Staphylococcus Aureus Toxins and Their Molecular Activity in Infectious Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections
toxins Review The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections Patience Shumba 1, Srikanth Mairpady Shambat 2 and Nikolai Siemens 1,* 1 Center for Functional Genomics of Microbes, Department of Molecular Genetics and Infection Biology, University of Greifswald, D-17489 Greifswald, Germany; [email protected] 2 Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, University of Zurich, CH-8091 Zurich, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +49-3834-420-5711 Received: 20 May 2019; Accepted: 10 June 2019; Published: 11 June 2019 Abstract: Necrotizing soft tissue infections (NSTIs) are critical clinical conditions characterized by extensive necrosis of any layer of the soft tissue and systemic toxicity. Group A streptococci (GAS) and Staphylococcus aureus are two major pathogens associated with monomicrobial NSTIs. In the tissue environment, both Gram-positive bacteria secrete a variety of molecules, including pore-forming exotoxins, superantigens, and proteases with cytolytic and immunomodulatory functions. The present review summarizes the current knowledge about streptococcal and staphylococcal toxins in NSTIs with a special focus on their contribution to disease progression, tissue pathology, and immune evasion strategies. Keywords: Streptococcus pyogenes; group A streptococcus; Staphylococcus aureus; skin infections; necrotizing soft tissue infections; pore-forming toxins; superantigens; immunomodulatory proteases; immune responses Key Contribution: Group A streptococcal and Staphylococcus aureus toxins manipulate host physiological and immunological responses to promote disease severity and progression. 1. Introduction Necrotizing soft tissue infections (NSTIs) are rare and represent a more severe rapidly progressing form of soft tissue infections that account for significant morbidity and mortality [1]. -

Drug-Resistant Streptococcus Pneumoniae and Methicillin
NEWS & NOTES Conference Summary pneumoniae can vary among popula- conference sessions was that statically tions and is influenced by local pre- sound methods of data collection that Drug-resistant scribing practices and the prevalence capture valid, meaningful, and useful of resistant clones. Conference pre- data and meet the financial restric- Streptococcus senters discussed the role of surveil- tions of state budgets are indicated. pneumoniae and lance in raising awareness of the Active, population-based surveil- Methicillin- resistance problem and in monitoring lance for collecting relevant isolates is the effectiveness of prevention and considered the standard criterion. resistant control programs. National- and state- Unfortunately, this type of surveil- Staphylococcus level epidemiologists discussed the lance is labor-intensive and costly, aureus benefits of including state-level sur- making it an impractical choice for 1 veillance data with appropriate antibi- many states. The challenges of isolate Surveillance otic use programs designed to address collection, packaging and transport, The Centers for Disease Control the antibiotic prescribing practices of data collection, and analysis may and Prevention (CDC) convened a clinicians. The potential for local sur- place an unacceptable workload on conference on March 12–13, 2003, in veillance to provide information on laboratory and epidemiology person- Atlanta, Georgia, to discuss improv- the impact of a new pneumococcal nel. ing state-based surveillance of drug- vaccine for children was also exam- Epidemiologists from several state resistant Streptococcus pneumoniae ined; the vaccine has been shown to health departments that have elected (DRSP) and methicillin-resistant reduce infections caused by resistance to implement enhanced antimicrobial Staphylococcus aureus (MRSA). -

Biological Toxins As the Potential Tools for Bioterrorism
