Pleomorphic Lipoma • Chondroid Lipoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medical Directors Arup Medical Directors and Consulting Faculty | 2015
MEDICAL DIRECTORS ARUP MEDICAL DIRECTORS AND CONSULTING FACULTY | 2015 MAY 2015 www.aruplab.com Information in this brochure is current as of May 2015. All content is subject to change. Please contact ARUP Client Services at (800) 522-2787 with any questions or concerns. ARUP LABORATORIES ARUP Laboratories is a national clinical and anatomic pathology reference laboratory and a nonprofit enterprise of the University of Utah and its Department of Pathology. Located in Salt Lake City, Utah, ARUP offers in excess of 3,000 tests and test combinations, ranging from routine screening tests to esoteric molecular and genetic assays. Rather than competing with its clients for physician office business, ARUP chooses instead to support clients’ existing test menus by offering complex and unique tests, with accompanying consultative support, to enhance their abilities to provide local and regional laboratory services. ARUP’s clients include many of the nation’s university teaching hospitals and children’s hospitals, as well as multihospital groups, major commercial laboratories, group purchasing organizations, military and other government facilities, and major clinics. In addition, ARUP is a worldwide leader in innovative laboratory research and development, led by the efforts of the ARUP Institute for Clinical and Experimental Pathology®. Since its formation in 1984 by the Department of Pathology at the University of Utah, ARUP has founded its reputation on reliable and consistent laboratory testing and service. This simple strategy contributes significantly to client satisfaction. When ARUP conducts surveys, clients regularly rate ARUP highly and respond that they would recommend ARUP to others. As the most responsive source of quality information and knowledge, ARUP strives to be the reference laboratory of choice for community healthcare systems. -
Rare Skin Cancers in General Practice
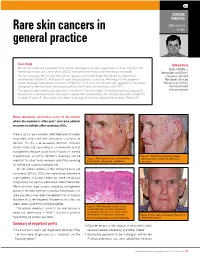
CLINICAL PRACTICE Skin cancer Rare skin cancers in series general practice Case study Anthony Dixon Mr LA has long been troubled with actinic damage to his skin, especially his face. He has had MBBS, FACRRM, is many squamous cell carcinomas (SCCs) removed and many solar keratoses managed. dermasurgeon and Director On this occasion Mr LA had two actinic lesions on his left cheek that failed to respond to of Research, Skin Alert cryotherapy (Figure 1). A biopsy of each site produced a surprise. Histology of the superior Skin Cancer Clinics and lesion revealed sebaceous carcinoma (Figure 2). This is an uncommon yet aggressive cutaneous Skincanceronly, Belmont, malignancy derived from sebaceous glands. The 5 year survival rate is 60–70%. Victoria. anthony@ The tumour was widely excised with a minimum 10 mm margin. A multidisciplinary approach skincanceronly.com resulted in a decision not to proceed to adjunctive radiotherapy. The wound was well healed by 8 weeks (Figure 3). Four years on there is no sign of local or regional recurrence (Figure 4). Many sebaceous carcinomas occur on the eyelids where the outcome is often poor;1 and some patients are prone to multiple other cutaneous SCCs. There is also a rare syndrome called Muir-torre of visceral neoplasms associated with sebaceous carcinoma on the skin.2 As this is an autosomal dominant condition, family history and counselling is an esssential part of management (enquire about family history of internal malignancies). A family member's diagnosis can be Figure 3. Satisfactory healing 8 weeks Figure 1. Two actinic lesions on the left face following wide excision of sebaceous important for other family members and offers screening have failed to respond to cryotherapy carcinoma for internal and cutaneous malignancies. -

