Well-Differentiated Spindle Cell Liposarcoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

TERT Promoter Mutations Occur Frequently in Gliomas and a Subset of Tumors Derived from Cells with Low Rates of Self-Renewal
TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal Patrick J. Killelaa,1, Zachary J. Reitmana,1, Yuchen Jiaob,1, Chetan Bettegowdab,c,1, Nishant Agrawalb,d, Luis A. Diaz, Jr.b, Allan H. Friedmana, Henry Friedmana, Gary L. Galliac,d, Beppino C. Giovanellae, Arthur P. Grollmanf, Tong-Chuan Heg, Yiping Hea, Ralph H. Hrubanh, George I. Jalloc, Nils Mandahli, Alan K. Meekerh,m, Fredrik Mertensi, George J. Nettoh,l, B. Ahmed Rasheeda, Gregory J. Rigginsc, Thomas A. Rosenquistf, Mark Schiffmanj, Ie-Ming Shihh, Dan Theodorescuk, Michael S. Torbensonh, Victor E. Velculescub, Tian-Li Wangh, Nicolas Wentzensenj, Laura D. Woodh, Ming Zhangb, Roger E. McLendona, Darell D. Bignera, Kenneth W. Kinzlerb, Bert Vogelsteinb,2, Nickolas Papadopoulosb, and Hai Yana,2 aThe Preston Robert Tisch Brain Tumor Center at Duke, Pediatric Brain Tumor Foundation Institute at Duke, and Department of Pathology, Duke University Medical Center, Durham, NC 27710; bLudwig Center for Cancer Genetics and Howard Hughes Medical Institutions, Johns Hopkins Kimmel Cancer Center, Johns Hopkins Medical Institutions, Baltimore, MD 21231; Departments of cNeurosurgery, dOtolaryngology—Head and Neck Surgery, hPathology, lUrology, and mOncology, Johns Hopkins University School of Medicine, Baltimore, MD 21231; eChristus Stehlin Foundation for Cancer Research, Houston, TX 77025; fDepartment of Pharmacological Sciences, Stony Brook University, Stony Brook, NY 11794; gMolecular Oncology Laboratory, Department of Orthopaedic -
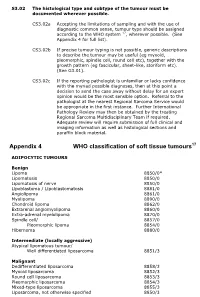
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Pleomorphic Lipoma: a Rare Tumor in the Retropharyngeal Space Pleomorphic Lipoma: a Rare Tumor in the Retropharyngeal Space
AIJOC 10.5005/jp-journals-10003-1141 CASE REPORT Pleomorphic Lipoma: A Rare Tumor in the Retropharyngeal Space Pleomorphic Lipoma: A Rare Tumor in the Retropharyngeal Space Vidya Bhushan Rangappa, Raghavendra Suresh, Kapila Manikantan, AM Balasubramanya ABSTRACT well encapsulated, hypodense lesion in the retropharyngeal Lipomas are benign tumors arising from fat cells. Occurrence space extending into right parapharyngeal space pushing of lipoma in retropharyngeal space is very rare entity. To the larynx and pharynx to left and displacement of right great best of our knowledge, this is the second case of pleomorphic vessels laterally (Fig. 2). The lesion was seen extending lipoma being reported in the retropharyngeal space. They are from skull base to upper mediastinum. Fine needle aspiration usually asymptomatic until they are of large size. We report a case of a large pleomorphic lipoma in the retropharyngeal space, cytology (FNAC) of the lesion was consistent with features with emphasis on the clinical characters and histologic of lipoma. Surgically the mass was removed with a extended characteristics of the lesion. These tumors are best managed thyroidectomy incision extending from right mastoid tip surgically by a transcervical approach. down to left lateral part of the neck. Mass was dissected Keywords: Pleomorphic, Retropharyngeal space, Lipoma, from the surrounding structures completely with the capsule Benign, Neck swelling. (Figs 3 and 4). The mass was measuring 8 × 6 cm (Fig. 5). How to cite this article: Rangappa VB, Suresh R, Manikantan Histopathological examination showed characteristic K, Balasubramanya AM. Pleomorphic Lipoma: A Rare Tumor in 'floret' cells which are large hyperchromatic multinucleated the Retropharyngeal Space. -

