients with 1.