Key Messages and Actions for Zika Prevention and Control: Guide for Schools Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dengue Fact Sheet
State of California California Department of Public Health Health and Human Services Agency Division of Communicable Disease Control Dengue Fact Sheet What is dengue? Dengue is a disease caused by any one of four closely related dengue viruses (DENV- 1, DENV-2, DENV-3, and DENV-4). Where does dengue occur? Dengue occurs in many tropical and sub-tropical areas of the world, particularly sub- Saharan Africa, the Middle East, Southeast Asia, and Central and South America. With the exception of Mexico, Puerto Rico, small areas in southern Texas and southern Florida, and some regions of Hawaii, dengue transmission does not occur in North America. Worldwide there are an estimated 50 to 100 million cases of dengue per year. How do people get dengue? People get dengue from the bite of an infected mosquito. The mosquito becomes infected when it bites a person who has dengue virus in their blood. It takes a week or more for the dengue organisms to mature in the mosquito; then the mosquito can transmit the virus to another person when it bites. Dengue is transmitted principally by Aedes aegypti (yellow fever mosquito) and Aedes albopictus (Asian tiger mosquito). These mosquitoes are not native to California, but infestations have been identified in multiple counties in California. Dengue virus cannot be transmitted from person to person. What are the symptoms of dengue? There are two types of illness that can result from infection with a dengue virus: dengue and severe dengue. The main symptoms of dengue are high fever, severe headache, severe pain behind the eyes, joint pain, muscle and bone pain, rash, bruising, and may include mild bleeding from the nose or mouth. -

Dengue and Yellow Fever
GBL42 11/27/03 4:02 PM Page 262 CHAPTER 42 Dengue and Yellow Fever Dengue, 262 Yellow fever, 265 Further reading, 266 While the most important viral haemorrhagic tor (Aedes aegypti) as well as reinfestation of this fevers numerically (dengue and yellow fever) are insect into Central and South America (it was transmitted exclusively by arthropods, other largely eradicated in the 1960s). Other factors arboviral haemorrhagic fevers (Crimean– include intercontinental transport of car tyres Congo and Rift Valley fevers) can also be trans- containing Aedes albopictus eggs, overcrowding mitted directly by body fluids. A third group of of refugee and urban populations and increasing haemorrhagic fever viruses (Lassa, Ebola, Mar- human travel. In hyperendemic areas of Asia, burg) are only transmitted directly, and are not disease is seen mainly in children. transmitted by arthropods at all. The directly Aedes mosquitoes are ‘peri-domestic’: they transmissible viral haemorrhagic fevers are dis- breed in collections of fresh water around the cussed in Chapter 41. house (e.g. water storage jars).They feed on hu- mans (anthrophilic), mainly by day, and feed re- peatedly on different hosts (enhancing their role Dengue as vectors). Dengue virus is numerically the most important Clinical features arbovirus infecting humans, with an estimated Dengue virus may cause a non-specific febrile 100 million cases per year and 2.5 billion people illness or asymptomatic infection, especially in at risk.There are four serotypes of dengue virus, young children. However, there are two main transmitted by Aedes mosquitoes, and it is un- clinical dengue syndromes: dengue fever (DF) usual among arboviruses in that humans are the and dengue haemorrhagic fever (DHF). -