Spindle Cell Liposarcoma with a TRIO-TERT Fusion Transcript
Virchows Archiv (2019) 475:391–394 https://doi.org/10.1007/s00428-019-02545-5 BRIEF REPORTS Spindle cell liposarcoma with a TRIO-TERT fusion transcript David I. Suster1 & Vikram Deshpande1 & Ivan Chebib1 & Martin S. Taylor1 & John Mullen2 & Miriam A. Bredella3 & G. Petur Nielsen1 Received: 7 January 2019 /Revised: 8 February 2019 /Accepted: 11 February 2019 /Published online: 22 February 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Conventional well-differentiated, dedifferentiated, and myxoid liposarcomas have long been known to harbor numerous typical genetic alterations that allow for diagnosis of these tumors. These include MDM2 and CDK4 amplification in well-differentiated and dedifferentiated liposarcomas as well as FUS-DDIT3 rearrangements in myxoid liposarcoma. More recently, in-frame TRIO- TERT fusion genes have been described in a subset of non-translocation-related sarcomas including myxofibrosarcoma, dedifferentiated liposarcoma, undifferentiated pleomorphic sarcoma, pleomorphic rhabdomyosarcoma, and leiomyosarcoma. These genetic rearrangements lead to TERT mRNA expression levels hundreds of times higher than normal, causing increased telomerase activation in these tumors. Herein, we describe an unusual case of a liposarcoma with spindle cell features and a TRIO-TERT fusion transcript identified through next-generation sequencing. Keywords Liposarcoma . TRIO-TERT . Fusion transcript The current classification of spindle cell lipomatous neoplasms Recently, a novel in-frame TRIO-TERT fusion has been is still evolving. In the literature, the term Bspindle cell identified in some non-translocation-related sarcomas [6]. liposarcoma^ has been used to describe many tumors including TRIO plays an important role in cell adhesion and nuclear spindled variants of well-differentiated liposarcoma and signaling pathways and is part of a family of Rho GTPases myxoid liposarcoma, as well as spindle cell lipomas with that act as guanine nucleotide exchange factors [7]. -

Spindle Cell Lipoma of the Anterior Triangle of the Neck
Braz J Otorhinolaryngol. 2011;77(3):401. CASE REPORT BJORL .org Spindle cell lipoma of the anterior triangle of the neck: a rare entity Smita Upadhyay1, Arpit Sharma2, Shashikant Mhashal3, Jyoti P Dabholkar4 Keywords: immunohistochemistry, lipoma, neck. INTRODUCTION involves the elderly males. Most common both of these have similar cytogenetics they locations involve the posterior neck, shoulder are considered as a single entity 5. Solitary lipomas are the most common and back however in our case the anterior It is important to differentiate SCL from soft tissue tumor. Lipomas include a gamut triangle of the neck were involved. liposarcoma. Liposarcoma are characterized of subtypes. Spindle cell lipoma (SCL) is a by more numerous spindle cells, presence of distinct entity accounting for about 1.5% of nuclear pleomorphism and MDM-2 amplifica- all lipomas1. The diagnosis of SCL is a his- tion1. Myxoid stroma can sometimes be seen tological one and careful study is required to in SCL when it mimics myxoid liposarcomas. differentiate it from the liposarcoma. However the superficial location and the circumscribed lesion helps differentiate SCL CASE REPORT from the latter. Also the vascular pattern, pleomorphism and mitotic activity should A 48 year old male reported with a be assessed6. The other differential diagnosis history of a left sided neck swelling since 2 includes dermatofibrosarcoma protuberans, years which was progressively increasing in mammary type solitary fibrous tumor and size. A 4x4 cm swelling was present in the an- myofibroblastoma. terior triangle of the neck which was firm and The treatment is surgical excision mobile. ENT examination and investigations and recurrences are extremely rare even with were unremarkable. -

Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy
ANTICANCER RESEARCH 35: 5717-5736 (2015) Review Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy MICHAEL KOCH1, ANNE J. FREUNDL2, ABBAS AGAIMY3, FRANKLIN KIESEWETTER2, JULIAN KÜNZEL4, IWONA CICHA1* and CHRISTOPH ALEXIOU1* 1Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital Erlangen, Erlangen, Germany; 2Dermatology Clinic, 3Institute of Pathology, and 4ENT Department, University Hospital Mainz, Mainz, Germany Abstract. Background: Atypical fibroxanthoma (AFX) is an in 1962 (2). The name 'atypical fibroxanthoma' reflects the uncommon, rapidly growing cutaneous neoplasm of uncertain tumor composition, containing mainly xanthomatous-looking histogenesis. Thus far, there are no guidelines for diagnosis and cells and a varying proportion of fibrocytoid cells with therapy of this tumor. Patients and Methods: We included 18 variable, but usually marked cellular atypia (3). patients with 21 AFX, and 2,912 patients with a total of 2,939 According to previous reports, AFX chiefly occurs in the AFX cited in the literature between 1962 and 2014. Results: In sun-exposed head-and-neck area, especially in elderly males our cohort, excision with safety margin was performed in 100% (3). There are two disease peaks described: one within the 5th of primary tumors. Local recurrences were observed in 25% of to 7th decade of life and another one between the 7th and 8th primary tumors and parotid metastases in 5%. Ten-year disease- decade. The former disease peak is associated with lower specific survival was 100%. The literature research yielded 280 tumor frequency (21.8%) and tumors that do not necessarily relevant publications. Over 90% of the reported cases were manifest on skin areas exposed to sunlight (4). -

Pleural Mesothelioma Dilated and the Pulmonary Trunk Was Occluded by a Large Embolus
Thorax 1993;48:409-410 409 lungs showed fibrosis, subpleural honeycomb Liposarcomatous changes, chronic bronchitis, and foci of bron- chopneumonia. The heart was slightly differentiation in diffuse enlarged (weight 430 g, right ventricle 120 g, left ventricle 230 g). The right side was Thorax: first published as 10.1136/thx.48.4.409 on 1 April 1993. Downloaded from pleural mesothelioma dilated and the pulmonary trunk was occluded by a large embolus. The left atrium J Krishna, M T Haqqani was occupied by a large myxoid tumour mass measuring 15 x 6 cm attached to a blood clot which extended into the pulmonary veins. The rest of the organs showed no abnor- Abstract malities. A case history is presented of a woman who died eight hours after hospital MICROSCOPICAL APPEARANCES admission with severe breathlessness. At The right pleura was diffusely infiltrated by necropsy the right lung was encased in a the tumour, which showed a sarcomatous thickened pleura with a large tumour. pattern with myxoid change and abundant Histological examination of the tumour typical lipoblasts containing sharply defined showed pleural mesothelioma with cytoplasmic vacuoles indenting hyperchro- liposarcomatous differentiation. The matic nuclei in the right upper lobe. This was lungs showed changes of asbestosis and confirmed on the electron microscope after the asbestos fibre count was significandy the tissue was post fixed in osmium tetraoxide raised. Liposarcomatous differentiation (fig 1). The right upper lobe also showed an in pleural mesothelioma has not been adjacent mesothelioma with an epithelial reported previously. glandular component (fig 2), uniformly nega- tive for carcinoembryonic antigen but (Thorax 1993;48:409-410) strongly positive for epithelial membrane antigen and cytokeratin. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -
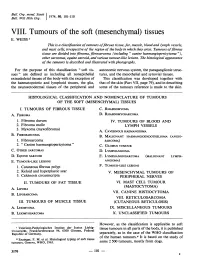
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -
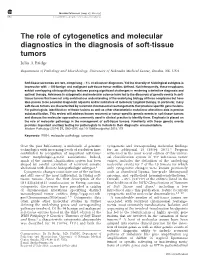
The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events