Vaccine Prior Authorization Change Effective January 1, 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RNA-Based Adjuvant CV8102 Enhances the Immunogenicity of a Licensed Rabies Vaccine in a first-In-Human Trial
Vaccine 37 (2019) 1819–1826 Contents lists available at ScienceDirect Vaccine journal homepage: www.elsevier.com/locate/vaccine RNA-based adjuvant CV8102 enhances the immunogenicity of a licensed rabies vaccine in a first-in-human trial Fatma Doener a,1, Henoch S. Hong a,1, Ingo Meyer b,1, Keyvan Tadjalli-Mehr c, Angelika Daehling c, ⇑ Regina Heidenreich a, Sven D. Koch a, Mariola Fotin-Mleczek a, Ulrike Gnad-Vogt c, a Curevac AG, Paul-Ehrlich-Strasse 15, 72076 Tübingen, Germany b CRS Clinical Research Services Mönchengladbach GmbH, 41061 Mönchengladbach, Germany c Curevac AG, Schumannstrasse 27, 60325 Frankfurt, Germany article info abstract Article history: Background: We report the first-in-concept human trial of the safety, tolerability and immunogenicity Received 27 September 2018 when a novel TLR 7/8/RIG I agonist RNA-based adjuvant, CV8102, was administered alone or mixed with Received in revised form 30 January 2019 fractional doses of a licensed rabies vaccine (RabipurÒ) as model antigen. Accepted 3 February 2019 Methods: The primary objective was to assess the safety and reactogenicity of various dose levels of Available online 21 February 2019 CV8102 alone or mixed with RabipurÒ in healthy 18–40 year-old male volunteers. A secondary objective was to assess the immune-enhancing potential of bedside-mixes of CV8102 with fractional doses of Keywords: Ò Rabipur by measuring induction of rabies virus neutralising titres (VNTs). Adjuvant Results: Fifty-six volunteers received 50–100 lg CV8102 alone (n = 11), bedside-mixed CV8102 and RNA Ò Ò Ò Rabies Rabipur (n = 20), or Rabipur alone (n = 25; control). -

USDA-Approved Animal Rabies Vaccines
United States Department of Agriculture (USDA) Approved Animal Rabies Vaccines Table 1. Rabies Vaccines Licensed and Marketed in the United States, 2016 Age at For use Route of Product Name Produced by Marketed by Dose primary Booster vaccination in inoculation vaccination* A) MONOVALENT (Inactivated) RAB RABVAC 1 Boehringer Boehringer Dogs 1 ml 3 months Annually IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months Annually IM or SC Vetmedica Inc Inc License No. 124 RABVAC 3 Boehringer Boehringer Dogs 1 ml 3 months 1 year later & triennially IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months 1 year later & triennially IM or SC Vetmedica Inc Inc Horses 2 ml 3 months Annually IM License No. 124 EQUIRAB with Merck Animal Merck Animal Health Horses 1 ml 4 months Annually IM Havlogen Health License No. 165A DEFENSOR 1 Zoetis Zoetis Dogs 1 ml 3 months Annually IM or SC License No. 190 Cats 1 ml 3 months Annually SC DEFENSOR 3 Zoetis Zoetis Dogs 1 ml 3 months 1 year later & triennially IM or SC License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM NOBIVAC: 1- Zoetis Merck Animal Health Dogs 1 ml 3 months Annually IM or SC Rabies License No. 190 Cats 1 ml 3 months Annually SC NOBIVAC: 3- Zoetis Merck Animal Health Dogs 1 ml 3 months 1 year later & triennially IM or SC Rabies and 3- License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Rabies CA Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM IMRAB 1 Merial, Inc Merial, Inc Dogs 1 ml 3 months Annually SC License No. -
A Guide to Vaccinations for Parents
