Neurofibromatosis Type 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Segmental Overvekst Og Vaskulærmalformasjoner V02
2/1/2021 Segmental overvekst og vaskulærmalformasjoner v02 Avdeling for medisinsk genetikk Segmental overvekst og vaskulærmalformasjoner Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* ACVRL1 175 NM_000020.3 2-10 Telangiectasia, hereditary hemorrhagic, type 2 OMIM ADAMTS3 219 NM_014243.3 1-22 Hennekam lymphangiectasia- lymphedema syndrome 3 OMIM AKT1 391 NM_005163.2 2-14 Cowden syndrome 6 OMIM Proteus syndrome, somatic OMIM AKT2 392 NM_001626.6 2-14 Diabetes mellitus, type II OMIM Hypoinsulinemic hypoglycemia with hemihypertrophy OMIM AKT3 393 NM_005465.7 2-14 Megalencephaly-polymicrogyria- polydactyly-hydrocephalus syndrome 2 OMIM file:///data/SegOv_v02-web.html 1/7 2/1/2021 Segmental overvekst og vaskulærmalformasjoner v02 Ekson Gen Gen affisert (HGNC (HGNC -

Phenotypic and Genotypic Characterisation of Noonan-Like
1of5 ELECTRONIC LETTER J Med Genet: first published as 10.1136/jmg.2004.024091 on 2 February 2005. Downloaded from Phenotypic and genotypic characterisation of Noonan-like/ multiple giant cell lesion syndrome J S Lee, M Tartaglia, B D Gelb, K Fridrich, S Sachs, C A Stratakis, M Muenke, P G Robey, M T Collins, A Slavotinek ............................................................................................................................... J Med Genet 2005;42:e11 (http://www.jmedgenet.com/cgi/content/full/42/2/e11). doi: 10.1136/jmg.2004.024091 oonan-like/multiple giant cell lesion syndrome (NL/ MGCLS; OMIM 163955) is a rare condition1–3 with Key points Nphenotypic overlap with Noonan’s syndrome (OMIM 163950) and cherubism (OMIM 118400) (table 1). N Noonan-like/multiple giant cell lesion syndrome (NL/ Recently, missense mutations in the PTPN11 gene on MGCLS) has clinical similarities with Noonan’s syn- chromosome 12q24.1 have been identified as the cause of drome and cherubism. It is unclear whether it is a Noonan’s syndrome in 45% of familial and sporadic cases,45 distinct entity or a variant of Noonan’s syndrome or indicating genetic heterogeneity within the syndrome. In the cherubism. 5 study by Tartaglia et al, there was a family in which three N Three unrelated patients with NL/MGCLS were char- members had features of Noonan’s syndrome; two of these acterised, two of whom were found to have mutations had incidental mandibular giant cell lesions.3 All three in the PTPN11 gene, the mutation found in 45% of members were found to have a PTPN11 mutation known to patients with Noonan’s syndrome. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

Cardiomyopathy Precision Panel Overview Indications
Cardiomyopathy Precision Panel Overview Cardiomyopathies are a group of conditions with a strong genetic background that structurally hinder the heart to pump out blood to the rest of the body due to weakness in the heart muscles. These diseases affect individuals of all ages and can lead to heart failure and sudden cardiac death. If there is a family history of cardiomyopathy it is strongly recommended to undergo genetic testing to be aware of the family risk, personal risk, and treatment options. Most types of cardiomyopathies are inherited in a dominant manner, which means that one altered copy of the gene is enough for the disease to present in an individual. The symptoms of cardiomyopathy are variable, and these diseases can present in different ways. There are 5 types of cardiomyopathies, the most common being hypertrophic cardiomyopathy: 1. Hypertrophic cardiomyopathy (HCM) 2. Dilated cardiomyopathy (DCM) 3. Restrictive cardiomyopathy (RCM) 4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) 5. Isolated Left Ventricular Non-Compaction Cardiomyopathy (LVNC). The Igenomix Cardiomyopathy Precision Panel serves as a diagnostic and tool ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes. Indications The Igenomix Cardiomyopathy Precision Panel is indicated in those cases where there is a clinical suspicion of cardiomyopathy with or without the following manifestations: - Shortness of breath - Fatigue - Arrythmia (abnormal heart rhythm) - Family history of arrhythmia - Abnormal scans - Ventricular tachycardia - Ventricular fibrillation - Chest Pain - Dizziness - Sudden cardiac death in the family 1 Clinical Utility The clinical utility of this panel is: - The genetic and molecular diagnosis for an accurate clinical diagnosis of a patient with personal or family history of cardiomyopathy, channelopathy or sudden cardiac death. -

