Letters Anterior Part of the Cingulate Gyrus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex Hans Ten Donkelaar, Nathalie Tzourio-Mazoyer, Jürgen Mai
Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex Hans ten Donkelaar, Nathalie Tzourio-Mazoyer, Jürgen Mai To cite this version: Hans ten Donkelaar, Nathalie Tzourio-Mazoyer, Jürgen Mai. Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex. Frontiers in Neuroanatomy, Frontiers, 2018, 12, pp.93. 10.3389/fnana.2018.00093. hal-01929541 HAL Id: hal-01929541 https://hal.archives-ouvertes.fr/hal-01929541 Submitted on 21 Nov 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. REVIEW published: 19 November 2018 doi: 10.3389/fnana.2018.00093 Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex Hans J. ten Donkelaar 1*†, Nathalie Tzourio-Mazoyer 2† and Jürgen K. Mai 3† 1 Department of Neurology, Donders Center for Medical Neuroscience, Radboud University Medical Center, Nijmegen, Netherlands, 2 IMN Institut des Maladies Neurodégénératives UMR 5293, Université de Bordeaux, Bordeaux, France, 3 Institute for Anatomy, Heinrich Heine University, Düsseldorf, Germany The gyri and sulci of the human brain were defined by pioneers such as Louis-Pierre Gratiolet and Alexander Ecker, and extensified by, among others, Dejerine (1895) and von Economo and Koskinas (1925). -

1. Lateral View of Lobes in Left Hemisphere TOPOGRAPHY
TOPOGRAPHY T1 Division of Cerebral Cortex into Lobes 1. Lateral View of Lobes in Left Hemisphere 2. Medial View of Lobes in Right Hemisphere PARIETAL PARIETAL LIMBIC FRONTAL FRONTAL INSULAR: buried OCCIPITAL OCCIPITAL in lateral fissure TEMPORAL TEMPORAL 3. Dorsal View of Lobes 4. Ventral View of Lobes PARIETAL TEMPORAL LIMBIC FRONTAL OCCIPITAL FRONTAL OCCIPITAL Comment: The cerebral lobes are arbitrary divisions of the cerebrum, taking their names, for the most part, from overlying bones. They are not functional subdivisions of the brain, but serve as a reference for locating specific functions within them. The anterior (rostral) end of the frontal lobe is referred to as the frontal pole. Similarly, the anterior end of the temporal lobe is the temporal pole, and the posterior end of the occipital lobe the occipital pole. TOPOGRAPHY T2 central sulcus central sulcus parietal frontal occipital lateral temporal lateral sulcus sulcus SUMMARY CARTOON: LOBES SUMMARY CARTOON: GYRI Lateral View of Left Hemisphere central sulcus postcentral superior parietal superior precentral gyrus gyrus lobule frontal intraparietal sulcus gyrus inferior parietal lobule: supramarginal and angular gyri middle frontal parieto-occipital sulcus gyrus incision for close-up below OP T preoccipital O notch inferior frontal cerebellum gyrus: O-orbital lateral T-triangular sulcus superior, middle and inferior temporal gyri OP-opercular Lateral View of Insula central sulcus cut surface corresponding to incision in above figure insula superior temporal gyrus Comment: Insula (insular gyri) exposed by removal of overlying opercula (“lids” of frontal and parietal cortex). TOPOGRAPHY T3 Language sites and arcuate fasciculus. MRI reconstruction from a volunteer. central sulcus supramarginal site (posterior Wernicke’s) Language sites (squares) approximated from electrical stimulation sites in patients undergoing operations for epilepsy or tumor removal (Ojeman and Berger). -

White Matter Anatomy: What the Radiologist Needs to Know
White Matter Anatomy What the Radiologist Needs to Know Victor Wycoco, MBBS, FRANZCRa, Manohar Shroff, MD, DABR, FRCPCa,*, Sniya Sudhakar, MBBS, DNB, MDb, Wayne Lee, MSca KEYWORDS Diffusion tensor imaging (DTI) White matter tracts Projection fibers Association Fibers Commissural fibers KEY POINTS Diffusion tensor imaging (DTI) has emerged as an excellent tool for in vivo demonstration of white matter microstructure and has revolutionized our understanding of the same. Information on normal connectivity and relations of different white matter networks and their role in different disease conditions is still evolving. Evidence is mounting on causal relations of abnormal white matter microstructure and connectivity in a wide range of pediatric neurocognitive and