A GUIDE TO VACCINATIONS FOR PARENTS What are vaccines? When should my child be vaccinated? Why does my child need the HPV vaccine? HISTORY OF VACCINATIONS Smallpox is a serious infectious disease that causes fever and a distinctive, progressive 600 1796 skin rash. years ago Edward Jenner developed Variolation, intentionally a vaccine against smallpox. Cases of paralysis from polio in the U.S. exposing an individual to Almost 200 years later, in 1980, in the early 1950s: smallpox material, traces back the World Health Organization more than to 16th-century China. This declared that smallpox process resulted in a milder had been eradicated, 15,000 form of the disease. or wiped out. In the year 2017: Childhood vaccines can prevent 14 potentially serious 0 diseases or conditions throughout your child’s lifetime. 1955 1940s 1885 Jonas Salk’s polio vaccine The routine immunization Louis Pasteur developed a was proven safe and effective. schedule included vaccines vaccine against rabies. The Polio has now been eliminated against four potentially serious rabies vaccine series, which in the U.S., and organizations diseases (smallpox, diphtheria, can be given to people who are currently working tetanus, and pertussis). may have been exposed to to eradicate polio Now the schedule includes the virus, has made rabies worldwide. vaccines to prevent a total infection very rare in the of 14 conditions. United States. In the U.S., vaccines go through three phases of clinical trials to make sure they are safe and effective before they are licensed. 2006 Today The HPV vaccine was Vaccine research licensed in the U.S. -

Dengue Fact Sheet
State of California California Department of Public Health Health and Human Services Agency Division of Communicable Disease Control Dengue Fact Sheet What is dengue? Dengue is a disease caused by any one of four closely related dengue viruses (DENV- 1, DENV-2, DENV-3, and DENV-4). Where does dengue occur? Dengue occurs in many tropical and sub-tropical areas of the world, particularly sub- Saharan Africa, the Middle East, Southeast Asia, and Central and South America. With the exception of Mexico, Puerto Rico, small areas in southern Texas and southern Florida, and some regions of Hawaii, dengue transmission does not occur in North America. Worldwide there are an estimated 50 to 100 million cases of dengue per year. How do people get dengue? People get dengue from the bite of an infected mosquito. The mosquito becomes infected when it bites a person who has dengue virus in their blood. It takes a week or more for the dengue organisms to mature in the mosquito; then the mosquito can transmit the virus to another person when it bites. Dengue is transmitted principally by Aedes aegypti (yellow fever mosquito) and Aedes albopictus (Asian tiger mosquito). These mosquitoes are not native to California, but infestations have been identified in multiple counties in California. Dengue virus cannot be transmitted from person to person. What are the symptoms of dengue? There are two types of illness that can result from infection with a dengue virus: dengue and severe dengue. The main symptoms of dengue are high fever, severe headache, severe pain behind the eyes, joint pain, muscle and bone pain, rash, bruising, and may include mild bleeding from the nose or mouth. -

Dengue and Yellow Fever
GBL42 11/27/03 4:02 PM Page 262 CHAPTER 42 Dengue and Yellow Fever Dengue, 262 Yellow fever, 265 Further reading, 266 While the most important viral haemorrhagic tor (Aedes aegypti) as well as reinfestation of this fevers numerically (dengue and yellow fever) are insect into Central and South America (it was transmitted exclusively by arthropods, other largely eradicated in the 1960s). Other factors arboviral haemorrhagic fevers (Crimean– include intercontinental transport of car tyres Congo and Rift Valley fevers) can also be trans- containing Aedes albopictus eggs, overcrowding mitted directly by body fluids. A third group of of refugee and urban populations and increasing haemorrhagic fever viruses (Lassa, Ebola, Mar- human travel. In hyperendemic areas of Asia, burg) are only transmitted directly, and are not disease is seen mainly in children. transmitted by arthropods at all. The directly Aedes mosquitoes are ‘peri-domestic’: they transmissible viral haemorrhagic fevers are dis- breed in collections of fresh water around the cussed in Chapter 41. house (e.g. water storage jars).They feed on hu- mans (anthrophilic), mainly by day, and feed re- peatedly on different hosts (enhancing their role Dengue as vectors). Dengue virus is numerically the most important Clinical features arbovirus infecting humans, with an estimated Dengue virus may cause a non-specific febrile 100 million cases per year and 2.5 billion people illness or asymptomatic infection, especially in at risk.There are four serotypes of dengue virus, young children. However, there are two main transmitted by Aedes mosquitoes, and it is un- clinical dengue syndromes: dengue fever (DF) usual among arboviruses in that humans are the and dengue haemorrhagic fever (DHF). -

