District Health Plan 2010-2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Stenographer (Post Code-01)
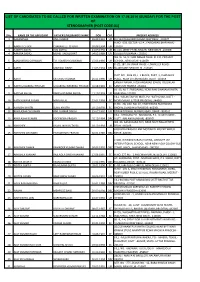
LIST OF CANDIDATES TO BE CALLED FOR WRITTEN EXAMINATION ON 17.08.2014 (SUNDAY) FOR THE POST OF STENOGRAPHER (POST CODE-01) SNo. NAME OF THE APPLICANT FATHER'S/HUSBAND'S NAME DOB CAT. PRESENT ADDRESS 1 AAKANKSHA ANIL KUMAR 28.09.1991 UR B II 544 RAGHUBIR NAGAR NEW DELHI -110027 H.NO. -539, SECTOR -15-A , FARIDABAD (HARYANA) - 2 AAKRITI CHUGH CHARANJEET CHUGH 30.08.1994 UR 121007 3 AAKRITI GOYAL AJAI GOYAL 21.09.1992 UR B -116, WEST PATEL NAGAR, NEW DELHI -110008 4 AAMIRA SADIQ MOHD. SADIQ BHAT 04.05.1989 UR GOOSU PULWAMA - 192301 WZ /G -56, UTTAM NAGAR NEAR, M.C.D. PRIMARY 5 AANOUKSHA GOSWAMI T.R. SOMESH GOSWAMI 15.03.1995 UR SCHOOL, NEW DELHI -110059 R -ZE, 187, JAI VIHAR PHASE -I, NANGLOI ROAD, 6 AARTI MAHIPAL SINGH 21.03.1994 OBC NAJAFGARH NEW DELHI -110043 PLOT NO. -28 & 29, J -1 BLOCK, PART -1, CHANAKYA 7 AARTI SATENDER KUMAR 20.01.1990 UR PLACE, NEAR UTTAM NAGAR, DELHI -110059 SANJAY NAGAR, HOSHANGABAD (GWOL TOLI) NEAR 8 AARTI GULABRAO THOSAR GULABRAO BAKERAO THOSAR 30.08.1991 SC SANTOSHI TEMPLE -461001 I B -35, N.I.T. FARIDABAD, NEAR RAM DHARAM KANTA, 9 AASTHA AHUJA RAKESH KUMAR AHUJA 11.10.1993 UR HARYANA -121001 VILL. -MILAK TAJPUR MAFI, PO. -KATHGHAR, DISTT. - 10 AATIK KUMAR SAGAR MADAN LAL 22.01.1993 SC MORADABAD (UTTAR PRADESH) -244001 H.NO. -78, GALI NO. 02, KHATIKPURA BUDHWARA 11 AAYUSHI KHATRI SUNIL KHATRI 10.10.1993 SC BHOPAL (MADHYA PRADESH) -462001 12 ABHILASHA CHOUHAN ANIL KUMAR SINGH 25.07.1992 UR RIYASAT PAWAI, AURANGABAD, BIHAR - 824101 VILL. -

JMSCR Vol||07||Issue||08||Page 09-13||August 2019
JMSCR Vol||07||Issue||08||Page 09-13||August 2019 http://jmscr.igmpublication.org/home/ ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v7i8.02 Skeletal Metastasis in Carcinoma Gallbladder Authors Dr Satyendra Narayan Sinha1*, Dr Madhulika2, Dr Manisha Singh3 1Radiation Oncology Department, Paras HMRI Hospital, Patna (India) 2Medical Oncology Department, Mahavir Cancer Sansthan, Phulwarisharif, Patna (India) 3Head, Medical Oncology Department, Mahavir Cancer Sansthan, Phulwarisharif, Patna (India) *Corresponding Author Dr Satyendra Narayan Sinha Radiation Oncology Department, Paras HMRI Hospital, Patna (India) Abstract Gallbladder carcinoma is the 5th most common gastrointestinal tract cancers and is an aggressive malignancy with varied presentation. The predominant sites of mestatasis being liver and regional lymph nodes. Skeletal metastasis in gallbladder carcinoma is very rare and only 15 cases have been reported in English literature so far. In this manuscript, we describe our experience of two cases of skeletal metastasis in carcinoma gallbladder. Keywords: Gallbladder Cancer, Skeletal Metastasis in Gallbladder Cancer, Bony Metastasis. Introduction Case Report – 1 Gallbladder cancer is the most common of all the A normotensive and nondiabetic male patient of biliary tract cancers and is fifth most common of age 30 year from Patna (India) presented to the gastrointestinal tract. Gallbladder cancer Mahavir Cancer Sansthan on 8th January 2018 preferentially metastasizes to regional lymph with complain of right hypochondrial pain and nodes and liver parenchyma. Bone metastasis severe back pain for last 3 months. There is past from gallbladder carcinoma are rare presentation. history of lap cholecystectomy and In a study by Sameer G et al.[1] 2.5% patients have appendicectomy on 26th September 2017 outside cytologically proven skeletal metastasis. -

