Medical Management of Biologic Casualties Handbook
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Unapproved Products, Off-Label Use, and Black-Box Warning
Use of Unapproved Products, Off-Label Use, and Black-Box Warning ... A Variation of Newton’s Third Law or the Practical Application of the Rule of Unin- tended Consequences … Considerations in Military Operational Medicine Jerome F. Pierson, RPh, PhD Executive Editors Note: As multiple medical research and development efforts (both in SOF and in conventional research units) offer new drugs and medical equipment to the battlefield, we need to understand the rules of engagement for use, which, are dif- ferent for individual providers versus military heath care systems. ABSTRACT This article discusses the regulatory requirements for the use of unapproved drugs and off-label use of drugs and provides specific examples for military medicine. Additionally, it explains issues associated with standardization by the Service as a designated set, kit, or outfit as opposed to a general guidance. The former situation can be interpreted as a de facto policy whereas the latter is an adaptation of practice of medicine. Recent news stories brought to light the challenges assaulted from many sides to include consumer groups who facing military medicine in an environment where dramatic at times advocate for greater safety and at other times de- life-saving measures have become the expected rather then mand quicker access to therapeutic breakthroughs as well the exception.1,2 However, many of these same life-saving as the pharmaceutical industry which faces demands from measures have the potential to place a practitioner in situa- stockholders for return on investment. Reliance upon re- tions of “damned if you do, damned if you don’t” with re- sults from controlled clinical trials is problematic in that it gard to adherence to various regulatory and legal hurdles. -

The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections
toxins Review The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections Patience Shumba 1, Srikanth Mairpady Shambat 2 and Nikolai Siemens 1,* 1 Center for Functional Genomics of Microbes, Department of Molecular Genetics and Infection Biology, University of Greifswald, D-17489 Greifswald, Germany; [email protected] 2 Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, University of Zurich, CH-8091 Zurich, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +49-3834-420-5711 Received: 20 May 2019; Accepted: 10 June 2019; Published: 11 June 2019 Abstract: Necrotizing soft tissue infections (NSTIs) are critical clinical conditions characterized by extensive necrosis of any layer of the soft tissue and systemic toxicity. Group A streptococci (GAS) and Staphylococcus aureus are two major pathogens associated with monomicrobial NSTIs. In the tissue environment, both Gram-positive bacteria secrete a variety of molecules, including pore-forming exotoxins, superantigens, and proteases with cytolytic and immunomodulatory functions. The present review summarizes the current knowledge about streptococcal and staphylococcal toxins in NSTIs with a special focus on their contribution to disease progression, tissue pathology, and immune evasion strategies. Keywords: Streptococcus pyogenes; group A streptococcus; Staphylococcus aureus; skin infections; necrotizing soft tissue infections; pore-forming toxins; superantigens; immunomodulatory proteases; immune responses Key Contribution: Group A streptococcal and Staphylococcus aureus toxins manipulate host physiological and immunological responses to promote disease severity and progression. 1. Introduction Necrotizing soft tissue infections (NSTIs) are rare and represent a more severe rapidly progressing form of soft tissue infections that account for significant morbidity and mortality [1]. -