Dengue Fever/Severe Dengue Fever/Chikungunya Fever! Report on Suspicion of Infection During Business Hours
Dengue Fever/Severe Dengue Fever/Chikungunya Fever! Report on suspicion of infection during business hours PROTOCOL CHECKLIST Enter available information into Merlin upon receipt of initial report Review background information on the disease (see Section 2), case definitions (see Section 3 for dengue and for chikungunya), and laboratory testing (see Section 4) Forward specimens to the Florida Department of Health (DOH) Bureau of Public Health Laboratories (BPHL) for confirmatory laboratory testing (as needed) Inform local mosquito control personnel of suspected chikungunya or dengue case as soon as possible (if applicable) Inform state Arbovirus Surveillance Coordinator on suspicion of locally acquired arbovirus infection Contact provider (see Section 5A) Interview case-patient Review disease facts (see Section 2) Mode of transmission Ask about exposure to relevant risk factors (see Section 5. Case Investigation) History of travel, outdoor activities, and mosquito bites two weeks prior to onset History of febrile illness or travel for household members or other close contacts in the month prior to onset History of previous arbovirus infection or vaccination (yellow fever, Japanese encephalitis) Provide education on transmission and prevention (see Section 6) Awareness of mosquito-borne diseases Drain standing water at least weekly to stop mosquitoes from multiplying Discard items that collect water and are not being used Cover skin with clothing or Environmental Protection Agency (EPA)-registered repellent such as DEET (N,N-diethyl-meta-toluamide) Use permethrin on clothing (not skin) according to manufacturer’s directions Cover doors and windows with intact screens to keep mosquitoes out of the house Enter additional data obtained from interview into Merlin (see Section 5D) Arrange for a convalescent specimen to be taken (if necessary) Dengue/Chikungunya Guide to Surveillance and Investigation Dengue Fever/Severe Dengue/Chikungunya 1. -

Mm7002e1 Allergic Reactions Including Anaphylaxis After Receipt
Morbidity and Mortality Weekly Report Early Release / Vol. 70 January 6, 2021 Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine — United States, December 14–23, 2020 CDC COVID-19 Response Team; Food and Drug Administration As of January 3, 2021, a total of 20,346,372 cases of were determined not to be anaphylaxis, 86 were judged to coronavirus disease 2019 (COVID-19) and 349,246 associ- be nonanaphylaxis allergic reactions, and 61 were considered ated deaths have been reported in the United States. Long- nonallergic adverse events. Seven case reports were still under term sequalae of COVID-19 over the course of a lifetime investigation. This report summarizes the clinical and epide- currently are unknown; however, persistent symptoms and miologic characteristics of case reports of allergic reactions, serious complications are being reported among COVID-19 including anaphylaxis and nonanaphylaxis allergic reactions, survivors, including persons who initially experience a mild after receipt of the first dose of Pfizer-BioNTech COVID-19 acute illness.