District Health Plan 2010-2011
District Health Plan 2010-2011 District Health Society, Gaya 1 Foreword NRHM was launched in April 2005. The State Health Society (Bihar) and the District Health Societies (Gaya) were formed by end of 2005. The recruitment of Block level managers and other staff were completed by May 2007. The data centre was established by 2006, which worked on outsourced mode. However, a new system replaced the out sourced mode and the data centres were put in place by 2008. Public health system has witnessed an increased utilization of services in 2009 reflected by an increased number of persons being provided every type of service that is available- be it outpatient care, inpatient care, institutional delivery services or emergency services, or surgical services, or laboratory services. The strategy of revitalizing the BPHC and District hospital has shown results. Human resources and Quality of services remains an issue that needs to be addressed. The District Health Planning in Gaya used a situational analysis form focusing on areas in health covered by NRHM viz; RCH, NRHM Additionalities, Immunization, Disease control, and Convergence. This DHAP has been evolved through a participatory and consultative process, wherein community, NGO and other stakeholders have participated and deliberated on the specific health needs. I need to congratulate the SHS Bihar for its dynamic leadership and enthusiasm provided to district level so that the plan is made. We also acknowledge PHRN (NGO partner) for organizing the capacity building programme for the preparation of District Health Action Plan. This District Health Action Plan (DHAP) is one of the key instruments to achieve NRHM goals. -

The Banaras Hindu University (Amendment) Bill, 195 8
C.B. (II) No. -p. LOK SABHA THE BANARAS HINDU UNIVERSITY (AMENDMENT) BILL, 195 8 (Report of the SeleCt Committee) PREsENTED ON lliB" 27TH AUGUST, 1958 T4.2,dN15:(Z).N58t JB 060192 .. LOlt SABRA SECRETARIAT NEW DELHI Aagast, 19S8 CONTE NTis PAGES 1, Composition of the Select Committee i-ii 2. Report of the Select Commi~tee .. iili-v 3· Minutes of Dissent Vi-xvili 4· Bill as amended by the Select Committee APPENDIX I Motion in Lok Sabha for reference of the Bill to Select Committee 9-10 APPENDIX II Minutes of the sittings of the Select Committee • • APPENDIX III Documents circulated to the Select Committee and approved b y them for presentation to Lok Sabha 26-58 838 LS-1. THE BANARAS HINDU UNIVERSITY (AMENDMENT) BILL, 1958. Composition of the Select Committee 1. Sardar Hukam Singh-Chairman. 2. Shri Banarasi Prasad Jhunjhunwala 3. Shri Satyendra Narayan Sinha 4. Shrimati Jayaben Vajubhai Shah 5. Shri Radha Charan Sharma 6. Shri C. R. Narasimhan 7. Shri R. Govindarajulu Naidu 8. Shri T. R. Neswi 9. Shri Hiralal Shastri 10. Shri Tribhuan Narayan Singh 11. Shri Sinhasan Singh 12. Shri Atal Bihari Vajpayee 13. Pandit Munishwar Dutt Upadhyay 14. Shri Birbal Singh 15. Pandit Krishna Chandra Sharma 16. Shri Nardeo Snatak 17. Shri Mahavir Tyagi 18. Shri N. G. Ranga 19. Shri N. R. Ghosh 20. Shri Nibaran Chandra Laskar 21. Shri T. Sanganna 22. Shri Prakash Vir Shastri 23. Shri Prabhat Kar 24. Shri T. Nagi Reddy 25. Shri Braj Raj Singh 26. Shri J. M. Mohamed Imam 27. -