Mosquito Repellents for Travellers. BMJ (Clinical Research Ed), 350
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by LSHTM Research Online Stanczyk, NM; Behrens, RH; Chen-Hussey, V; Stewart, SA; Logan, JG (2015) Mosquito repellents for travellers. BMJ (Clinical research ed), 350. h99. ISSN 0959-8138 DOI: 10.1136/bmj.h99 Downloaded from: http://researchonline.lshtm.ac.uk/2121428/ DOI: 10.1136/bmj.h99 Usage Guidelines Please refer to usage guidelines at http://researchonline.lshtm.ac.uk/policies.html or alterna- tively contact [email protected]. Available under license: Creative Commons Attribution Non-commercial http://creativecommons.org/licenses/by-nc/2.5/ BMJ 2015;350:h99 doi: 10.1136/bmj.h99 (Published 19 February 2015) Page 1 of 4 Practice PRACTICE THERAPEUTICS Mosquito repellents for travellers 1 1 2 Nina M Stanczyk research fellow , Ron H Behrens senior lecturer , Vanessa Chen-Hussey research 1 3 scientist and clinical trials manager , Sophie A Stewart senior research scientist and clinical trials 3 1 3 coordinator , James G Logan senior lecturer 1Department of Disease Control, London School of Hygiene and Tropical Medicine, London WC1E 7HT, UK; 2Hospital for Tropical Diseases, London, UK; 3Arthropod Control Product Test Centre, London School of Hygiene and Tropical Medicine, London, UK This is one of a series of occasional articles on therapeutics for common isolated as a byproduct of Eucalyptus citriodora (lemon or serious conditions, covering new drugs and old drugs with important eucalyptus). new indications or concerns. The series advisers are Robin Ferner, honorary professor of clinical pharmacology, University of Birmingham Icaridin—Icaridin (hydroxyethyl isobutyl piperidine and Birmingham City Hospital, and Albert Ferro, professor of carboxylate) is also known by the trade names Bayrepel, cardiovascular clinical pharmacology, King’s College London. -

Reflexion on Bio-Sourced Mosquito Repellents: Nature, Activity, and Preparation Claude Grison, David Carrasco, Franck Pelissier, Alexandra Moderc
Reflexion on Bio-Sourced Mosquito Repellents: Nature, Activity, and Preparation Claude Grison, David Carrasco, Franck Pelissier, Alexandra Moderc To cite this version: Claude Grison, David Carrasco, Franck Pelissier, Alexandra Moderc. Reflexion on Bio-Sourced Mosquito Repellents: Nature, Activity, and Preparation. Frontiers in Ecology and Evolution, Fron- tiers Media S.A, 2020, 8, 10.3389/fevo.2020.00008. hal-03051738 HAL Id: hal-03051738 https://hal.archives-ouvertes.fr/hal-03051738 Submitted on 10 Dec 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution| 4.0 International License fevo-08-00008 February 5, 2020 Time: 16:18 # 1 REVIEW published: 07 February 2020 doi: 10.3389/fevo.2020.00008 Reflexion on Bio-Sourced Mosquito Repellents: Nature, Activity, and Preparation Claude Grison1*, David Carrasco2, Franck Pelissier1 and Alexandra Moderc1 1 Laboratory of Bio-inspired Chemistry and Ecological Innovations, ChimEco (UMR 5021), University of Montpellier, CNRS, Montpellier, France, 2 MIVEGEC, University of Montpellier, IRD, CNRS, Montpellier, France Over the last decades, the geographical distribution of certain mosquito species carrying vector-borne diseases has considerably expanded. They represent a major health concern as they transmit pathogens causing alarming epidemics. -