International Journal of Molecular Sciences Review Biological Toxins as the Potential Tools for Bioterrorism Edyta Janik 1, Michal Ceremuga 2, Joanna Saluk-Bijak 1 and Michal Bijak 1,* 1 Department of General Biochemistry, Faculty of Biology and Environmental Protection, University of Lodz, Pomorska 141/143, 90-236 Lodz, Poland; [email protected] (E.J.); [email protected] (J.S.-B.) 2 CBRN Reconnaissance and Decontamination Department, Military Institute of Chemistry and Radiometry, Antoniego Chrusciela “Montera” 105, 00-910 Warsaw, Poland; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +48-(0)426354336 Received: 3 February 2019; Accepted: 3 March 2019; Published: 8 March 2019 Abstract: Biological toxins are a heterogeneous group produced by living organisms. One dictionary defines them as “Chemicals produced by living organisms that have toxic properties for another organism”. Toxins are very attractive to terrorists for use in acts of bioterrorism. The first reason is that many biological toxins can be obtained very easily. Simple bacterial culturing systems and extraction equipment dedicated to plant toxins are cheap and easily available, and can even be constructed at home. Many toxins affect the nervous systems of mammals by interfering with the transmission of nerve impulses, which gives them their high potential in bioterrorist attacks. Others are responsible for blockage of main cellular metabolism, causing cellular death. Moreover, most toxins act very quickly and are lethal in low doses (LD50 < 25 mg/kg), which are very often lower than chemical warfare agents. For these reasons we decided to prepare this review paper which main aim is to present the high potential of biological toxins as factors of bioterrorism describing the general characteristics, mechanisms of action and treatment of most potent biological toxins. -

Medical Management of Biologic Casualties Handbook
USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Fourth Edition February 2001 U.S. ARMY MEDICAL RESEARCH INSTITUTE OF INFECTIOUS DISEASES ¨ FORT DETRICK FREDERICK, MARYLAND 1 Sources of information: National Response Center 1-800-424-8802 or (for chem/bio hazards & terrorist events) 1-202-267-2675 National Domestic Preparedness Office: 1-202-324-9025 (for civilian use) Domestic Preparedness Chem/Bio Help line: 1-410-436-4484 or (Edgewood Ops Center - for military use) DSN 584-4484 USAMRIID Emergency Response Line: 1-888-872-7443 CDC'S Bioterrorism Preparedness and Response Center: 1-770-488-7100 John's Hopkins Center for Civilian Biodefense: 1-410-223-1667 (Civilian Biodefense Studies) An Adobe Acrobat Reader (pdf file) version and a Palm OS Electronic version of this Handbook can both be downloaded from the Internet at: http://www.usamriid.army.mil/education/bluebook.html 2 USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Fourth Edition February 2001 Editors: LTC Mark Kortepeter LTC George Christopher COL Ted Cieslak CDR Randall Culpepper CDR Robert Darling MAJ Julie Pavlin LTC John Rowe COL Kelly McKee, Jr. COL Edward Eitzen, Jr. Comments and suggestions are appreciated and should be addressed to: Operational Medicine Department Attn: MCMR-UIM-O U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) Fort Detrick, Maryland 21702-5011 3 PREFACE TO THE FOURTH EDITION The Medical Management of Biological Casualties Handbook, which has become affectionately known as the "Blue Book," has been enormously successful - far beyond our expectations. Since the first edition in 1993, the awareness of biological weapons in the United States has increased dramatically. -
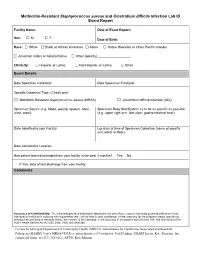
Methicillin-Resistant Staphylococcus Aureus and Clostridium Difficile Infection Lab ID Event Report
Methicillin-Resistant Staphylococcus aureus and Clostridium difficile Infection Lab ID Event Report Facility Name: Date of Event Report: Sex: M F □ □ Date of Birth: Race: □ White □ Black or African American □ Asian □ Native Hawaiian or Other Pacific Islander □ American Indian or Alaska Native □ Other [specify] __________________ Ethnicity: □ Hispanic or Latino □ Not Hispanic or Latino □ Other Event Details Date Specimen Collected: Date Specimen Finalized: Specific Organism Type: (Check one) □ Methicillin-Resistant Staphylococcus aureus (MRSA) □ Clostridium difficile Infection (CDI) Specimen Source (e.g. blood, wound, sputum, bone, Specimen Body Site/System try to be as specific as possible urine, stool): (e.g. upper right arm, foot ulcer, gastrointestinal tract): Date Admitted to your Facility: Location at time of Specimen Collection (name of specific unit, ward, or floor): Date Admitted to Location: Has patient been discharged from your facility in the past 3 months? Yes No If Yes, date of last discharge from your facility: Comments Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)). For use by Michigan Department of Community Health (MDCH), Surveillance for Healthcare-Associated and Resistant Pathogens (SHARP) Unit’s MRSA/CDI Prevention Initiative (Coordinator: Gail Denkins, SHARP Intern: Kate Manton); fax completed forms to (517) 335-8263, ATTN: Kate Manton. -

