Inhaled Corticosteroid Use in COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Difference Between Patient-Reported Side Effects of Ciclesonide Versus fluticasone Propionate
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Respiratory Medicine (2010) 104, 1825e1833 available at www.sciencedirect.com journal homepage: www.elsevier.com/locate/rmed Difference between patient-reported side effects of ciclesonide versus fluticasone propionate Thys van der Molen a, Juliet M. Foster a,b, Manfred Caeser c,e, Thomas Mu¨ller c, Dirkje S. Postma d,* a Department of General Practice, University Medical Center Groningen, University of Groningen, Hanzeplein 1, 9700 RB, Groningen, The Netherlands b Woolcock Institute of Medical Research, 431 Glebe Point Rd, Glebe NSW 2037, Sydney, Australia c Nycomed GmbH, Byk-Gulden-Straße 2, 78467 Konstanz, Konstanz, Germany d Department of Pulmonary Diseases, University Medical Center Groningen, University of Groningen, Hanzeplein 1, 9700 RB, Groningen, The Netherlands Received 18 January 2010; accepted 26 May 2010 Available online 2 July 2010 KEYWORDS Summary Adverse events; Rationale: Patient-reported outcomes provide new insights into the dynamics of asthma Inhaled corticosteroid management. Further to asthma control and quality of life, self-reported side effects of treat- questionnaire; ment can be assessed with the validated Inhaled Corticosteroid Questionnaire (ICQ). ICQ; Objectives: To compare patient-reported side effects between the inhaled corticosteroids Patient-reported ciclesonide and fluticasone propionate. outcomes Methods: Patients with moderate or moderate-to-severe asthma, pre-treated with a constant dose and type of medication, were randomized in three separate studies: 1) once daily cicle- sonide 320 mg(n Z 234) or twice daily fluticasone propionate 200 mg(n Z 240); 2) twice daily ciclesonide 320 mg(n Z 255) or twice daily fluticasone propionate 375 mg(n Z 273); and 3) twice daily ciclesonide 320 mg(n Z 259) or twice daily fluticasone propionate 500 mg (n Z 244). -

The Inhaled Steroid Ciclesonide Blocks SARS-Cov-2 RNA Replication by Targeting Viral
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.22.258459; this version posted August 24, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting viral 2 replication-transcription complex in culture cells 3 4 Shutoku Matsuyamaa#, Miyuki Kawasea, Naganori Naoa, Kazuya Shiratoa, Makoto Ujikeb, Wataru 5 Kamitanic, Masayuki Shimojimad, and Shuetsu Fukushid 6 7 aDepartment of Virology III, National Institute of Infectious Diseases, Tokyo, Japan 8 bFaculty of Veterinary Medicine, Nippon Veterinary and Life Science University, Tokyo, Japan 9 cDepartment of Infectious Diseases and Host Defense, Gunma University Graduate School of 10 Medicine, Gunma, Japan 11 dDepartment of Virology I, National Institute of Infectious Diseases, Tokyo, Japan. 12 13 Running Head: Ciclesonide blocks SARS-CoV-2 replication 14 15 #Address correspondence to Shutoku Matsuyama, [email protected] 16 17 Word count: Abstract 149, Text 3,016 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.22.258459; this version posted August 24, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 18 Abstract 19 We screened steroid compounds to obtain a drug expected to block host inflammatory responses and 20 MERS-CoV replication. Ciclesonide, an inhaled corticosteroid, suppressed replication of MERS-CoV 21 and other coronaviruses, including SARS-CoV-2, the cause of COVID-19, in cultured cells. The 22 effective concentration (EC90) of ciclesonide for SARS-CoV-2 in differentiated human bronchial 23 tracheal epithelial cells was 0.55 μM. -