Biological Toxins As the Potential Tools for Bioterrorism
International Journal of Molecular Sciences Review Biological Toxins as the Potential Tools for Bioterrorism Edyta Janik 1, Michal Ceremuga 2, Joanna Saluk-Bijak 1 and Michal Bijak 1,* 1 Department of General Biochemistry, Faculty of Biology and Environmental Protection, University of Lodz, Pomorska 141/143, 90-236 Lodz, Poland; [email protected] (E.J.); [email protected] (J.S.-B.) 2 CBRN Reconnaissance and Decontamination Department, Military Institute of Chemistry and Radiometry, Antoniego Chrusciela “Montera” 105, 00-910 Warsaw, Poland; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +48-(0)426354336 Received: 3 February 2019; Accepted: 3 March 2019; Published: 8 March 2019 Abstract: Biological toxins are a heterogeneous group produced by living organisms. One dictionary defines them as “Chemicals produced by living organisms that have toxic properties for another organism”. Toxins are very attractive to terrorists for use in acts of bioterrorism. The first reason is that many biological toxins can be obtained very easily. Simple bacterial culturing systems and extraction equipment dedicated to plant toxins are cheap and easily available, and can even be constructed at home. Many toxins affect the nervous systems of mammals by interfering with the transmission of nerve impulses, which gives them their high potential in bioterrorist attacks. Others are responsible for blockage of main cellular metabolism, causing cellular death. Moreover, most toxins act very quickly and are lethal in low doses (LD50 < 25 mg/kg), which are very often lower than chemical warfare agents. For these reasons we decided to prepare this review paper which main aim is to present the high potential of biological toxins as factors of bioterrorism describing the general characteristics, mechanisms of action and treatment of most potent biological toxins. -

Frequencies Between Serial Killer Typology And
FREQUENCIES BETWEEN SERIAL KILLER TYPOLOGY AND THEORIZED ETIOLOGICAL FACTORS A dissertation presented to the faculty of ANTIOCH UNIVERSITY SANTA BARBARA in partial fulfillment of the requirements for the degree of DOCTOR OF PSYCHOLOGY in CLINICAL PSYCHOLOGY By Leryn Rose-Doggett Messori March 2016 FREQUENCIES BETWEEN SERIAL KILLER TYPOLOGY AND THEORIZED ETIOLOGICAL FACTORS This dissertation, by Leryn Rose-Doggett Messori, has been approved by the committee members signed below who recommend that it be accepted by the faculty of Antioch University Santa Barbara in partial fulfillment of requirements for the degree of DOCTOR OF PSYCHOLOGY Dissertation Committee: _______________________________ Ron Pilato, Psy.D. Chairperson _______________________________ Brett Kia-Keating, Ed.D. Second Faculty _______________________________ Maxann Shwartz, Ph.D. External Expert ii © Copyright by Leryn Rose-Doggett Messori, 2016 All Rights Reserved iii ABSTRACT FREQUENCIES BETWEEN SERIAL KILLER TYPOLOGY AND THEORIZED ETIOLOGICAL FACTORS LERYN ROSE-DOGGETT MESSORI Antioch University Santa Barbara Santa Barbara, CA This study examined the association between serial killer typologies and previously proposed etiological factors within serial killer case histories. Stratified sampling based on race and gender was used to identify thirty-six serial killers for this study. The percentage of serial killers within each race and gender category included in the study was taken from current serial killer demographic statistics between 1950 and 2010. Detailed data -

Free Executive Summary
Giving Full Measure to Countermeasures: Addressing Problems in the DoD Program to Develop Medical Countermeasures Against Biological Warfare Agents http://www.nap.edu/catalog/10908.html Committee on Accelerating the Research, Development, and Acquisition of Medical Countermeasures Against Biological Warfare Agents Medical Follow-up Agency and Board on Life Sciences Lois M. Joellenbeck, Jane S. Durch, and Leslie Z. Benet, Editors Copyright © National Academy of Sciences. All rights reserved. Giving Full Measure to Countermeasures: Addressing Problems in the DoD Program to Develop Medical Countermeasures Against Biological Warfare Agents http://www.nap.edu/catalog/10908.html THE NATIONAL ACADEMIES PRESS 500 Fifth Street, N.W. Washington, DC 20001 NOTICE: The project that is the subject of this report was approved by the Governing Board of the National Research Council, whose members are drawn from the councils of the Na- tional Academy of Sciences, the National Academy of Engineering, and the Institute of Medi- cine. The members of the committee responsible for the report were chosen for their special competences and with regard for appropriate balance. Support for this project was provided by Contract No. DAMD17-02-C-0099 between the National Academy of Sciences and the U.S. Army. The views presented in this report are those of the Institute of Medicine and National Research Council Committee on Accelerat- ing the Research, Development, and Acquisition of Medical Countermeasures Against Bio- logical Warfare Agents and are not necessarily those of the funding agencies. Library of Congress Cataloging-in-Publication Data Giving full measure to countermeasures : addressing problems in the DOD program to de- velop medical countermeasures against biological warfare agents / Committee on Acceler- ating the Research, Development, and Acquisition of Medical Countermeasures against Bio- logical Warfare Agents, Medical Follow-up Agency and Board on Life Sciences ; Lois M. -