* On December 11, 2020, the Food and Drug vaccine during December 14–23, 2020, in the United States. Administration (FDA) issued an Emergency Use Authorization CDC has issued updated interim clinical considerations for (EUA) for Pfizer-BioNTech COVID-19 vaccine to prevent use of mRNA COVID-19 vaccines currently authorized in the COVID-19, administered as 2 doses separated by 21 days. On United States (4) and interim considerations for preparing for December 12, 2020, the Advisory Committee on Immunization the potential management of anaphylaxis (5). In addition to Practices (ACIP) issued an interim recommendation for use screening for contraindications and precautions before admin- of Pfizer-BioNTech COVID-19 vaccine (1); initial doses were istering COVID-19 vaccines, vaccine locations should have recommended for health care personnel and long-term care the necessary supplies available to manage anaphylaxis, should facility residents (2). -

Ebola Virus Disease and Clinical Care Part I: History, Transmission, and Clinical Presentation
Ebola Virus Disease and Clinical Care Part I: History, Transmission, and Clinical Presentation This lecture is on Ebola virus disease (EVD) and clinical care. This is part one of a three-part lecture on this topic. Preparing Healthcare Workers to Work in Ebola Treatment Units (ETUs) in Africa This lecture will focus on EVD in the West African setting. Ebola Virus Disease and Clinical Care: The training and information you receive in this course will Part I: History, Transmission, and Clinical not cover the use of certain interventions such as intubation Presentation or dialysis which are not available in West African Ebola Treatment Units (ETUs). You will need supplemental training This presentation is current as of December 2014. This presentation contains materials from Centers for Disease Control and to care for patients appropriately in countries where advanced Prevention (CDC), Médecins Sans Frontières (MSF), and World Health Organization (WHO). care is available. U.S. Department of Health and Human Services U.S. Department of Health and Human Services Centers for Disease Control and Prevention Centers for Disease Control and Prevention version 12.03.2014 The learning objectives for this lecture are to: Learning Objectives ▶ Describe the routes of Ebola virus transmission Describe the routes of Ebola virus transmission Explain when and how patients are infectious ▶ Explain when and how patients are infectious Describe the clinical features of patients with Ebola ▶ Describe screening criteria for Ebola virus disease Describe the clinical features of patients with Ebola (EVD) used in West Africa Explain how to identify patients with suspected ▶ Describe screening criteria for EVD used in West Africa EVD who present to the ETU ▶ Explain how to identify patients with suspected EVD who present to the ETU This presentation contains materials from CDC, MSF, and WHO 2 A number of different viruses cause viral hemorrhagic fever. -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert, -
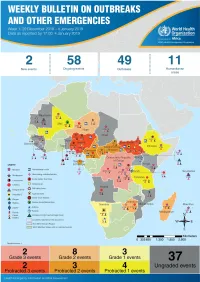
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview
1 Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview Contents This Weekly Bulletin focuses on selected acute public health emergencies occurring in the WHO African Region. The WHO Health Emergencies Programme (WHE) is currently monitoring 60 events in the region. This week’s edition covers key ongoing events, including: 2 Overview Ebola virus disease outbreak in the Democratic Republic of the Congo 3 - 6 Ongoing events Cholera in Burundi Cholera in Cameroon 7 Summary of major Yellow fever in Nigeria. issues challenges and proposed actions For each of these events, a brief description, followed by public health measures implemented and an interpretation of the situation is provided. 