1 AIMS MEMBER INSTITUTIONS North Zone CHANDIGARH Prof
AIMS MEMBER INSTITUTIONS North Zone CHANDIGARH Prof Deepak Kapoor Dean AIMS/AN/CH/NZ/1001 University Business School Punjab University, Chandigarh - 160014 Tel: 0172 - 2541591, 2534701, Mob: 9417006837, Fax: 0172 - 2541591 Email: [email protected], [email protected], Web: http://ubs.puchd.ac.in/ Prof Bhagat Ram Dean AIMS/LF/CH/NZ/2123 ICFAI Business School B 101, Industrial Area, SAS Nagar Phase - 8, Mohali - 160059 Chandigarh Tel: 0172 - 5063547-49 Fax: 0172 - 50635444 Email: [email protected], Website: www.ibsindia.org DELHI Mr Gautam Thapar President AIMS/LF/DLI/NZ/2197 All India Management Association Centre for Management Education "Management House", 14 Institutional Area, Lodhi Road, New Delhi - 110 003 Tel: 011-24645100, 24617354, 43128100, Fax: 011-24626689, Email: [email protected], Website: www.aima-ind.org Mr Raj Kumar Jain Chairman AIMS/AN/DL/NZ/1368 APAR Indian College of Management and Technology Apar Campus, 6 Community Centre, Sector – 8, Rohini 1 Delhi – 110 085 Tel: 011 – 45044000 Email: [email protected] Website: www.aparindiacollege.com Dr Alok Saklani Director AIMS/LF/DLI/NZ/2001 Apeejay School of Management Sector - 8, Dwarka Institutional Area, New Delhi - 110 077 Tel: 011- 25363979/80/83/86/88, 25364523 Fax: 011-25363985 E-mail: [email protected] Website: www.apeejay.edu Dr A N Sarkar Director AIMS/AN/DLI/NZ/1003 Asia-Pacific Institute of Management Plot No: 3 & 4, Institutional Area, Jasola (Opp Sarita Vihar), New Delhi - 110025 Tel: 011 - 42094800 (30 Lines), 011-26950549, 25363978 Fax: 011 - 26951541 E-Mail: -

English Version
htb Series, Vol. V!!. No.1 Tuesday, July 23, 1985 SravanB 1, 1907 (Saka) LOK SABHA DEBA1L.. (English Version) Third Session (Eighth Lok Sabba) (Vol. VII contains Nos. 1 to 10) LOK SABHA SECRETARIAT NEW DELHI Price: Rs. 4.00 [ORIGINAL ENGLISH PROCEEDINGS INClUDFD IN ENGLISh VEIlSION AND OR.IGINAL HINDI PllOcBEDINOS INDCLUDED IN HINDI VI1\SION WILL BB TUATID AS AUTHOlUTATIVE AND NOT THE TIlANSLAnON TJIIUOP.] CONTENTS No.1, Tuelday, July 23, 1985/Sravana 1, 1907 (Saka) CoLUMNS Mcmberswom I Obituary References 1-7 Oral Answer to Questions ·Starred Questions Nos. 1 to 5 7-26 Written Answers to Questions: Starred Questions Nos. 6 to 20 26-38 Unstarred Questions Nos. 1 to 10, 12 to 72, 38-230 74 to 159 and 161 to 214. Re : Adjournment Motion on Proclaiming Eemergency 231-253 Papers Laid on the Table 252-253 Statement Re : (i) Collision of 138 UP Amritsar-Bilaspu.r Chhatis garh Express with Down Tugblalcabad goods train at Raja-Ki Mandi station of Central Railway on 13.6.1985; and (ii) Collision of a private bus with a goods train at' a manned level crossing gate between Dr. Radhakrishnan Nagar and Morwani Stations of Western Railway on 16.6.1985 Shri Bansi Lal 253-256 ~tatement Re: Crash of Air India Jumbo Jet 'KANISHKA' on 23rd June, 1985 Shri Asbok Gehlot 256-258 The Sign+marked above the name of a Member indicates the Question was a«ually asked on the floor of the House b)' that Member. (U) CoLUMNS Statement Re : Report of rthe National Institute of Public Finance and Policy on "Aspects of black Economy in India" Shri Vish wanath Pratap Singh 258-259 Calling Attention to Matter of Urgent Public Importance- 259-285 Armed clashes on Assam-Nagaland border between Assam Police and NagaJand Police Shri Lalit Maken 259-260 263-268 Shri S.B. -