white matter diseases. Hence there is a pressing need for every neuroradiologist to acquire a strong basic knowledge of white matter anatomy and to make an effort to apply this knowledge in routine reporting. INTRODUCTION (Fig. 1). However, the use of specific DTI sequences provides far more detailed and clini- DTI has allowed in vivo demonstration of axonal cally useful information. architecture and connectivity. This technique has set the stage for numerous studies on normal and abnormal connectivity and their role in devel- DIFFUSION TENSOR IMAGING: THE BASICS opmental and acquired disorders. Referencing established white matter anatomy, DTI atlases, Using appropriate magnetic field gradients, and neuroanatomical descriptions, this article diffusion-weighted sequences can be used to summarizes the major white matter anatomy and detect the motion of the water molecules to and related structures relevant to the clinical neurora- from cells. This free movement of the water mole- diologist in daily practice. -
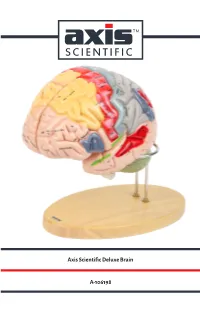
Axis Scientific Deluxe Brain A-106198
Axis Scientific Deluxe Brain A-106198 Hypothalamic Pineal Cingulate Paracentral Sagittal View Interventricular foramen sulcus recess sulcus Sagittal View (Right) (Foramen of Monro) lobule (Left) Anterior View Precuneus Cingulate gyrus Body of fornix Interthalamic adhesion Splenium of Body of corpus callosum corpus callosum Superior frontal gyrus Lateral ventricle Cavity of third ventricle Cuneus Sulcus of corpus callosum Calcarine Septum pellucidum Posterior commissure sulcus Genu of corpus callosum Lateral View Pineal Cingulate sulcus (subfrontal) (Right) gland Anterior commissure Sylvian Lamina terminalis Superior medullary aqueduct vellum Optic recess Anterior Corpora Optic chiasm commissure quadrigemina Infundibular recess Vermis of cerebellum Vermis of Tuber cinereum Frontal lobe Pituitary gland cerebellum Pons Mammillary body Oculomotor nerve Arbor vitae Hypoglossal Pons Fourth Interpeduncular nerve (CN XII) (CN Ill) (Cerebellar white ventricle Cerebral fossa matter) peduncle Olive Pyramidal Medulla Longitudinal Decussation tract Vestibulocochlear Central canal of oblongata fibers of pons of pyramids nerve (CN VIII) medulla oblongata Medial longitudinal Flocculus of cerebellum Abducens nerve (CN VI) fasciculus Glossopharyngeal nerve (CN IX) Pyramidal tract Corona radiata Lateral View Posterior Lateral Vagus nerve (CN X) Hypoglossal nerve (CN XII) Inferior parietal (Left) Pre-central Central View (Left) Lateral geniculate body Lentiform Olive Motor area sulcus Post-central lobe lntraparietal Cerebellar tonsil sulcus sulcus nucleus -

01 08 Ventral Surface of the Brain-NOTES.Pdf
Ventral Surface of the Brain Medical Neuroscience | Tutorial Notes Ventral Surface of the Brain 1 MAP TO NEUROSCIENCE CORE CONCEPTS NCC1. The brain is the body's most complex organ. LEARNING OBJECTIVES After study of the assigned learning materials, the student will: 1. Describe the major features of the cerebral lobes, as seen from the ventral view, discussing major gyri and sulci that characterize each lobe. 2. Recognize the major embryological subdivisions of the brain that are visible from the ventral view. NARRATIVE by Leonard E. WHITE and Nell B. CANT Duke Institute for Brain Sciences Department of Neurobiology Duke University School of Medicine Overview When you view the lateral aspect of a human brain specimen (see Figures A3A and A112), three structures are usually visible: the cerebral hemispheres, the cerebellum, and part of the brainstem (although the brainstem is not visible in the specimen photographed in lateral view for Fig. 1 below). The spinal cord has usually been severed (but we’ll consider the spinal cord later), and the rest of the subdivisions are hidden from lateral view by the hemispheres. The diencephalon and the rest of the brainstem are visible on the medial surface of a brain that has been cut in the midsagittal plane. Parts of all of the subdivisions are also visible from the ventral surface of the whole brain. In this set of tutorials, you will find video demonstrations (from the brain anatomy lab) and photographs (in the tutorial notes) of these brain surfaces, and sufficient detail in the narrative to appreciate the overall organization of the parts of the brain that are visible from each perspective. -