Atypical Compound Nevus Arising in Mature Cystic Ovarian Teratoma
J Cutan Pathol 2005: 32: 71–123 Copyright # Blackwell Munksgaard 2005 Blackwell Munksgaard. Printed in Denmark Journal of Cutaneous Pathology Abstracts of the Papers Presented at the 41st Annual Meeting of The American Society of Dermatopathology Westin Copley Place Boston, Massachusetts, USA October 14–17, 2004 These abstracts were presented in oral or poster format at the 41st Annual Meeting of The American Society of Dermatopathology on October 14–17, 2004. They are listed on the following pages in alphabetical order by the first author’s last name. 71 Abstracts IN SITU HYBRIDIZATION IS A VALUABLE DIAGNOSTIC A 37-year-old woman with diagnosis of Sjogren’s syndrome (SS) TOOL IN CUTANEOUS DEEP FUNGAL INFECTIONS presented with asymptomatic non-palpable purpura of the lower J.J. Abbott1, K.L. Hamacher2,A.G.Bridges2 and I. Ahmed1,2 extremities. Biopsy of a purpuric macule revealed a perivascular Departments of Laboratory Medicine and Pathology1 and and focally nodular lymphocytic infiltrate with large numbers of Dermatology2, plasma cells, seemingly around eccrine glands. There was no vascu- litis. The histologic findings in the skin were strikingly similar to those Mayo Clinic and Mayo Foundation, Rochester, MN, USA of salivary, parotid, and other ‘‘secretory’’ glands affected in SS. The cutaneous manifestations of SS highlighted in textbooks include Dimorphic fungal infections (histoplasmosis, blastomycosis, coccidiomy- xerosis, annular erythema, small-vessel vasculitis, and pigmented cosis, and cryptococcosis) can occur in immunocompromised and purpura. This case illustrates that purpura in skin of patients with healthy individuals. Cutaneous involvement is often secondary and SS may be caused by a peri-eccrine plasma-rich infiltrate. -

A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated Through 445 Nm Diode Laser
healthcare Case Report A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated through 445 nm Diode Laser Maria Vittoria Viani 1,*, Luigi Corcione 1, Chiara Di Blasio 2, Ronell Bologna-Molina 3 , Paolo Vescovi 1 and Marco Meleti 1 1 Department of Medicine and Surgery, University of Parma, 43126 Parma, Italy; [email protected] (L.C.); [email protected] (P.V.); [email protected] (M.M.) 2 Private practice, Centro Medico Di Blasio, 43121 Parma; Italy; [email protected] 3 Faculty of Dentistry, University of the Republic, 14600 Montevideo, Uruguay; [email protected] * Correspondence: [email protected] Received: 10 June 2020; Accepted: 11 August 2020; Published: 13 August 2020 Abstract: Oral granular cell tumor (GCT) is a relatively rare, benign lesion that can easily be misdiagnosed. Particularly, the presence of pseudoepitheliomatous hyperplasia might, in some cases, lead to the hypothesis of squamous cell carcinoma. Surgical excision is the treatment of choice. Recurrence has been reported in up to 15% of cases treated with conventional surgery. Here, we reported a case of GCT of the tongue in a young female patient, which was successfully treated through 445 nm diode laser excision. Laser surgery might reduce bleeding and postoperative pain and may be associated with more rapid healing. Particularly, the vaporization effect on remnant tissues could eliminate GCT cells on the surgical bed, thus hypothetically leading to a lower rate of recurrence. In the present case, complete healing occurred in 1 week, and no recurrence was observed after 6 months. Laser surgery also allows the possibility to obtain second intention healing. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Understanding Your Pathology Report: Benign Breast Conditions
cancer.org | 1.800.227.2345 Understanding Your Pathology Report: Benign Breast Conditions When your breast was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. Information in this report will be used to help manage your care. The questions and answers that follow are meant to help you understand medical language you might find in the pathology report from a breast biopsy1, such as a needle biopsy or an excision biopsy. In a needle biopsy, a hollow needle is used to remove a sample of an abnormal area. An excision biopsy removes the entire abnormal area, often with some of the surrounding normal tissue. An excision biopsy is much like a type of breast-conserving surgery2 called a lumpectomy. What does it mean if my report uses any of the following terms: adenosis, sclerosing adenosis, apocrine metaplasia, cysts, columnar cell change, columnar cell hyperplasia, collagenous spherulosis, duct ectasia, columnar alteration with prominent apical snouts and secretions (CAPSS), papillomatosis, or fibrocystic changes? All of these are terms that describe benign (non-cancerous) changes that the pathologist might see under the microscope. They do not need to be treated. They are of no concern when found along with cancer. More information about many of these can be found in Non-Cancerous Breast Conditions3. What does it mean if my report says fat necrosis? Fat necrosis is a benign condition that is not linked to cancer risk. -