SARS-Cov-2 As a Superantigen in Multisystem Inflammatory Syndrome in Children (MIS-C)
SARS-CoV-2 as a superantigen in multisystem inflammatory syndrome in children (MIS-C) Theodore Kouo, Worarat Chaisawangwong J Clin Invest. 2021. https://doi.org/10.1172/JCI149327. Commentary In-Press Preview Multisystem Inflammatory Syndrome in Children (MIS-C) is a rare but deadly new disease in children that rapidly progresses to hyperinflammation, shock, and can lead to multiple organ failure if unrecognized. It has been found to be temporally associated with the COVID-19 pandemic and is often associated with SARS-CoV-2 exposure in children. In this issue of the JCI, Porritt, Paschold, and Rivas et al. identify restricted T cell receptor (TCR) β-chain variable domain (Vβ) usage in patients with severe MIS-C indicating a potential role for SARS-CoV-2 as a superantigen. These findings suggest that a blood test that determines the presence of specific TCR beta variable gene segments (TRBV) may identify patients at risk for severe MIS-C. Find the latest version: https://jci.me/149327/pdf SARS-CoV-2 as a superantigen in multisystem inflammatory syndrome in children (MIS-C) Theodore Kouo1 and Worarat Chaisawangwong2 1Department of Pediatrics, Division of Emergency Medicine, 2Department of Pathology, Johns Hopkins University, School of Medicine, Baltimore, MD, USA. Address correspondence to: Theodore Kouo Johns Hopkins Children’s Center 1800 Orleans Street, G1509 Phone: 410-955-6146 Email: [email protected] COI Statement: The authors declare that no conflict of interest exists. Abstract Multisystem Inflammatory Syndrome in Children (MIS-C) is a rare but deadly new disease in children that rapidly progresses to hyperinflammation, shock, and can lead to multiple organ failure if unrecognized. -
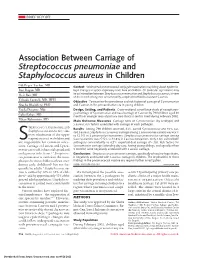
Association Between Carriage of Streptococcus Pneumoniae and Staphylococcus Aureus in Children
BRIEF REPORT Association Between Carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children Gili Regev-Yochay, MD Context Widespread pneumococcal conjugate vaccination may bring about epidemio- Ron Dagan, MD logic changes in upper respiratory tract flora of children. Of particular significance may Meir Raz, MD be an interaction between Streptococcus pneumoniae and Staphylococcus aureus, in view of the recent emergence of community-acquired methicillin-resistant S aureus. Yehuda Carmeli, MD, MPH Objective To examine the prevalence and risk factors of carriage of S pneumoniae Bracha Shainberg, PhD and S aureus in the prevaccination era in young children. Estela Derazne, MSc Design, Setting, and Patients Cross-sectional surveillance study of nasopharyn- geal carriage of S pneumoniae and nasal carriage of S aureus by 790 children aged 40 Galia Rahav, MD months or younger seen at primary care clinics in central Israel during February 2002. Ethan Rubinstein, MD Main Outcome Measures Carriage rates of S pneumoniae (by serotype) and S aureus; risk factors associated with carriage of each pathogen. TREPTOCOCCUS PNEUMONIAE AND Results Among 790 children screened, 43% carried S pneumoniae and 10% car- Staphylococcus aureus are com- ried S aureus. Staphylococcus aureus carriage among S pneumoniae carriers was 6.5% mon inhabitants of the upper vs 12.9% in S pneumoniae noncarriers. Streptococcus pneumoniae carriage among respiratory tract in children and S aureus carriers was 27.5% vs 44.8% in S aureus noncarriers. Only 2.8% carried both Sare responsible for common infec- pathogens concomitantly vs 4.3% expected dual carriage (P=.03). Risk factors for tions. Carriage of S aureus and S pneu- S pneumoniae carriage (attending day care, having young siblings, and age older than moniae can result in bacterial spread and 3 months) were negatively associated with S aureus carriage. -
Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Clostridium difficile infection: How to deal with the problem DH INFORMATION RE ADER B OX Policy Estates HR / Workforce Commissioning Management IM & T Planning / Finance Clinical Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 9833 Title Clostridium difficile infection: How to deal with the problem Author DH and HPA Publication Date December 2008 Target Audience PCT CEs, NHS Trust CEs, SHA CEs, Care Trust CEs, Medical Directors, Directors of PH, Directors of Nursing, PCT PEC Chairs, NHS Trust Board Chairs, Special HA CEs, Directors of Infection Prevention and Control, Infection Control Teams, Health Protection Units, Chief Pharmacists Circulation List Description This guidance outlines newer evidence and approaches to delivering good infection control and environmental hygiene. It updates the 1994 guidance and takes into account a national framework for clinical governance which did not exist in 1994. Cross Ref N/A Superseded Docs Clostridium difficile Infection Prevention and Management (1994) Action Required CEs to consider with DIPCs and other colleagues Timing N/A Contact Details Healthcare Associated Infection and Antimicrobial Resistance Department of Health Room 528, Wellington House 133-155 Waterloo Road London SE1 8UG For Recipient's Use Front cover image: Clostridium difficile attached to intestinal cells. Reproduced courtesy of Dr Jan Hobot, Cardiff University School of Medicine. Clostridium difficile infection: How to deal with the problem Contents Foreword 1 Scope and purpose 2 Introduction 3 Why did CDI increase? 4 Approach to compiling the guidance 6 What is new in this guidance? 7 Core Guidance Key recommendations 9 Grading of recommendations 11 Summary of healthcare recommendations 12 1. -

Medical Management of Biological Casualties Handbook
USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 U.S. ARMY MEDICAL RESEARCH INSTITUTE OF INFECTIOUS DISEASES FORT DETRICK FREDERICK, MARYLAND Emergency Response Numbers National Response Center: 1-800-424-8802 or (for chem/bio hazards & terrorist events) 1-202-267-2675 National Domestic Preparedness Office: 1-202-324-9025 (for civilian use) Domestic Preparedness Chem/Bio Helpline: 1-410-436-4484 or (Edgewood Ops Center – for military use) DSN 584-4484 USAMRIID’s Emergency Response Line: 1-888-872-7443 CDC'S Emergency Response Line: 1-770-488-7100 Handbook Download Site An Adobe Acrobat Reader (pdf file) version of this handbook can be downloaded from the internet at the following url: http://www.usamriid.army.mil USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 Lead Editor Lt Col Jon B. Woods, MC, USAF Contributing Editors CAPT Robert G. Darling, MC, USN LTC Zygmunt F. Dembek, MS, USAR Lt Col Bridget K. Carr, MSC, USAF COL Ted J. Cieslak, MC, USA LCDR James V. Lawler, MC, USN MAJ Anthony C. Littrell, MC, USA LTC Mark G. Kortepeter, MC, USA LTC Nelson W. Rebert, MS, USA LTC Scott A. Stanek, MC, USA COL James W. Martin, MC, USA Comments and suggestions are appreciated and should be addressed to: Operational Medicine Department Attn: MCMR-UIM-O U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) Fort Detrick, Maryland 21702-5011 PREFACE TO THE SIXTH EDITION The Medical Management of Biological Casualties Handbook, which has become affectionately known as the "Blue Book," has been enormously successful - far beyond our expectations. -

Free PDF Download
European Review for Medical and Pharmacological Sciences 2021; 25: 1622-1630 Superantigens, superantigen-like proteins and superantigen derivatives for cancer treatment J.