Anatomy and White Matter Connections of the Orbitofrontal Gyrus
LABORATORY INVESTIGATION J Neurosurg 128:1865–1872, 2018 Anatomy and white matter connections of the orbitofrontal gyrus Joshua D. Burks, MD,1 Andrew K. Conner, MD,1 Phillip A. Bonney, MD,1 Chad A. Glenn, MD,1 Cordell M. Baker, BS,1 Lillian B. Boettcher, BS,1 Robert G. Briggs, BS,1 Daniel L. O’Donoghue, PhD,2 Dee H. Wu, PhD,3 and Michael E. Sughrue, MD1 Departments of 1Neurosurgery, 2Cell Biology, and 3Radiological Sciences, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma OBJECTIVE The orbitofrontal cortex (OFC) is understood to have a role in outcome evaluation and risk assessment and is commonly involved with infiltrative tumors. A detailed understanding of the exact location and nature of associated white matter tracts could significantly improve postoperative morbidity related to declining capacity. Through diffusion tensor imaging–based fiber tracking validated by gross anatomical dissection as ground truth, the authors have charac- terized these connections based on relationships to other well-known structures. METHODS Diffusion imaging from the Human Connectome Project for 10 healthy adult controls was used for tractogra- phy analysis. The OFC was evaluated as a whole based on connectivity with other regions. All OFC tracts were mapped in both hemispheres, and a lateralization index was calculated with resultant tract volumes. Ten postmortem dissections were then performed using a modified Klingler technique to demonstrate the location of major tracts. RESULTS The authors identified 3 major connections of the OFC: a bundle to the thalamus and anterior cingulate gyrus, passing inferior to the caudate and medial to the vertical fibers of the thalamic projections; a bundle to the brain- stem, traveling lateral to the caudate and medial to the internal capsule; and radiations to the parietal and occipital lobes traveling with the inferior fronto-occipital fasciculus. -
Neuroanatomy for the Neuroscientist Stanley Jacobson • Elliott M
Neuroanatomy for the Neuroscientist Stanley Jacobson • Elliott M. Marcus Neuroanatomy for the Neuroscientist Stanley Jacobson Elliott M. Marcus Tufts University Health Science Schools University of Massachusetts Boston, MA School of Medicine USA Worcester, MA USA ISBN 978-0-387-70970-3 e-ISBN 978-0-387-70971-0 DOI: 10.1007/978-0-387-70971-0 Library of Congress Control Number: 2007934277 © 2008 Springer Science + Business Media, LLC All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science + Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identified as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. Printed on acid-free paper 9 8 7 6 5 4 3 2 1 springer.com To our families who showed infinite patience: To our wives Avis Jacobson and Nuran Turksoy To our children Arthur Jacobson and Robin Seidman Erin Marcus and David Letson To our grandchildren Ross Jacobson Zachary Letson and Amelia Letson Preface The purpose of this textbook is to enable a neuroscientist to discuss the structure and functions of the brain at a level appropriate for students at many levels of study, including undergraduate, graduate, dental, or medical school level. -

The Cerebral Sulci and Gyri
Neurosurg Focus 28 (2):E2, 2010 The cerebral sulci and gyri GUILHERME CARVALHAL RIBAS, M.D. Department of Surgery, University of São Paulo Medical School—LIM-02, Hospital Israelita Albert Einstein, São Paulo, Brazil The aim of this study was to describe in detail the microanatomy of the cerebral sulci and gyri, clarifying the nomenclature for microneurosurgical purposes. An extensive review of the literature regarding the historical, evo- lutionary, embryological, and anatomical aspects pertinent to human cerebral sulci and gyri was conducted, with a special focus on microneuroanatomy issues in the field of neurosurgery. An intimate knowledge of the cerebral sulci and gyri is needed to understand neuroimaging studies, as well as to plan and execute current