Dengue Fever/Severe Dengue Fever/Chikungunya Fever! Report on Suspicion of Infection During Business Hours
Dengue Fever/Severe Dengue Fever/Chikungunya Fever! Report on suspicion of infection during business hours PROTOCOL CHECKLIST Enter available information into Merlin upon receipt of initial report Review background information on the disease (see Section 2), case definitions (see Section 3 for dengue and for chikungunya), and laboratory testing (see Section 4) Forward specimens to the Florida Department of Health (DOH) Bureau of Public Health Laboratories (BPHL) for confirmatory laboratory testing (as needed) Inform local mosquito control personnel of suspected chikungunya or dengue case as soon as possible (if applicable) Inform state Arbovirus Surveillance Coordinator on suspicion of locally acquired arbovirus infection Contact provider (see Section 5A) Interview case-patient Review disease facts (see Section 2) Mode of transmission Ask about exposure to relevant risk factors (see Section 5. Case Investigation) History of travel, outdoor activities, and mosquito bites two weeks prior to onset History of febrile illness or travel for household members or other close contacts in the month prior to onset History of previous arbovirus infection or vaccination (yellow fever, Japanese encephalitis) Provide education on transmission and prevention (see Section 6) Awareness of mosquito-borne diseases Drain standing water at least weekly to stop mosquitoes from multiplying Discard items that collect water and are not being used Cover skin with clothing or Environmental Protection Agency (EPA)-registered repellent such as DEET (N,N-diethyl-meta-toluamide) Use permethrin on clothing (not skin) according to manufacturer’s directions Cover doors and windows with intact screens to keep mosquitoes out of the house Enter additional data obtained from interview into Merlin (see Section 5D) Arrange for a convalescent specimen to be taken (if necessary) Dengue/Chikungunya Guide to Surveillance and Investigation Dengue Fever/Severe Dengue/Chikungunya 1. -

Mosquito Repellent Thermal Stability, Permeability and Air Volatility
Published as: António B Mapossa, Walter W Focke, Alcides Sitoe, Homa Izadi, Elizbé du Toit, René Androsch, Chanita Sungkapreecha, L. van der Merwe. Mosquito repellent thermal stability, permeability and air volatility. Pest Management Science, 76, 1112-1120. Mosquito repellent thermal stability, permeability and air volatility António B Mapossa1,2, Alcides Sitoe1,2,3, Walter W Focke1,2,*, Homa Izadi1, Elizabeth L du Toit1, René Androsch4, Chanita Sungkapreecha4, Elizabet M. van der Merwe5 1Institute of Applied Materials, Department of Chemical Engineering, University of Pretoria, Lynnwood Road, Pretoria, South Africa 2UP Institute for Sustainable Malaria Control & MRC Collaborating Centre for Malaria Research, University of Pretoria, Private Bag X20, Hatfield 0028, Pretoria, South Africa, Pretoria, South Africa 3Department of Chemistry, Eduardo Mondlane University, Maputo, Mozambique 4Interdisciplinary Center for Transfer-oriented Research in Natural Sciences, Martin Luther University Halle- Wittenberg, D-06099 Halle/Saale, Germany 5Department of Chemistry, University of Pretoria, Lynnwood Road, Pretoria, South Africa Abstract BACKGROUND: The effectiveness of mosquito repellents, whether applied topically on the skin or released from a wearable device, is crucially determined by the evaporation rate. This is because a repellent has to be present in the form of vapour in the vicinity of the exposed skin that needs protection. Therefore, gravimetric techniques were used to investigate the direct evaporation of selected liquid repellents, their permeation through polymer films, and their release from a microporous polyethylene matrix. RESULTS: Evaporation of a repellent into quiescent air is determined by its air permeability. It is defined as the product of the vapour pressure and the diffusion coefficient, i.e. = . It was found that the repellent ranking, in terms of decreasing volatility, was ethyl anthranilate > citriodiol > dimethyl phthalate > DEET > decanoic acid > ethyl butylacetylaminopropionate > Icaridin. -