Etats Rapides
List of European Pharmacopoeia Reference Standards Effective from 2015/12/24 Order Reference Standard Batch n° Quantity Sale Information Monograph Leaflet Storage Price Code per vial Unit Y0001756 Exemestane for system suitability 1 10 mg 1 2766 Yes +5°C ± 3°C 79 ! Y0001561 Abacavir sulfate 1 20 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001552 Abacavir for peak identification 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001551 Abacavir for system suitability 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0000055 Acamprosate calcium - reference spectrum 1 n/a 1 1585 79 ! Y0000116 Acamprosate impurity A 1 50 mg 1 3-aminopropane-1-sulphonic acid 1585 Yes +5°C ± 3°C 79 ! Y0000500 Acarbose 3 100 mg 1 See leaflet ; Batch 2 is valid until 31 August 2015 2089 Yes +5°C ± 3°C 79 ! Y0000354 Acarbose for identification 1 10 mg 1 2089 Yes +5°C ± 3°C 79 ! Y0000427 Acarbose for peak identification 3 20 mg 1 Batch 2 is valid until 31 January 2015 2089 Yes +5°C ± 3°C 79 ! A0040000 Acebutolol hydrochloride 1 50 mg 1 0871 Yes +5°C ± 3°C 79 ! Y0000359 Acebutolol impurity B 2 10 mg 1 -[3-acetyl-4-[(2RS)-2-hydroxy-3-[(1-methylethyl)amino] propoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! acetamide (diacetolol) Y0000127 Acebutolol impurity C 1 20 mg 1 N-(3-acetyl-4-hydroxyphenyl)butanamide 0871 Yes +5°C ± 3°C 79 ! Y0000128 Acebutolol impurity I 2 0.004 mg 1 N-[3-acetyl-4-[(2RS)-3-(ethylamino)-2-hydroxypropoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! butanamide Y0000056 Aceclofenac - reference spectrum 1 n/a 1 1281 79 ! Y0000085 Aceclofenac impurity F 2 15 mg 1 benzyl[[[2-[(2,6-dichlorophenyl)amino]phenyl]acetyl]oxy]acetate -

Ep 2626065 A1
(19) TZZ Z_T (11) EP 2 626 065 A1 (12) EUROPEAN PATENT APPLICATION published in accordance with Art. 153(4) EPC (43) Date of publication: (51) Int Cl.: A61K 31/137 (2006.01) A61K 31/135 (2006.01) 14.08.2013 Bulletin 2013/33 A61K 31/4704 (2006.01) A61K 31/58 (2006.01) A61K 31/56 (2006.01) A61K 9/12 (2006.01) (2006.01) (2006.01) (21) Application number: 11827927.2 A61K 9/14 A61P 11/06 (86) International application number: Date of filing: 01.02.2011 (22) PCT/CN2011/070883 (87) International publication number: WO 2012/041031 (05.04.2012 Gazette 2012/14) (84) Designated Contracting States: (72) Inventor: WU, Wei-hsiu AL AT BE BG CH CY CZ DE DK EE ES FI FR GB Taipei GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO Taiwan (TW) PL PT RO RS SE SI SK SM TR (74) Representative: Patentanwaltskanzlei WILHELM (30) Priority: 28.09.2010 CN 201010502339 & BECK Prinzenstrasse 13 (71) Applicant: Intech Biopharm Ltd. 80639 München (DE) Taipei (TW) (54) COMPOUND COMPOSITION FOR INHALATION USED FOR TREATING ASTHMA (57) An inhaled pharmaceutical composition con- tric way as a controller. The eccentric way control therapy tains primary active ingredients of beta2- agonist and cor- could create a low blood concentration period during the ticosteroids.The pharmaceuticalcompositions disclosed day and minimize the acute tolerance phenomenon (or in the present invention are to be inhaled by a patient so called tachyphylaxis) for bronchodilator - beta2-ago- when needed as a reliever, or administrated in an eccen- nists in treating asthma or other obstructive respiratory disorders. -
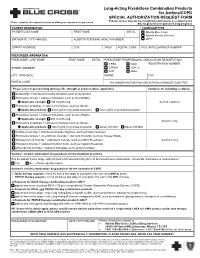
Long-Acting Fixed-Dose Combination Products for Asthma/COPD SPECIAL AUTHORIZATION REQUEST FORM
Long-Acting Fixed-Dose Combination Products for Asthma/COPD SPECIAL AUTHORIZATION REQUEST FORM Patients may or may not meet eligibility requirements as established by Please complete all required sections to allow your request to be processed Alberta government-sponsored drug programs PATIENT INFORMATION COVERAGE TYPE PATIENT LAST NAME FIRST NAME INITIAL Alberta Blue Cross Alberta Human Services BIRTHDATE (YYYY-MM-DD) ALBERTA PERSONAL HEALTH NUMBER Other STREET ADDRESS CITY PROV POSTAL CODE ID/CLIENT/COVERAGE NUMBER PRESCRIBER INFORMATION PRESCRIBER LAST NAME FIRST NAME INITIAL PRESCRIBER PROFESSIONAL ASSOCIATION REGISTRATION CPSA ACO REGISTRATION NUMBER STREET ADDRESS CARNA ADA+C ACP Other CITY , PROVINCE PHONE FAX POSTAL CODE FAX NUMBER MUST BE PROVIDED WITH EACH REQUEST SUBMITTED Please select requested drug (and specific strength or product, where applicable) Complete the following section(s) Budesonide + formoterol fumarate dihydrate (such as Symbicort) Fluticasone furoate + vilanterol trifenatate (such as Breo Ellipta) Applicable strength 100 mcg/25 mcg Section I and/or II Fluticasone propionate + salmeterol xinafoate (such as Advair) Applicable products 250 mcg/50 mcg inhalation powder 500 mcg/50 mcg inhalation powder Fluticasone furoate + vilanterol trifenatate (such as Breo Ellipta) Applicable strength 200 mcg/25 mcg Section I only Fluticasone propionate + salmeterol xinafoate (such as Advair) Applicable products 100 mcg/50 mcg inhalation powder Advair 125 MDI Advair 250 MDI Aclidinium bromide + formoterol fumarate dihydrate (such as Duaklir Genuair) Fluticasone furoate + umeclidinium bromide + vilanterol trifenatate (such as Trelegy Ellipta) Glycopyrronium bromide + indacaterol maleate (such as Ultibro Breezhaler) Section II only Tiotropium bromide + olodaterol hydrochloride (such as Inspiolto Respimat) Umeclidinium bromide + vilanterol trifenatate (such as Anoro Ellipta) Section I. -