microneurosurgical procedures. (DOI: 10.3171/2009.11.FOCUS09245) KEY WORDS • brain gyrus • brain mapping • brain sulcus • cerebral cortex • cerebral lobe LTHOUGH there is no strict relationship between atized surgical procedure.23 As early as ~ 10,000 years brain structure and function, current knowledge ago, cranial trephination was performed “successfully” shows that the two are closely interrelated. The (that is, with new bone formation after the procedure) in Abrain is divided into regions and subdivided into more the neolithic cultures of Europe, and there are findings specific zones, although there is increasing evidence that dating to 2000 years ago in South America, where the the borders between those zones are much blurrier than practice was particularly common in the pre-Incan -
Cerebrum and Functional Areas of Brain
Cerebrum and Functional Areas Amadi O. Ihunwo, PhD School of Anatomical Sciences Lecture Outline • Review sulci and gyri of cerebral hemisphere • Functional Areas Cerebral Hemispheres • Largest part of the brain • Greatest degree of development is in humans • Ocupy the anterior and middle cranial fossae • Consist of an outer cerebral cortex and an inner white matter • A median longitudinal fissure incompletely separates the cerebrum into 2 halves; right and left Gyri and Sulci • Gyri – Complicated irregular foldings (convolutions) of surface of cerebral hemispheres • Sulci – Intervening grooves between gyri. – May be shallow or deep. – Sometimes deep sulci are called fissures. • Gyri & sulci maximise surface of cerebrum; – 70% of cerebrum is hidden in sulci. – Fairly constant, at the same time, vary within certain limits, not only from one brain to another, but within the same brain. Superolateral surface of cerebrum • Lateral sulcus (Sylvius): between frontal, Parietal & temporal lobes. • Central sulcus (Rolando): 1 cm post to midpoint between frontal & occipital pole; Runs downwards & ends just before lateral sulcus; Landmark separating frontal from parietal lobes • Frontal lobe: Largest: 3 sulci: Parietal Lobe Precentral sulcus, Superior & inferior frontal sulci Sulcus: Postcentral & Intraparietal Gyri: Postcentral, superior parietal • 4 gyri: Precentral gyrus, Superior, middle & inferior gyri lobule, inferior parietal lobule with supramarginal & angular gyri Temporal & Occipital lobes • Temporal lobe Lies inferior to lateral sulcus. Sulci: superior & inferior Gyri: superior, middle & inferior. • Occipital lobe Posterior to line joining pre- occipital notch to parieto- occipital sulcus (medial surface) Lateral occipital sulcus (lunate) o The only fairly constant sulcus on superolateral surface o Calcarine sulcus (medial surface) Medial Surface • Corpus callosum – most conspicuous structure; white matter • Cingulate sulcus – intervenes between cingulate gyrus & extension of superior frontal gyrus. -

MR Imaging of the Temporal Stem: Anatomic Dissection
AJNR Am J Neuroradiol 25:677–691, May 2004 MR Imaging of the Temporal Stem: Anatomic Dissection Tractography of the Uncinate Fasciculus, Inferior Occipitofrontal Fasciculus, and Meyer’s Loop of the Optic Radiation E. Leon Kier, Lawrence H. Staib, Lawrence M. Davis, and Richard A. Bronen BACKGROUND AND PURPOSE: The MR anatomy of the uncinate fasciculus, inferior occipitofrontal fasciculus, and Meyer’s loop of the optic radiation, which traverse the temporal stem, is not well known. The purpose of this investigation was to study these structures in the anterior temporal lobe and the external and extreme capsules and to correlate the dissected anatomy with the cross-sectional MR anatomy. METHODS: Progressive dissection was guided by three-dimensional MR renderings and cross- sectional images. Dissected segments of the tracts and the temporal stem were traced and projected onto reformatted images. The method of dissection tractography is detailed in a companion article. RESULTS: The temporal stem extends posteriorly from the level of the amygdala to the level of the lateral geniculate body. The uncinate and inferior occipitofrontal fasciculi pass from the temporal lobe into the extreme and external capsules via the temporal stem. Meyer’s loop extends to the level of the amygdala, adjacent to the uncinate fasciculus and anterior commis- sure. These anatomic features were demonstrated on correlative cross-sectional MR images and compared with clinical examples. CONCLUSION: This study clarified the MR anatomy of the uncinate and inferior occipitofrontal fasciculi and Meyer’s loop in the temporal stem and in the external and extreme capsules, helping to explain patterns of tumor spread. -