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

Fetal Hydrops in Combination with Gonadoblastoid Testicular Dysplasia May Represent a Lethal Type of Noonan Syndrome
etics & E en m G b ry n o a l o Reischer et al., Human Genet Embryol 2016, 6:3 m g u y H Human Genetics & Embryology DOI: 10.4172/2161-0436.1000137 ISSN: 2161-0436 Research Article Open Access Fetal Hydrops in Combination with Gonadoblastoid Testicular Dysplasia May Represent a Lethal Type of Noonan Syndrome Theresa Reischer1, Maximilian Schmid1, Sukirthini Balendran1, Manuel Nistal2, Julia Vodopiutz3, Elisabeth Krampl-Bettelheim4, Niko Popitsch5, Sandra Liebmann-Reindl6 and Berthold Streubel6,7* 1Department of Obstetrics and Feto-Maternal Medicine, Medical University of Vienna, Vienna, Austria 2Department of Pathology, Hospital La Paz, Universidad Autónoma de Madrid, Spain 3Department of Pediatrics, Medical University of Vienna, Vienna, Austria 4Fetomed - Center for Fetal Medicine, Doebling Private Hospital, Vienna, Austria 5Wellcome Trust Centre for Human Genetics, University of Oxford, Oxford, UK 6Core Facility Genomics, Medical University of Vienna, Vienna, Austria 7Department of Pathology, Medical University of Vienna, Austria Abstract Objectives: Fetal gonadoblastoid testicular dysplasia is a rare finding. The combination with typical features of Noonan syndrome has never been described so far. We performed genetic testing including whole exome sequencing in two cases with fetal hydrops, congenital heart disease and gonadoblastoid testicular dysplasia. Methods: Exome sequencing was performed in the index case, where high quality DNA was isolated from fetal blood. In the second case and in five further gonadoblastoma samples, conventional Sanger sequencing was performed on DNA isolated from formalin fixed, paraffin embedded tissue. Results: Whole exome sequencing of the index case revealed a pathogenic mutation in the RIT1 gene (c.270G>A (p.Met90Ile)), leading to the diagnosis of Noonan syndrome type 8. -

An Unusual Case of Cowden Syndrome Associated With
Pistorius et al. Hereditary Cancer in Clinical Practice (2016) 14:11 DOI 10.1186/s13053-016-0051-8 CASE REPORT Open Access An unusual case of Cowden syndrome associated with ganglioneuromatous polyposis Steffen Pistorius1,6*†, Barbara Klink2,7*†, Jessica Pablik3, Andreas Rump2, Daniela Aust3,7, Marlene Garzarolli4, Evelin Schröck2,7 and Hans K. Schackert5,6,7 Abstract Background: Ganglioneuromatous polyposis (GP) is a very rare disorder which may be associated with other clinical manifestations and syndromes, such as Cowden syndrome, multiple endocrine neoplasia (MEN) type II and neurofibromatosis (NF) 1. The risk for malignant transformation of ganglioneuromas is unknown, and the combination of GP with colon cancer has been only very seldom reported. Methods and results: We report the case of a 60-year old male patient with adenocarcinoma, adenomas and lipomas of the colon and multiple gastroduodenal lesions combined with generalised lipomatosis and macrocephaly. Based on the initial endoscopic and histological findings, a (restorative) proctocolectomy was recommended but declined by the patient. Instead, a colectomy was performed. The histological examination revealed an unforeseen GP in addition to the colon cancer. Extensive molecular diagnostics allowed for the differential diagnosis of the causes of the clinical manifestations, and the clinical suspicion of Cowden syndrome could not be confirmed using Sanger Sequencing and MLPA for the analysis of PTEN. Finally, a pathogenic germline mutation in PTEN (heterozygous stop mutation in exon 2: NM_000314 (PTEN):c.138C > A; p.Tyr46*) could be detected by next-generation sequencing (NGS), confirming an unusual presentation of Cowden syndrome with GP. Conclusions: Cowden syndrome should be considered in cases of GP with extracolonic manifestation and verified by combined clinical and molecular diagnostics. -