Well-Differentiated Spindle Cell Liposarcoma
Modern Pathology (2010) 23, 729–736 & 2010 USCAP, Inc. All rights reserved 0893-3952/10 $32.00 729 Well-differentiated spindle cell liposarcoma (‘atypical spindle cell lipomatous tumor’) does not belong to the spectrum of atypical lipomatous tumor but has a close relationship to spindle cell lipoma: clinicopathologic, immunohistochemical, and molecular analysis of six cases Thomas Mentzel1, Gabriele Palmedo1 and Cornelius Kuhnen2 1Dermatopathologie, Friedrichshafen, Germany and 2Institute of Pathology, Medical Center, Mu¨nster, Germany Well-differentiated spindle cell liposarcoma represents a rare atypical/low-grade malignant lipogenic neoplasm that has been regarded as a variant of atypical lipomatous tumor. However, well-differentiated spindle cell liposarcoma tends to occur in subcutaneous tissue of the extremities, the trunk, and the head and neck region, contains slightly atypical spindled tumor cells often staining positively for CD34, and lacks an amplification of MDM2 and/or CDK4 in most of the cases analyzed. We studied a series of well-differentiated spindle cell liposarcomas arising in two female and four male patients (age of the patients ranged from 59 to 85 years). The neoplasms arose on the shoulder, the chest wall, the thigh, the lower leg, the back of the hand, and in paratesticular location. The size of the neoplasms ranged from 1.5 to 10 cm (mean: 6.0 cm). All neoplasms were completely excised. The neoplasms were confined to the subcutis in three cases, and in three cases, an infiltration of skeletal muscle was seen. Histologically, the variably cellular neoplasms were composed of atypical lipogenic cells showing variations in size and shape, and spindled tumor cells with slightly enlarged, often hyperchromatic nuclei. -

Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Subcutaneous Hemangiosarcoma: the First Report in Maltese Dog
pISSN 1598-298X / eISSN 2384-0749 J Vet Clin 36(3) : 169-171 (2019) http://dx.doi.org/10.17555/jvc.2019.06.36.3.169 Subcutaneous Hemangiosarcoma: The First Report in Maltese Dog Ha-Jung Kim, Eun-Taek Hong and Guk-Hyun Suh1 Department of Veterinary Internal Medicine, College of Veterinary Medicine, Chonnam National University, Gwangju 500-757, Korea (Received: March 13, 2019 / Accepted: May 09, 2019) Abstract : Subcutanous hemangiosarcoma is rare malignant condition in dogs. An eleven-year-old neutered male Maltese was presented with multicentric cutaneous hemorrhagic nodules followed by lethargy. The patient showed regenerative anemia and thrombocytopenia with skyrocketing D-dimer, indicating that he had disseminated intravascular coagulation (DIC) on progress. Fine needle aspiration, histopathology, X-ray, and computed tomographic scanning ultimately diagnosed this patient as subcutaneous hemangiosarcoma with disseminated metastasis to the body. Unfortunately, the dog died due to side effects of anti-thrombotic therapy for DIC. This case report described a rare subcutaneous hemangiosarcoma in a Maltese dog. Key words : dog, skin neoplasms, hemangiosarcoma, disseminated intravascular coagulation, histopathology. Introduction had a 2 month history of multicentric cutaneous hemor- rhagic nodules initiated from his dorsum (Fig 1A and C). Hemangiosarcoma (a.k.a. malignant hemangioendotheli- There were no specific findings from skin examination such oma or angisarcoma) is an outbreak of tumor from endothe- as scraping or taping, and no bacteria or fungi were cultured lial cells which occurs more frequently in dogs than any from the lesions. On physical examination, he had a pale other species, accounting for 0.3% to 2.0% of all tumors in mucous membrane with bilateral ocular hemorrhage (Fig dogs with a high fatality rate (1,7). -

Pleomorphic Lipoma: a Rare Tumor in the Retropharyngeal Space Pleomorphic Lipoma: a Rare Tumor in the Retropharyngeal Space
AIJOC 10.5005/jp-journals-10003-1141 CASE REPORT Pleomorphic Lipoma: A Rare Tumor in the Retropharyngeal Space Pleomorphic Lipoma: A Rare Tumor in the Retropharyngeal Space Vidya Bhushan Rangappa, Raghavendra Suresh, Kapila Manikantan, AM Balasubramanya ABSTRACT well encapsulated, hypodense lesion in the retropharyngeal Lipomas are benign tumors arising from fat cells. Occurrence space extending into right parapharyngeal space pushing of lipoma in retropharyngeal space is very rare entity. To the larynx and pharynx to left and displacement of right great best of our knowledge, this is the second case of pleomorphic vessels laterally (Fig. 2). The lesion was seen extending lipoma being reported in the retropharyngeal space. They are from skull base to upper mediastinum. Fine needle aspiration usually asymptomatic until they are of large size. We report a case of a large pleomorphic lipoma in the retropharyngeal space, cytology (FNAC) of the lesion was consistent with features with emphasis on the clinical characters and histologic of lipoma. Surgically the mass was removed with a extended characteristics of the lesion. These tumors are best managed thyroidectomy incision extending from right mastoid tip surgically by a transcervical approach. down to left lateral part of the neck. Mass was dissected Keywords: Pleomorphic, Retropharyngeal space, Lipoma, from the surrounding structures completely with the capsule Benign, Neck swelling. (Figs 3 and 4). The mass was measuring 8 × 6 cm (Fig. 5). How to cite this article: Rangappa VB, Suresh R, Manikantan Histopathological examination showed characteristic K, Balasubramanya AM. Pleomorphic Lipoma: A Rare Tumor in 'floret' cells which are large hyperchromatic multinucleated the Retropharyngeal Space. -