8 All events currently being monitored Major issues and challenges include: The Ebola virus disease (EVD) outbreak in the Democratic Republic of the Congo (DRC) is in a critical phase as it enters its sixth month since the declaration of the outbreak. Despite the use of an effective vaccine, novel therapeutics as well as other EVD strategic interventions, the outbreak is persisting due to security challenges, pockets of community reluctance and inadequate infection prevention and control in some health facilities. Nevertheless, WHO and partners, under the government’s leadership, continue to respond to the EVD outbreak and remain committed to containing the outbreak. The Ministry of Health of Burundi has declared a new outbreak of cholera in the country. This outbreak, which is rapidly evolving, is particularly affecting people living in overcrowded areas, where sanitation conditions are precarious. Given that the risk factors for transmission of water-borne diseases are prevalent in the affected communities, there is a need to aggressively tackle this outbreak at its early stage using relevant sectors in order to avoid further spread. -

Bioreactor-Grown Bacillus of Calmette and Guérin (BCG) Vaccine Protects
pharmaceutics Article Bioreactor-Grown Bacillus of Calmette and Guérin (BCG) Vaccine Protects Badgers against Virulent Mycobacterium bovis When Administered Orally: Identifying Limitations in Baited Vaccine Delivery Sandrine Lesellier 1,2, Colin P. D. Birch 3 , Dipesh Davé 1, Deanna Dalley 1, Sonya Gowtage 1, Simonette Palmer 1, Claire McKenna 1 , Gareth A. Williams 1, Roland Ashford 1, Ute Weyer 4, Sarah Beatham 5 , Julia Coats 5, Alex Nunez 6, Pedro Sanchez-Cordon 6 , John Spiropoulos 6, Stephen Powell 7, Jason Sawyer 1, Jordan Pascoe 8, Charlotte Hendon-Dunn 8, Joanna Bacon 8 and Mark A. Chambers 1,9,* 1 Department of Bacteriology, Animal and Plant Health Agency, Woodham Lane, New Haw, Addlestone, Surrey KT15 3NB, UK; [email protected] (S.L.); [email protected] (D.D.); [email protected] (D.D.); [email protected] (S.G.); [email protected] (S.P.); [email protected] (C.M.); [email protected] (G.A.W.); [email protected] (R.A.); [email protected] (J.S.) 2 Laboratoire de la Rage et de la Faune Sauvage de Nancy (LRFSN), Technopole Agricole et Vétérinaire, Domaine de Pixérécourt-Bât. H., CS 40009-54220 Malzéville, France 3 Department of Epidemiological Sciences, Animal and Plant Health Agency, Woodham Lane, New Haw, Addlestone, Surrey KT15 3NB, UK; [email protected] 4 Animal Services Unit, Animal and Plant Health Agency, Woodham Lane, New Haw, Addlestone, Surrey KT15 3NB, UK; [email protected] 5 Animal and Plant Health Agency, Sand Hutton Campus, York, North -

COVID-19 Vaccine and Allergy
COVID Vaccine and Allergy Stephanie Leonard, MD Associate Clinical Professor Department of Pediatric Allergy & Immunology January 20, 2020 Safe and Impactful • Proper Screening COVID Vaccine • Monitoring Administration • Clinical Assessment • Vaccine Adverse Event Reporting System (VAERS) detected 21 cases of anaphylaxis after administration of a reported 1,893,360 first doses of the Pfizer-BioNTech COVID-19 vaccine • 11.1 cases per million doses (0.001%) • 1.3 cases per million for flu vaccines • 71% occurred within 15 min of vaccination, 86% within 30 minutes • Range = 2–150 minutes • Of 20 with follow-up info, all had recovered or been discharged home. • 17 (81%) with h/o allergies to food, vaccine, medication, venom, contrast, or pets. • 4 with no h/o any allergies • 7 with h/o anaphylaxis • Rabies vaccine • Flu vaccine • 19 (90%) diffuse rash or generalized hives Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine — United States, December 14–23, 2020. MMWR Morb Mortal Wkly Rep 2021;70:46–51. Early Signs of Anaphylaxis • Respiratory: sensation of throat closing*, stridor, shortness of breath, wheeze, cough • Gastrointestinal: nausea*, vomiting, diarrhea, abdominal pain • Cardiovascular: dizziness*, fainting, tachycardia, hypotension • Skin/mucosal: generalized hives, itching, or swelling of lips, face, throat *these can be subjective and overlap with anxiety or vasovagal syndrome Labs that can help assess for anaphylaxis • Tryptase, serum (red top tube) • C5b-9 terminal complement complex Level, serum (SC5B9) (lavender top EDTA tube) Emergency Supplies Management of anaphylaxis at a COVID-19 vaccination site • If anaphylaxis is suspected, take the following steps: • Rapidly assess airway, breathing, circulation, and mentation (mental activity).