Insect Repellent Essentials
Insect Repellent Essentials: A Brief Guide Insect repellents are substances that, when used as directed, can reduce tick, mosquito, and other insect bites. Preventing bites will help you avoid disease-causing pathogens carried by these animals. WHY SHOULD YOU USE INSECT REPELLENT? You can protect yourself from ticks and mosquitoes by properly applying insect repellents when outdoors during times of year when these critters are most active. Repellents used on your skin generally work by How do they making it harder for biting insects and ticks to work? smell or find you. Not all ticks and mosquitoes carry disease-causing agents, but there are a few in the Northeast that can be harmful: Several mosquito species in the Northeast can transmit: West Nile virus Eastern equine encephalitis virus LaCrosse encephalitis virus Jamestown Canyon virus Blacklegged (aka deer) ticks: Lone star ticks: Lyme disease Ehrlichiosis Anaplasmosis Tularemia Babesiosis Heartland virus Ehrlichiosis Powassan virus disease American dog ticks: Brown dog ticks: Tularemia Rocky Mountain Rocky Mountain Spotted Fever Spotted Fever Visit www.cdc.gov/ncezid/dvbd to learn more about these vector-borne diseases WHEN SHOULD YOU APPLY INSECT REPELLENT? Apply insect repellent when you are outdoors in tick or mosquito habitats. Ticks in the Northeast can be active year-round and any time of day. They are most active during the warmer months of the year, and can be as small as poppy seeds during the spring and summer. You can still be bitten by a tick in the winter! If the temperature is warm enough and the snow has started to melt, ticks can be active. -

Ebola Virus Disease and Clinical Care Part I: History, Transmission, and Clinical Presentation
Ebola Virus Disease and Clinical Care Part I: History, Transmission, and Clinical Presentation This lecture is on Ebola virus disease (EVD) and clinical care. This is part one of a three-part lecture on this topic. Preparing Healthcare Workers to Work in Ebola Treatment Units (ETUs) in Africa This lecture will focus on EVD in the West African setting. Ebola Virus Disease and Clinical Care: The training and information you receive in this course will Part I: History, Transmission, and Clinical not cover the use of certain interventions such as intubation Presentation or dialysis which are not available in West African Ebola Treatment Units (ETUs). You will need supplemental training This presentation is current as of December 2014. This presentation contains materials from Centers for Disease Control and to care for patients appropriately in countries where advanced Prevention (CDC), Médecins Sans Frontières (MSF), and World Health Organization (WHO). care is available. U.S. Department of Health and Human Services U.S. Department of Health and Human Services Centers for Disease Control and Prevention Centers for Disease Control and Prevention version 12.03.2014 The learning objectives for this lecture are to: Learning Objectives ▶ Describe the routes of Ebola virus transmission Describe the routes of Ebola virus transmission Explain when and how patients are infectious ▶ Explain when and how patients are infectious Describe the clinical features of patients with Ebola ▶ Describe screening criteria for Ebola virus disease Describe the clinical features of patients with Ebola (EVD) used in West Africa Explain how to identify patients with suspected ▶ Describe screening criteria for EVD used in West Africa EVD who present to the ETU ▶ Explain how to identify patients with suspected EVD who present to the ETU This presentation contains materials from CDC, MSF, and WHO 2 A number of different viruses cause viral hemorrhagic fever. -
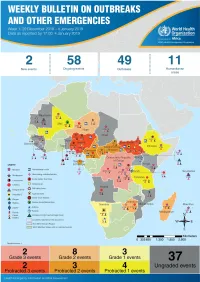
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview
1 Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview Contents This Weekly Bulletin focuses on selected acute public health emergencies occurring in the WHO African Region. The WHO Health Emergencies Programme (WHE) is currently monitoring 60 events in the region. This week’s edition covers key ongoing events, including: 2 Overview Ebola virus disease outbreak in the Democratic Republic of the Congo 3 - 6 Ongoing events Cholera in Burundi Cholera in Cameroon 7 Summary of major Yellow fever in Nigeria. issues challenges and proposed actions For each of these events, a brief description, followed by public health measures implemented and an interpretation of the situation is provided. 8 All events currently being monitored Major issues and challenges include: The Ebola virus disease (EVD) outbreak in the Democratic Republic of the Congo (DRC) is in a critical phase as it enters its sixth month since the declaration of the outbreak. Despite the use of an effective vaccine, novel therapeutics as well as other EVD strategic interventions, the outbreak is persisting due to security challenges, pockets of community reluctance and inadequate infection prevention and control in some health facilities. Nevertheless, WHO and partners, under the government’s leadership, continue to respond to the EVD outbreak and remain committed to containing the outbreak. The Ministry of Health of Burundi has declared a new outbreak of cholera in the country. This outbreak, which is rapidly evolving, is particularly affecting people living in overcrowded areas, where sanitation conditions are precarious. Given that the risk factors for transmission of water-borne diseases are prevalent in the affected communities, there is a need to aggressively tackle this outbreak at its early stage using relevant sectors in order to avoid further spread. -