-Y. CHEN Xiehe Biology Group, Nobel Institute of Medicine, Shenzhen, Guangdong Province, China Abstract. – OBJECTIVE: Bacterial superanti- gesting a more complex mechanism of immune gens (SAgs) are proteins produced by few types response6. Indeed, the current view is that SAgs of bacteria that have been linked to several hu- bind to multiple coreceptors forming a costimu- man diseases. Due to their potent in vitro and in latory axis between coreceptors critical for T-cell vivo tumoricidal effects, they are extensively in- 7 vestigated for oncological applications either activation . CD28 is a homodimer expressed alone or in combination with classical antican- constitutively on T cells that interacts with its cer drugs. However, the intrinsic toxicity of nat- B7 coligands expressed on antigen-presenting ural SAgs stimulated the development of more cells, transducing the signal essential for T cell effective and less toxic SAg-based immunother- activation. The staphylococcal superantigen-like apy. This review summarizes our current knowl- protein 1 (SSL1) specifically binds to human edge on SAg-based immunotherapy including extracellular signal-regulated kinase 2 (hERK2), SAg-like proteins and SAg derivatives, as well as their potential alone or with other therapeu- an important stress-activated kinase in mito- 8 tic modalities including chemotherapy and ra- gen-activated protein kinase signaling pathways . diotherapy. It is now clearer that SAgs induce the release of cytokines and chemokines through multiple Key Words: pathways as it was recently observed in in vitro Superantigen, Superantigen derivative, Superanti- 9 gen-like, Cancer, Combination therapy experiments . -

Penetration of Stratified Mucosa Cytolysins Augment Superantigen
Cytolysins Augment Superantigen Penetration of Stratified Mucosa Amanda J. Brosnahan, Mary J. Mantz, Christopher A. Squier, Marnie L. Peterson and Patrick M. Schlievert This information is current as of September 25, 2021. J Immunol 2009; 182:2364-2373; ; doi: 10.4049/jimmunol.0803283 http://www.jimmunol.org/content/182/4/2364 Downloaded from References This article cites 76 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/182/4/2364.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 25, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2009 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Cytolysins Augment Superantigen Penetration of Stratified Mucosa1 Amanda J. Brosnahan,* Mary J. Mantz,† Christopher A. Squier,† Marnie L. Peterson,‡ and Patrick M. Schlievert2* Staphylococcus aureus and Streptococcus pyogenes colonize mucosal surfaces of the human body to cause disease. A group of virulence factors known as superantigens are produced by both of these organisms that allows them to cause serious diseases from the vaginal (staphylococci) or oral mucosa (streptococci) of the body. -

Nasopharyngeal Infection by Streptococcus Pyogenes Requires Superantigen-Responsive Vβ-Specific T Cells
Nasopharyngeal infection by Streptococcus pyogenes requires superantigen-responsive Vβ-specific T cells Joseph J. Zeppaa, Katherine J. Kaspera, Ivor Mohorovica, Delfina M. Mazzucaa, S. M. Mansour Haeryfara,b,c,d, and John K. McCormicka,c,d,1 aDepartment of Microbiology and Immunology, Schulich School of Medicine & Dentistry, Western University, London, ON N6A 5C1, Canada; bDepartment of Medicine, Division of Clinical Immunology & Allergy, Schulich School of Medicine & Dentistry, Western University, London, ON N6A 5A5, Canada; cCentre for Human Immunology, Western University, London, ON N6A 5C1, Canada; and dLawson Health Research Institute, London, ON N6C 2R5, Canada Edited by Philippa Marrack, Howard Hughes Medical Institute, National Jewish Health, Denver, CO, and approved July 14, 2017 (received for review January 18, 2017) The globally prominent pathogen Streptococcus pyogenes secretes context of invasive streptococcal disease is extremely dangerous, potent immunomodulatory proteins known as superantigens with a mortality rate of over 30% (10). (SAgs), which engage lateral surfaces of major histocompatibility The role of SAgs in severe human infections has been well class II molecules and T-cell receptor (TCR) β-chain variable domains established (5, 11, 12), and specific MHC-II haplotypes are known (Vβs). These interactions result in the activation of numerous Vβ- risk factors for the development of invasive streptococcal disease specific T cells, which is the defining activity of a SAg. Although (13), an outcome that has been directly linked to SAgs (14, 15). streptococcal SAgs are known virulence factors in scarlet fever However, how these exotoxins contribute to superficial disease and and toxic shock syndrome, mechanisms by how SAgs contribute colonization is less clear.