Simple Technique to Identify Haemosiderin in Immunoperoxidase Stained Sections
J Clin Pathol: first published as 10.1136/jcp.37.10.1190 on 1 October 1984. Downloaded from 1190 Technical methods Phosphate buffer at pH 8*0 gave the sharpest 2 Rozenszajn L, Leibovich M, Shoham D, Epstein J. The esterase staining reactions, although there was little differ- activity in megaloblasts, leukaemic and normal haemopoietic cells. Br J Haematol 1968; 14:605-19. ence at pH 7-0 or pH 7-5. As the buffer pH was 3Hayhoe FGJ, Quaglino D. Haematological cytochemistry. Edin- increased above pH 8-0 staining with both substrates burgh: Churchill Livingstone, 1980. became progressively weaker, especially above pH 4Li CY, Lam KW, Yam LT. Esterases in human leucocytes. J 9.0. Below pH 7-0 staining with a-naphthyl butyrate Histochem Cytochem 1973;21:1-12. Yam LT, Li CY, Crosby WH. Cytochemical identification of became weaker, and below pH 5*0 staining with monocytes and granulocytes. Am J Clin Pathol 1971;55:283- naphthol AS-D chloroacetate began to disappear. 90. 6 Armitage RJ, Linch DC, Worman CP, Cawley JC. The morphol- This work was supported by a Medical Research ogy and cytochemistry of human T-cell subpopulations defined by monoclonal antibodies and Fc receptors. Br J Haematol Council project grant. I thank Professor FGJ 1983;51:605-13. Hayhoe for valuable advice. References Requests for reprints to: Dr DM Swirsky, Department of Gomori G. Chloroacyl esters as histochemical substrates. J His- Haematological Medicine, University Clinical School, Hills tochem Cytochem 1953;1:469-70. Road, Cambridge CB2 2QL, England. Simple technique to identify identification of the two compounds on the same haemosiderin in slide. -

Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy
ANTICANCER RESEARCH 35: 5717-5736 (2015) Review Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy MICHAEL KOCH1, ANNE J. FREUNDL2, ABBAS AGAIMY3, FRANKLIN KIESEWETTER2, JULIAN KÜNZEL4, IWONA CICHA1* and CHRISTOPH ALEXIOU1* 1Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital Erlangen, Erlangen, Germany; 2Dermatology Clinic, 3Institute of Pathology, and 4ENT Department, University Hospital Mainz, Mainz, Germany Abstract. Background: Atypical fibroxanthoma (AFX) is an in 1962 (2). The name 'atypical fibroxanthoma' reflects the uncommon, rapidly growing cutaneous neoplasm of uncertain tumor composition, containing mainly xanthomatous-looking histogenesis. Thus far, there are no guidelines for diagnosis and cells and a varying proportion of fibrocytoid cells with therapy of this tumor. Patients and Methods: We included 18 variable, but usually marked cellular atypia (3). patients with 21 AFX, and 2,912 patients with a total of 2,939 According to previous reports, AFX chiefly occurs in the AFX cited in the literature between 1962 and 2014. Results: In sun-exposed head-and-neck area, especially in elderly males our cohort, excision with safety margin was performed in 100% (3). There are two disease peaks described: one within the 5th of primary tumors. Local recurrences were observed in 25% of to 7th decade of life and another one between the 7th and 8th primary tumors and parotid metastases in 5%. Ten-year disease- decade. The former disease peak is associated with lower specific survival was 100%. The literature research yielded 280 tumor frequency (21.8%) and tumors that do not necessarily relevant publications. Over 90% of the reported cases were manifest on skin areas exposed to sunlight (4).