The President
3 1999 Compilation and Parts 100±102 Revised as of January 1, 2000 The President Published by: Office of the Federal Register National Archives and Records Administration A Special Edition of the Federal Register VerDate 11-MAY-2000 08:53 Aug 11, 2000 Jkt 190004 PO 00000 Frm 00001 Fmt 8091 Sfmt 8091 Y:\SGML\190004F.XXX pfrm07 PsN: 190004F U.S. GOVERNMENT PRINTING OFFICE WASHINGTON: 2000 For sale by U.S. Government Printing Office Superintendent of Documents, Mail Stop: SSOP, Washington, DC 20402±9328 ii VerDate 11-MAY-2000 08:53 Aug 11, 2000 Jkt 190004 PO 00000 Frm 00002 Fmt 8092 Sfmt 8092 Y:\SGML\190004F.XXX pfrm07 PsN: 190004F Table of Contents Page List of Title 3 Compilations ....................................................................... iv Explanation of the Code of Federal Regulations ........................................... v Explanation of This Title ........................................................................... ix How To Cite This Title ............................................................................... xi Title 3 ......................................................................................................... xiii 1999 CompilationÐPresidential Documents .................................... 1 Chapter IÐExecutive Office of the President .................................. 325 Title 3 Finding Aids .................................................................................... 335 Tables ............................................................................................. -

SARS-Cov-2 As a Superantigen in Multisystem Inflammatory Syndrome in Children (MIS-C)
SARS-CoV-2 as a superantigen in multisystem inflammatory syndrome in children (MIS-C) Theodore Kouo, Worarat Chaisawangwong J Clin Invest. 2021. https://doi.org/10.1172/JCI149327. Commentary In-Press Preview Multisystem Inflammatory Syndrome in Children (MIS-C) is a rare but deadly new disease in children that rapidly progresses to hyperinflammation, shock, and can lead to multiple organ failure if unrecognized. It has been found to be temporally associated with the COVID-19 pandemic and is often associated with SARS-CoV-2 exposure in children. In this issue of the JCI, Porritt, Paschold, and Rivas et al. identify restricted T cell receptor (TCR) β-chain variable domain (Vβ) usage in patients with severe MIS-C indicating a potential role for SARS-CoV-2 as a superantigen. These findings suggest that a blood test that determines the presence of specific TCR beta variable gene segments (TRBV) may identify patients at risk for severe MIS-C. Find the latest version: https://jci.me/149327/pdf SARS-CoV-2 as a superantigen in multisystem inflammatory syndrome in children (MIS-C) Theodore Kouo1 and Worarat Chaisawangwong2 1Department of Pediatrics, Division of Emergency Medicine, 2Department of Pathology, Johns Hopkins University, School of Medicine, Baltimore, MD, USA. Address correspondence to: Theodore Kouo Johns Hopkins Children’s Center 1800 Orleans Street, G1509 Phone: 410-955-6146 Email: [email protected] COI Statement: The authors declare that no conflict of interest exists. Abstract Multisystem Inflammatory Syndrome in Children (MIS-C) is a rare but deadly new disease in children that rapidly progresses to hyperinflammation, shock, and can lead to multiple organ failure if unrecognized. -