Utah Medicaid Pharmacy and Therapeutics Committee Drug
Utah Medicaid Pharmacy and Therapeutics Committee Drug Class Review Single Ingredient Nasal Corticosteroids Beclomethasone dipropionate (Qnasl) Beclomethasone dipropionate monohydrate (Beconase AQ) Budesonide (Rhinocort) Ciclesonide (Omnaris, Zetonna) Flunisolide (Generic) Fluticasone Furoate (Flonase Sensimist) Fluticasone Propionate (Flonase, Xhance) Mometasone Furoate (Nasonex) Triamcinolone Acetonide (Nasacort) AHFS Classification: 52.08.08 Corticosteroids (EENT) Final Report February 2018 Review prepared by: Valerie Gonzales, Pharm.D., Clinical Pharmacist Elena Martinez Alonso, B.Pharm., MSc MTSI, Medical Writer Vicki Frydrych, Pharm.D., Clinical Pharmacist Joanita Lake, B.Pharm., MSc EBHC (Oxon), Research Assistant Professor Joanne LaFleur, Pharm.D., MSPH, Associate Professor University of Utah College of Pharmacy University of Utah College of Pharmacy, Drug Regimen Review Center Copyright © 2018 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved Contents Abbreviations ................................................................................................................................................ 2 Executive Summary ....................................................................................................................................... 3 Introduction .................................................................................................................................................. 5 Table 1. Nasal corticosteroid products ............................................................................................. -

Drug Class Review Nasal Corticosteroids
Drug Class Review Nasal Corticosteroids Final Report Update 1 June 2008 The Agency for Healthcare Research and Quality has not yet seen or approved this report The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Dana Selover, MD Tracy Dana, MLS Colleen Smith, PharmD Kim Peterson, MS Oregon Evidence-based Practice Center Oregon Health & Science University Mark Helfand, MD, MPH, Director Marian McDonagh, PharmD, Principal Investigator, Drug Effectiveness Review Project Copyright © 2008 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 1 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION ..........................................................................................................................5 Scope and Key Questions .......................................................................................................................7 METHODS ....................................................................................................................................9 Literature Search .....................................................................................................................................9 -