Ashkenazi Jewish
Reproductive Genetic Carrier Screening in Canada All couples planning their families should have a three-generation family history taken, ideally in the preconception period. Attention should be paid to the red flags in Box 1 to assess risk to future offspring. A personal or family history of: congenital anomaly e.g. congenital heart defect, neural tube defect intellectual disability or developmental delay genetic syndrome e.g. neurofibromatosis, Noonan syndrome chromosomal disorder e.g. Down syndrome (trisomy 21), familial translocation muscular disorder e.g. X-linked Duchenne and Becker muscular dystrophies bleeding disorder e.g. X-linked hemophilia A or B stillbirth sudden unexplained death other major health concerns such as cardiomyopathy, neurological disease, epilepsy, hearing loss, autism, and psychiatric disorders consanguinity Box 1. Personal and family history red flags that should prompt a referral for genetic consultation, ideally when individuals are planning a family (preconception). A history of any of these red flags should prompt referral for genetic consultation. Individuals and their partners should be encouraged to make their best efforts to obtain confirmatory information such as medical records, genetic test results, even family photos. One’s ethnicity is an important piece of risk assessment as some populations are known to have a higher incidence of certain genetic conditions due to a founder effect. Founder effect confers reduced genetic diversity in a population descended from a small number of ancestors. Founder mutations refer to specific gene mutations observed at high frequency in a specific population due to the presence of that gene mutation in a single or small number of ancestors. -
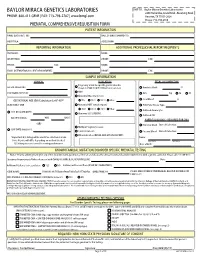
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Noonan Spectrum Disorders Panel, Sequencing ARUP Test Code 2010772 Noonan Disorders Sequencing Specimen Whole Blood
Patient Report |FINAL Client: Example Client ABC123 Patient: Patient, Example 123 Test Drive Salt Lake City, UT 84108 DOB 12/9/2011 UNITED STATES Gender: Female Patient Identifiers: 01234567890ABCD, 012345 Physician: Doctor, Example Visit Number (FIN): 01234567890ABCD Collection Date: 01/01/2017 12:34 Noonan Spectrum Disorders Panel, Sequencing ARUP test code 2010772 Noonan Disorders Sequencing Specimen Whole Blood Noonan Disorders Sequencing Interp Positive INDICATION FOR TESTING Short stature and facial features suggestive of Noonan syndrome. RESULT One pathogenic variant was detected in the PTPN11 gene. PATHOGENIC VARIANT Gene: PTPN11 (NM_002834.3) Nucleic Acid Change: c.188A>G; Heterozygous Amino Acid Alteration: p.Tyr63Cys Inheritance: Autosomal Dominant INTERPRETATION One pathogenic variant, c.188A>G; p.Tyr63Cys, was detected in the PTPN11 gene by massively parallel sequencing and confirmed by Sanger sequencing. Pathogenic PTPN11 variants are inherited in an autosomal dominant manner, and are associated with Noonan syndrome 1 (MIM: 163950), metachondromatosis (MIM: 156250), and LEOPARD syndrome 1 (MIM: 151100). No additional pathogenic variants were identified in the other targeted genes by massively parallel sequencing. Please refer to the background information included in this report for a list of the genes analyzed and limitations of this test. Evidence for variant classification: The PTPN11 c.188A>G, p.Tyr63Cys variant (rs121918459) has been reported in multiple patients diagnosed with Noonan syndrome (Tartaglia 2001, Jongmans 2011, Martinelli 2012, Hashida 2013, Lepri 2014, Okamoto 2015). This variant is located in a structurally important region of the catalytic N-terminal SH2 domain of PTPN11 (Hof 1998), and several additional variants in neighboring codons have also been identified in Noonan patients (Jongmans 2011, Tartaglia 2002, Tartaglia 2006). -