JP 3-11, Operations in Chemical, Biological, Radiological, and Nuclear Environments, 04 October 2013
Joint Publication 3-11 OF NT TH E E W M I S E' L L H D T E F T E N A R D R A M P Y E D • • U A N C I I T R E E D M S A T F AT E S O Operations in Chemical, Biological, Radiological, and Nuclear Environments 29 October 2018 PREFACE 1. Scope This publication provides doctrine for planning, conducting, and assessing military operations in chemical, biological, radiological, and nuclear environments. 2. Purpose This publication has been prepared under the direction of the Chairman of the Joint Chiefs of Staff (CJCS). It sets forth joint doctrine to govern the activities and performance of the Armed Forces of the United States in joint operations, and it provides considerations for military interaction with governmental and nongovernmental agencies, multinational forces, and other interorganizational partners. It provides military guidance for the exercise of authority by combatant commanders and other joint force commanders (JFCs), and prescribes joint doctrine for operations and training. It provides military guidance for use by the Armed Forces in preparing and executing their plans and orders. It is not the intent of this publication to restrict the authority of the JFC from organizing the force and executing the mission in a manner the JFC deems most appropriate to ensure unity of effort in the accomplishment of objectives. 3. Application a. Joint doctrine established in this publication applies to the Joint Staff, commanders of combatant commands, subordinate unified commands, joint task forces, subordinate components of these commands, the Services, and combat support agencies. -

Medical Management of Biological Casualties Handbook
USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 U.S. ARMY MEDICAL RESEARCH INSTITUTE OF INFECTIOUS DISEASES FORT DETRICK FREDERICK, MARYLAND Emergency Response Numbers National Response Center: 1-800-424-8802 or (for chem/bio hazards & terrorist events) 1-202-267-2675 National Domestic Preparedness Office: 1-202-324-9025 (for civilian use) Domestic Preparedness Chem/Bio Helpline: 1-410-436-4484 or (Edgewood Ops Center – for military use) DSN 584-4484 USAMRIID’s Emergency Response Line: 1-888-872-7443 CDC'S Emergency Response Line: 1-770-488-7100 Handbook Download Site An Adobe Acrobat Reader (pdf file) version of this handbook can be downloaded from the internet at the following url: http://www.usamriid.army.mil USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 Lead Editor Lt Col Jon B. Woods, MC, USAF Contributing Editors CAPT Robert G. Darling, MC, USN LTC Zygmunt F. Dembek, MS, USAR Lt Col Bridget K. Carr, MSC, USAF COL Ted J. Cieslak, MC, USA LCDR James V. Lawler, MC, USN MAJ Anthony C. Littrell, MC, USA LTC Mark G. Kortepeter, MC, USA LTC Nelson W. Rebert, MS, USA LTC Scott A. Stanek, MC, USA COL James W. Martin, MC, USA Comments and suggestions are appreciated and should be addressed to: Operational Medicine Department Attn: MCMR-UIM-O U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) Fort Detrick, Maryland 21702-5011 PREFACE TO THE SIXTH EDITION The Medical Management of Biological Casualties Handbook, which has become affectionately known as the "Blue Book," has been enormously successful - far beyond our expectations. -