Impact of Study Design on the Evaluation of Inhaled And
REVIEW Impact of Study Design on the Evaluation of Inhaled and Intranasal Corticosteroids’ Effect on Hypothalamic–Pituitary–Adrenal Axis Function, Part I: General Overview of HPA Axis Study Design YING FAN,1 LIAN MA,2 JENNIFER PIPPINS,3 SUSAN LIMB,3 YUN XU,1 CHANDRAHAS G. SAHAJWALLA1 1Division of Clinical Pharmacology II, Office of Clinical Pharmacology, US Food and Drug Administration, Silver Spring, Maryland 2College of Pharmacy, Oregon State University, Corvallis, Oregon 3Division of Pulmonary, Allergy, and Rheumatology Products, Office of Drug Evaluation II, Center for Drug Evaluation and Research, US Food and Drug Administration, Silver Spring, Maryland Received 28 March 2013; revised 3 July 2013; accepted 9 July 2013 Published online 5 August 2013 in Wiley Online Library (wileyonlinelibrary.com). DOI 10.1002/jps.23689 ABSTRACT: Inhaled and intranasal corticosteroids (ICS and INS) are among the mainstays of the treatment for asthma and allergic rhinitis, respectively, and also carry the potential to suppress the hypothalamic–pituitary–adrenal (HPA) axis. Several important factors affect the interpretability of trials investigating the impact of ICS and INS on the HPA axis. This paper reviews 106 published clinical trials, peer-reviewed articles, and New Drug Application reviews of approved ICS and INS, using MEDLINE and Drugs@FDA database. The trials included in this review evaluated the potential impact on HPA axis function of eight approved single-ingredient ICS and INS (beclomethasone dipropionate, budesonide, ciclesonide, flunisolide, fluticasone furoate, flucticasone propionate, mometasone furoate, and triamcinolone acetonide) and combination products containing these ingredients. The most commonly utilized design was blinded, placebo controlled, and short term (<6 weeks) for adult trials and blinded, placebo controlled, and long term (≥6 weeks) for pediatric trials. -

Market Characterization of the U.S. Metered Dose Inhaler Industry
Market Characterization of the U.S. Metered Dose Inhaler Industry Prepared for: Stratospheric Protection Division Office of Air and Radiation U.S. Environmental Protection Agency Washington, D.C. 20460 Prepared by: ICF 2550 S Clark St. Suite 1200 Arlington, VA 22202 September 2021 Table of Contents 1. Summary ......................................................................................................................... 1 2. Introduction ..................................................................................................................... 1 3. Market Characterization .................................................................................................. 2 3.1. Overview of MDI Products ........................................................................................ 2 3.2. Major Manufacturers ................................................................................................ 2 4. Subsector Background and HFC Use .............................................................................. 4 4.1. Propellants in Medical Inhalers ................................................................................. 4 4.2. Current and Projected Sales of HFC MDIs ............................................................... 7 4.3. Imports and Exports of MDI Products in the United States ......................................11 5. References .....................................................................................................................13 Appendix A: Analysis of the DPI -

COPD/Asthma Class Update
Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35, Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 © Copyright 2012 Oregon State University. All Rights Reserved Class Update: Asthma/COPD Medications Month/Year of Review: July 2014 Last Oregon Review: May 2012/November 2013 PDL Classes: Asthma Controller, Asthma Rescue, COPD Source Documents: OSU College of Pharmacy New drug(s): Anoro® Ellipta® (umeclidinium/vilanterol) Manufacturer: GSK/Theravance Dossier Received: Yes Current Status of PDL Classes: Chronic Obstructive Pulmonary Disease (COPD): Preferred Agents: IPRATROPIUM BROMIDE HFA AER AD, IPRATROPIUM BROMIDE SOLUTION, IPRATROPIUM/ALBUTEROL SULFATE AMPUL-NEB, TIOTROPIUM BROMIDE(SPIRIVA®) CAP W/DEV, IPRATROPIUM/ALBUTEROL (COMBIVENT®) RESPIMAT Non-Preferred Agents: AFORMOTEROL (BROVANA®), FORMOTEROL (PERFOROMIST), ROFLUMILAST (DALIRESP®), INDACATEROL (ARCAPTA®) NEOHALER, ACLIDINIUM (TUDORZA®) PRESSAIR, VILANTEROL/FLUTICASONE (BREO®) ELLIPTA Asthma Controllers and Asthma Rescue Preferred Agents: BECLOMETHASONE DIPROPIONATE(QVAR®), BUDESONIDE (PULMICORT FLEXHALER®), BUDESONIDE / FORMOTEROL FUMARATE (SYMBICORT®), FLUTICASONE PROPIONATE(FLOVENT HFA®), FLUTICASONE PROPIONATE(FLOVENT DISKUS®), FLUTICASONE/SALMETEROL(ADVAIR DISKUS®), FLUTICASONE/SALMETEROL(ADVAIR HFA®), FORMOTEROL (FORADIL®) AEROLIZER, MONTELUKAST SODIUM TAB CHEW/TABLET, SALMETEROL XINAFOATE (SEREVENT®), ALBUTEROL SULFATE SOLUTION/VIAL NEBS, PIRBUTEROL ACETATE, PROAIR® HFA, VENTOLIN® HFA Non-preferred Agents: CICLESONIDE -