Request for Proposal(Rfp)For Selection of Agency for Advertisement Rights
(A Constituent Unit of Patliputra University, Patna) Grade - 'A' Accredited by NAAC C.P.E. Status by U.G.C. REQUEST FOR PROPOSAL(RFP) FOR SELECTION OF AGENCY FOR ADVERTISEMENT RIGHTS ON HOARDINGS AT COLLEGE CAMPUS , PATNA At Principal , A.N College Boring Road ,Patna Email : [email protected] Website : www.ancpatna.ac.in Selection of Agency for advertisement rights on hoardings at College Campus, Patna Disclaimer 1. Though adequate care has been taken while preparing the RFP document, the Bidders/Applicants shall satisfy them that the document is complete in all respects. Intimation of any discrepancy shall be given to this office immediately. If no intimation is received from any Bidder within fifteen (15) days from the date of notification of RFP /Issue of the RFP documents, it shall be considered that the RFP document is complete in all respects and has been received by the Bidder. 2. Authority reserves the right to modify, amend or supplement this RFP document including all formats and Annexure. Any such change would be communicated to the applicants by posting it on the website www.ancpatna.ac.in. 3. The information provided in this RFP not intended to be an exhaustive on account of statutory requirements and should not be regarded as a complete or authoritative statement of law. The Authority accepts no responsibility for the accuracy or otherwise for any interpretation or opinion on the law expressed herein. 4. The Authority, its employees and advisers make no representation or warranty and shall have no liability to any person including any Applicant under any law, statute, rules or regulations or tort, principles of restitution or unjust enrichment or otherwise for any loss, damages, cost or expense which may arise from or be incurred or suffered on account of anything contained in this RFP or otherwise, including the accuracy, adequacy, correctness, reliability or completeness of the RFP and any assessment, assumption, statement or information contained therein or deemed to form part of this RFP or arising in anyway in this subject. -

Hon' Ble Dy Chief Minister of Bihar- Shri Shushil Kumar Modi
Hon' ble Dy Chief Minister of Bihar- Shri Shushil Kumar Modi Profile of the Dy CM Sushil Kumar Modi was born on the 5th of January, 1952 to Late Shri Moti Lal Modi and Late Smt. Ratna Devi. He started his schooling with Mount Caramel School, Patna where he did his Upper and Lower KG and also Class 1. In St Michaels’ High School, Patna he completed Class 2 and 3 and then joined St Severin’s High School for Class 4th to 6th. He then joined Ram Mohan Roy Seminary for his final schooling i.e. 8th to 10th. It is noteworthy that Mr Modi was a bright student from the start and throughout his school life he secured 1st division. He did his pre-university from Commerce College, Patna and B.Sc. from B.N.College, Patna with a 1st Division. He graduated from the state’s premier institution Patna Science College, Patna University and did his Botany Hons in 1973 securing 2nd position in the whole University. He was a proud scholar and holder of the National Merit Scholarship for Academic Excellence. To pursue his academic career further he enrolled himself in the M.Sc Botany Course in Patna University, but elsewhere lay his calling and as Shri Jai Prakash Narayan called on the young, zealous students from Bihar to make a change in society, he decided to participate in the movement and left College for a year. But who knew that it was the last of his College days and his first of steps into the world of public welfare and politics. -