Americans and Russians Are Mostly Disinterested and Disengaged with Each Other
Americans and Russians Are Mostly Disinterested and Disengaged with Each Other Brendan Helm, Research Assistant, Public Opinion, Chicago Council on Global Affairs Arik Burakovsky, Assistant Director, Russia and Eurasia Program, The Fletcher School of Law and Diplomacy, Tufts University Lily Wojtowicz, Research Associate, Public Opinion, Chicago Council on Global Affairs August 2019 The last few years have seen a substantial deterioration in relations between the United States and Russia. The international crisis over Ukraine, Russia’s interference in the 2016 US presidential election, and US sanctions against Russia have all contributed to the growing acrimony. Recent surveys conducted by the Chicago Council on Global Affairs and the Levada Analytical Center reveal that large majorities of both Russians and Americans now view their countries as rivals. But in the midst of heightened tensions between Moscow and Washington, how do regular citizens of each country view one another? A joint project conducted by the Chicago Council on Global Affairs, the Levada Analytical Center, and The Fletcher School of Law and Diplomacy at Tufts University shows that despite the perception of rivalry between their countries, Russians’ and Americans’ views on the people of the other country are more favorable. However, the survey results also show that Russians and Americans are not particularly curious about each other, they rarely follow news about one another, and the majority of each group has never met someone from the other. Nonetheless, self-reported interests from each side in arts and sciences suggest that there are non-political paths toward warmer relations. Key Findings • 68 percent of Americans view Russians either very or fairly positively, while 48 percent of Russians have those views of Americans. -
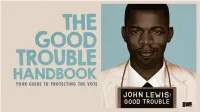
John Lewis' 'Good Trouble' Handbook
“THE RIGHT TO VOTE IS THE MOST POWERFUL NONVIOLENT TOOL WE HAVE IN A DEMOCRACY. I RISKED MY LIFE DEFENDING THAT RIGHT.” – Congressman John Lewis, John Lewis: Good Trouble Go to Map GOOD TROUBLE Congressman John Lewis’ life’s work has changed the very fabric of this country. Born in During the protest, John Lewis was hit on the head by a state trooper and suffered a the heart of the Jim Crow South, in the shadow of slavery, he saw the profound injustice fractured skull. On Bloody Sunday, Lewis risked his life for the right to vote and has since all around him and knew, from a young age, that he wanted to do something about it. By devoted his life to ensuring that every American has access to the ballot box. his late teens, he had joined the first Freedom Riders and later became the chairman of the Student Nonviolent Coordinating Committee (SNCC), one of the groups responsible Unfortunately, Congressman Lewis’ work did not end with the Civil Rights era. In 2013, for organizing the 1963 March on Washington. On August 28, 1963, on the steps of the Voting Rights Act, for which he shed his blood, was effectively gutted by a Supreme the Lincoln Memorial, John Lewis gave his own rousing speech alongside some of the Court decision, Shelby County v. Holder. In the years since, voter suppression targeting greatest leaders of the civil rights movement, including Rev. Dr. Martin Luther King Jr. communities of color has significantly increased. But it was March 7, 1965, that etched Congressman Lewis into the American psyche. -

None of the Above*
None Of The Above Gergely Ujhelyi, Somdeep Chatterjee, and Andrea Szabóy March 12, 2019 Abstract Who are “protest voters” and do they affect elections? We study this question using the introduction of a pure protest option (“None Of The Above”) on Indian ballots. To infer individual behavior from administrative data, we borrow a model from the consumer demand literature in Industrial Organization. We find that in elections without NOTA, most protest voters simply abstain. Protest voters who turn out scatter their votes among many candidates and consequently have little impact on election results. From a policy perspective, NOTA may be an effective tool to increase political participation, and can attenuate the electoral impact of compulsory voting. We thank Sourav Bhattacharya, Francisco Cantú, Alessandra Casella, Aimee Chin, Julien Labonne, Arvind Magesan, Eric Mbakop, Suresh Naidu, Mike Ting, and especially Thomas Fujiwara for useful com- ments and suggestions. We also thank seminar participants at Oxford, Columbia, WUSTL, Calgary, the 2016 Wallis Institute Conference, the 2016 Banff Workshop in Empirical Microeconomics, NEUDC 2016, and the 2016 STATA Texas Empirical Microeconomics conference for comments. Thanks to seminar participants at the Indian Statistical Institute Kolkata, Indian Institute of Technology Kanpur, and Public Choice Society 2015 for feedback on an earlier version. We gratefully acknowledge use of the Maxwell/Opuntia Cluster and support from the Center for Advanced Computing and Data Systems at the University of Houston. A previous version of the paper circulated under “‘None Of The Above’Votes in India and the Consumption Utility of Voting”(first version: November 1, 2015). yAuthor affi liations and contact: Department of Economics, University of Houston, [email protected]; Business Environment (Economics) Group, Indian Institute of Management Lucknow, [email protected]; Department of Economics, University of Houston, [email protected].