Sulci-Tracing Protocol.Pdf
For this protocol of BrainSuite all sulci are traced on the brain’s midcortical surface. On occasion, when sulci are very deep, they may be shown on a gray/white junction surface (but the curves will have been traced on the midcortical surface). All sulci are traced at a 0.5 of “stickiness”. When jumping over gyri which interrupt the course of a sulcus it is best to remove the “stickiness’ because it facilitates the placement of the curve. It is also advisable to turn the surface view in such a way that the dropping of a point is done perpendicular to the deep surface where the point is meant to be dropped. The different sulci curves cannot touch one another, there has to be a gap between them. This is important to keep in mind when, on occasion, some sulci actually cross other sulci. For alignment purposes they have to be kept separate. The sequence in which the sulci are traced is arbitrary. Here, and in the actual protocol in BrainSuite, the sulci are ordered by lobes, starting with the Frontal, continuing with the Temporal, the Parietal and finally the Occipital. In the Frontal and Parietal lobes I start with the dorsolateral views, move to the mesial views, and to the inferior view (in the frontal lobe). The Temporal lobe starts on the dorsolateral view and gradually proceeds to the mesial view. The occipital lobe starts with the mesial view because this is the view where its major sulci are seen, and finishes with the dorsolateral view. For a general overview, the first images show the brain in straight lateral, mesial and inferior views, with all sulci traced and identified with the abbreviations of the sulci names (all introduced in the text for the individual sulci). -

The Cerebral Sulci and Gyri
Neurosurg Focus 28 (2):E2, 2010 The cerebral sulci and gyri GUILHERME CARVALHAL RIBAS, M.D. Department of Surgery, University of São Paulo Medical School—LIM-02, Hospital Israelita Albert Einstein, São Paulo, Brazil The aim of this study was to describe in detail the microanatomy of the cerebral sulci and gyri, clarifying the nomenclature for microneurosurgical purposes. An extensive review of the literature regarding the historical, evo- lutionary, embryological, and anatomical aspects pertinent to human cerebral sulci and gyri was conducted, with a and gyri is needed to understand neuroimaging studies, as well as to plan and execute current microneurosurgical procedures. (DOI: 10.3171/2009.11.FOCUS09245) KEY WORDS LTHOUGH there is no strict relationship between 23 As early as ~ 10,000 years brain structure and function, current knowledge ago, cranial trephination was performed “successfully” Ashows that the two are closely interrelated. The (that is, with new bone formation after the procedure) in brain is divided into regions and subdivided into more dating to 2000 years ago in South America, where the practice was particularly common in the pre-Incan and was previously thought.35 Therefore, it is essential that Incan cultures of Peru.26 Despite this historical context, neurosurgeons have an intimate knowledge of brain mi- knowledge of the anatomy of the brain in general and of croanatomy, not only to improve their understanding of its surface in particular is quite recent.23,26,38 neuroimaging studies, but also to allow them to plan and perform neurosurgical procedures while considering par- ticular brain functions. Hippocrates (460–370 BC), who is considered the father of medicine, posited that the brain was responsible for mental activities and convulsions, whereas some impor- and transsulcal approaches80,84,85 have established the sul- tant Greek philosophers, such as Aristotle (384–322 BC), ci as fundamental landmarks on the brain surface.