Syndrome of the Month Aarskog Syndrome
J Med Genet: first published as 10.1136/jmg.28.1.44 on 1 January 1991. Downloaded from 444 Med Genet 1991; 28: 44-47 Syndrome of the month Edited by D Donnai and R Winter Aarskog syndrome Mary E M Porteous, David R Goudie Aarskog syndrome (facio-digital-genital syndrome) Clinical features in Aarskog syndrome. was first described in 1970 by Dagfm Aarskog' who Glasgow Published presented seven males from one family with a growth Clinical features series cases disorder and associated anomalies. A year later Scott2 Hypertelorism 16/17 73/83 reported three brothers with similar features and since Ptosis 8/17 33/64 Downward slanting palpebral then there have been over 100 cases published.3A20 We fissures 10/17 33/64 are aware of 12 subjects with Aarskog syndrome living Short nose 12/17 30/45 in the west of Scotland (population 1-6 million). Wide philtrum 12/17 76/87 Maxillary hypoplasia 12/17 72/87 However, owingtothe benignnatureofthecondition, it Anteverted nares 14/17 28/36 is underdiagnosed and the true incidence must be Abnormal auricles 9/17 76/86 Broad nasal bridge 17/17 33/58 higher than this. Crease below lower lip 8/17 72/82 Widow's peak 8/17 44/51 Short/broad hands 14/17 49/60 Brachydactyly 13/17 50/60 Inheritance Syndactyly 9/17 36/56 Aarskog syndrome has been assigned to the X Clinodactyly 15/17 42/65 Short 5th finger 15/17 22/28 http://jmg.bmj.com/ chromosome on the basis of pedigree analysis but this Joint laxity 10/17 36/47 interpretation remains open to doubt. -

Cutaneous Markers of Systemic Disease and a Window to New Aspects of Tumorigenesis
JMG Online First, published on June 15, 2005 as 10.1136/jmg.2003.017806 J Med Genet: first published as 10.1136/jmg.2003.017806 on 15 June 2005. Downloaded from The lentiginoses: Cutaneous markers of systemic disease and a window to new aspects of tumorigenesis Andrew J. Bauer (1, 2) and Constantine A. Stratakis (1) @ From the 1. Section on Endocrinology & Genetics (SEGEN), Developmental Endocrinology Branch (DEB), National Institute of Child Health and Human Development (NICHD), National Institutes of Health, Bethesda, MD 20892-1103, and 2. Walter Reed Army Medical Center, Department of Pediatrics, Washington, DC, 20307 http://jmg.bmj.com/ Short title: Familial lentiginoses Key Words: Carney complex, Peutz-Jeghers syndrome, L.E.O.P.A.R.D. syndrome, Noonan syndrome, on September 30, 2021 by guest. Protected copyright. Cowden disease @ Address all correspondence and reprint requests to: Dr. Constantine A. Stratakis, Section on Endocrinology & Genetics, DEB, NICHD, NIH, Building 10, CRC, Room I-3330, 10 Center Dr., MSC 1103, Bethesda, Maryland 20892, Tel: 301-4964686, Fax: 301-4020574, E-mail: [email protected]; the corresponding author has the right to grant on behalf of all authors and does grant on behalf of all authors, a non-exclusive licence (because both Drs Stratakis and Bauer are U.S. government employees) on a worldwide basis to the BMJ Publishing Group Ltd to permit this article to be published in JMG/ptMJPGL products and sublicences such use and exploit all subsidiary rights, as set out in the Journal’s site http://JMG.bmjjournals.com/misc/ifora/licenceform.shtml. Copyright Article author (or their employer) 2005.