College ID State University College Name Road City District Pin
College ID State University College name Road City District Pin Payable at IFSC No AC No MICR No BBA2-001 Bihar BBA Bihar Awadh Bihari Singh Mahavidyalaya Lalganj Vaishali Canara Bank,Lalganj Vaishali CNRB 0001252 125220150212 BBA2-003 Bihar BBA Bihar Braj Mohan Das College Dayalpur, Vaishali 844502 Allahabad Bank, Dyalpur Vaishali ALLA0210006 20263644708 844010002 BBA2-004 Bihar BBA Bihar Chandradeo Narain College Sahebganj Muzaffarpur 843125 Central Bank of India, Sahebganj Muzaffarpur CBIN0280026 2195891667 26 BBA2-005 Bihar BBA Bihar Dr S K Sinha Women's College Motihari 845401 State Bank of India, Motihari SBIN0001231 10953148213 845002003 BBA2-006 Bihar BBA Bihar Dr Ram Manohar Lohia Smarak Mahavidyalaya Muzaffarpur 842001 Canara Bank, Motijheel,Muzaffarpur CNRB0000258 0258201001285 842015002 BBA2-007 Bihar BBA Bihar Deo Chand College Hajipur, Vaishali 844101 Hajipur SBIN0012572 31505518429 844002004 BBA2-008 Bihar BBA Bihar Dr Jagannath Mishra College Muzaffarpur 842001 United bank of India, Motijheel, Muzaffarpur UTBIOMTJJ07 0825010102000 8420270002 BBA2-010 Bihar BBA Bihar Jagannath Singh College Chandauli Sitamarhi 843316 State Bank of India, Sitamarhi SBIN0004654 11621131845 843002503 BBA2-011 Bihar BBA Bihar Jamunilal Mahavidyalaya Hajipur Vaishali 844101 Punjab National Bank, Hajipur Vaishali PUNB0403700 4037000100062968 844024002 BBA2-013 Bihar BBA Bihar Jeewachh Mahavidyalaya Motipur, Muzaffarpur 843111 Punjab National Bank, Muzaffarpur PUNB0033400 0334000100194870 842024002 BBA2-015 Bihar BBA Bihar Khem Chand Tara Chand -
LOK SABHA DEBATES (English Version)
Eighth Series, Vol. XXI No. 7 Wednesday, November 12,1986 Kartika 21, 1908 (Saka) LOK SABHA DEBATES (English Version) Seventh Session (Eighth Lok Sabha) ' (Vol. X X I contains Nos. 1 to 10) LOK SABHA SECRETARIAT NEW DELHI Price : R s. 6,00 •» ' It I . i ,*J f * r [Original English proceedings included in English Version and Original Hindi proceedings included in Hindi Version will be treated as authoritative and not the translation thereof.] CONTENTS No. 7, Wednesday, November 12, 1986/Kartika 21, 1908 {Saka) Columns Oral Answers to Questions— 1— 29 ^Starred Questions Nos. 121 to 125 and 128 * Written Answers to Questions— 29— 204 Starred Questions Nos. 126 to 127 and 129 to 140 29— 42 Unstarred Questions Nos. 1258 to 1321 and 1323 to 1397 42— 204 Papers Laid on the Table 212*—221 Message from Rajya Sabha 222 Dock Workers (Safety, Health and. Welfare) Bill—As Amended by 223 Rajya Sabha Committee on Private Members' Bills and Resolution 223 Twenty-fifth Report Election to Committee 223 Central Advisory Committee for National Cadet Cnrps... Business Advisory Committee „ 224 Twenty-Ninth Report Calling Attention to matter of urgent public importance 224 236 Reported fire in Sahar terminal of Bombay airport Shri