Nasal Steroids C4730-A
Prior Authorization Criteria Nasal Steroids Policy Number: C4730-A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 03/2012 7/29/2020 7/29/2021 LAST P&T J CODE TYPE OF CRITERIA APPROVAL/VERSION Q4 2020 3490 (NOC) RxPA 20201028C4730-A PRODUCTS AFFECTED: Flonase Sensimist (fluticasone furoate), Flunisolide, Qnasl (beclomethasone), Nasonex (mometasone), Omnaris (ciclesonide), Zetonna (ciclesonide), Beconase AQ (beclomethasone), Xhance (fluticasone propionate), Rhinocort (budesonide) DRUG CLASS: Nasal Steroids ROUTE OF ADMINISTRATION: Intranasal PLACE OF SERVICE: Retail Pharmacy The recommendation is that medications in this policy will be for pharmacy benefit coverage and member self-administered AVAILABLE DOSAGE FORMS: 24 HR NASAL SPR ALLERGY, ALLER-FLO SPR 50MCG, ALLERGY RELF SPR 50MCG, BECONASE AQ SPR 42MCG, BUDESONIDE SPR NASAL BUDESONIDE SPR NASALOTC, BUDESONIDE SUS 32MCG, CLARISPRAY SPR 50MCG FLONASE ALGY SPR 50MCG, FLONASE SENS SPR 27.5MCG, FLONASE-OTC SPR 50MCG FLONASE-RX SPR 50MCG120, FLUNISOLIDE SPR 0.025%, FLUTICASONE SPR 50MCG FLUTICASONE SPR 50MCGOTC, MOMETASONE SPR 50MCG, NASACORT ALR SPR 55MCG/AC, NASACORT ALR SPR 55MCGOTC, NASAL ALLGY SPR 55MCG/AC, NASALIDE INH SPR 0.025%, NASONEX SPR 50MCG, OMNARIS SPR NASAL, PROPEL IMP 370MCG, QNASL CHILD SPR 40MCG, QNASL SPR 80MCG, RA NASAL SPR ALLERGY, RHINOCORT SPR ALRGYOTC, RHINOCORT SPR AQUA, TRIAMCINOLON AER 55MCGOTC, VERAMYST NSL SPR 27.5MCG, XHANCE SPR 93MCG, ZETONNA AER 37MCG FDA-APPROVED USES: Allergic rhinitis; Seasonal and perennial, Non-allergic rhinitis XHANCE/NASONEX/RHINOCORT ONLY- nasal polyp treatment, QNASL/BECONASE AQ ONLY- prophylaxis of nasal polyp recurrence following surgical removal COMPENDIAL APPROVED OFF-LABELED USES: COVERAGE CRITERIA: INITIAL AUTHORIZATION DIAGNOSIS: Molina Healthcare, Inc. -

Therapeutic Class Overview Intranasal Corticosteroids
Therapeutic Class Overview Intranasal Corticosteroids Therapeutic Class Overview/Summary: Intranasal corticosteroids are primarily used to treat perennial and seasonal allergic rhinitis and may be useful in the treatment of some forms of nonallergic rhinitis.1-9 Symptoms typically associated with allergic rhinitis include nasal congestion, rhinorrhea, sneezing and/or nasal itching. These symptoms result from a complex allergen driven mucosal inflammation caused by interplay between resident and infiltrating inflammatory cells and a number of vasoactive and proinflammatory mediators.10 Intranasal corticosteroids downregulate the inflammatory response by binding to the intracellular glucocorticoid receptors of inflammatory cells and causing a conformational change, thereby controlling the rate of protein synthesis and suppressing the transcription of cytokine and chemokine genes.11 Continuous administration of intranasal corticosteroids is more efficacious than as-needed dosing, and the onset of therapeutic effect occurs between three and twelve hours.10 As a result of the route of administration and the relatively low systemic bioavailability of these agents, intranasal corticosteroids are generally not associated with any clinically significant systemic side effects. Drug interactions are limited when administered at recommended doses. The most common side effects include nasal irritation and mild epistaxis.1-9 Triamcinolone (Nasacort AQ®), mometasone (Nasonex®) and fluticasone furoate (Veramyst®) are Food and Drug Administration (FDA) approved for use in children two years of age and older and fluticasone propionate (Flonase®) is FDA-approved for use in children four years of age and older. Beclomethasone (Beconase AQ®), budesonide (Rhinocort Aqua®), ciclesonide (Omnaris®), and flunisolide are FDA-approved for use in children six years of age and older.