Sharad Dighe ' 224 Shri Jagdish Tytler 225 Shri Haris Rawat 228 Dr. G. S. Rajhans 229 ^ Shri Jagdish Awasthi Shri Banwari Lai Purohit ’ 2^2 ♦The Sign + marked above the name of a Member indicates that the question was actually asked on the floor of the House by that Member, (ii) Columna Matters Under Rule 377 236— 240 (i) Need to start a new train from Kota or Ratlam to Delhi and to re-start Dehradun Express Shri Shanti Dbariwal 236 (ii) Need to declare the people of Ladakh region as Scheduled Tribe Sliri P. -
The Speaker Made References to the Passing Away of Shri Satyendra
> Title : The Speaker made references to the passing away of Shri Satyendra Narayan Sinha, member of the Provisional Parliament, Ist, 2nd and 5th to 8th Lok Sabhas; Shri Shankararao Patil, member 7th & 9th Lok Sabhas; Shri Ravindra Verma, member 3rd, 6th and 7th Lok Sabhas; Shri Kanshi Ram, member 10th & 11th Lok Sabhas and Shri Bhikku Ram Jain, member 7th Lok Sabha on 04.09.2006, 13.09.2006, 09.10.2006, 09.10.2006 and 10.11.2006 respectively. MR. SPEAKER: Hon. Members, I have to inform the House of the sad demise of five of our former colleagues, Shri Satyendra Narayan Sinha, Shri Shankararao Patil, Shri Ravindra Varma, Shri Kanshi Ram and Shri Bhikhu Ram Jain. Shri Satyendra Narayan Sinha was a Member of the Provisional Parliament, First, Second and Fifth to Eighth Lok Sabhas from 1950 to 1961 and 1971 to 1989 representing Aurangabad parliamentary constituency of Bihar.[MSOffice2] Shri Sinha was a Member of the Bihar Vidhan Sabha from 1961 to 1969 and Vidhan Parishad during 1989. An able administrator, Shri Sinha served as Minister for Education, Local Self Government and Agriculture in the Government of Bihar from 1961 to 1967. He rose to become the Chief Minister of Bihar in 1989. An active parliamentarian, Shri Sinha served as the Chairman of Committee on Estimates from 1977 to 1979. He was also a Member of the Committee on Finance from 1950 to 1952; Committee on Estimates from 1956 to 1958 and thereafter during 1985-86 and the Committee on Public Undertakings during 1982-83. An advocate by profession, Shri Sinha organized Legal Aid Programmes for political prisoners during pre-Independence days. -

Information to Users
INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand corner and continuing from left to right in equal sections with small overlaps. ProQuest Information and Learning 300 North Zeeb Road, Ann Arbor, Ml 48106-1346 USA 800-521-0600 UMI UNIVERSITY OF OKLAHOMA GRADUATE COLLEGE PEASANT UNREST, COMMUNITY WARRIORS AND STATE POWER IN INDIA: THE CASE OF PRIVATE CASTE SENAS (ARMIES) IN BIHAR A Dissertation SUBMITTED TO THE GRADUATE COLLGE in partial fulfillment of the requirements for the degree of Doctor of Philosophy By Ashwani Kumar Norman, Oklahoma 2003 UMI Number: 3082961 UMI” UMI Microform 3082961 Copyright 2003 by ProQuest Information and Learning Company. All rights reserved. This microform edition is protected against unauthorized copying under Title 17, United States Code. ProQuest Information and Learning Company 300 North Zeeb Road P.O. Box 1346 Ann Arbor, Ml 48106-1346 © Copyright by ASHWANI KUMAR 2003 All Rights Reserved PEASANT UNREST, COMMUNITY WARRIORS AND STATE POWER IN INDIA: THE CASE OF PRIVATE CASTE SENAS (ARMIES) IN BIHAR A Dissertation APPROVED FOR THE DEPARTMENT OF POLITICAL SCIENCE BY Dr.