Mosquitoes and West Nile Virus
Biologist’s meeting 11-Feb-2016 Scott C. Crans Rutgers Entomology/CVB/OCPE Contact Info: [email protected] Phone 848 932-6497 • Zika update Objectives • Vector bionomics • Species distribution • ID & monitoring • Local MCP response • Trapping • Reference collections CDC Survey https://docs.google.com/forms/d/1eqWDzmFw7AEGDyooZwpUXsebzh8qrUkzQJ82PDiYLPI/viewform?c=0&w=1 Fill out the survey for your county Maps were developed by CDC using currently available information. Mosquito populations may be detected in areas not shaded on this map, and may not be consistently found in all shaded areas. Container ecosystem • Container mosquitoes • Develop in <1L of water Endless examples Primary vector of Yellow fever, Dengue, Chikungunya, Zika http://fmel.ifas.ufl.edu/key/genus/aedes_aeg.shtml • Urban mosquito • Container habitats • Day biting (dusk & dawn) • Multiple bloodmeals • Endophilic • Anthropophilic Aedes aegypti • Highly adaptive mosquito • Natural & artificial containers • Rural & suburban • Opportunistic day biting (dusk & dawn) • Outside & inside • *Wider host range Aedes albopictus 10 d ? 3-7 d ? extrinsic incubation intrinsic incubation gonotrophic cycle ? State & county mosquito control responsibilities IVM components (Integrated Vector Management) • Continuing professional education • Public education • Mosquito & virus surveillance • Source reduction • Bio-Control • Larviciding • Pupiciding • Aduticiding • Annual reporting NJ philosophy • Measures populations • Justifies intervention • Effectiveness of abatement • Targets -

Natural and Synthetic Repellents for Pest Management of the Storage Mite Tyrophagus Putrescentiae (Schrank) (Sarcoptiformes: Acaridae)
insects Article Natural and Synthetic Repellents for Pest Management of the Storage Mite Tyrophagus putrescentiae (Schrank) (Sarcoptiformes: Acaridae) Naomi Manu 1, Mark Wesley Schilling 2 and Thomas Wesley Phillips 1,* 1 Department of Entomology, Kansas State University, Manhattan, KS 66506, USA; [email protected] 2 Department of Food Science Nutrition and Health Promotion, Mississippi State University, Mississippi State, MS 39762, USA; [email protected] * Correspondence: [email protected] Simple Summary: The ham mite is the major pest of dry-cured hams, aged cheeses, and specialty pet foods that are high in fats and proteins. Ham mites are also known to cause allergies in some cases for humans. The toxic fumigant gas methyl bromide had been used for years to control this mite pest, but it is being phased out of use due to its impact on the protective ozone layer of the earth’s upper atmosphere. Ham producers now require alternatives to methyl bromide for controlling mites. We conducted laboratory experiments with food-safe synthetic and plant-derived chemical repellents to keep mites away from dry cured hams. Our results showed that several of these repellents could effectively prevent ham mites from contacting and staying on treated pieces of ham, and that they would readily go to untreated ham pieces when given a choice. Further experiments found that mites would not feed on nor produce offspring when held on ham pieces coated with oils from thyme, lemon grass, rose, or a mixture of naturally occurring fat molecules. Our experiments suggest that Citation: Manu, N.; Schilling, these food-safe repellents might protect dry-cured hams from mites during their time in aging rooms M.W.; Phillips, T.W. -

Systematic Review of Important Viral Diseases in Africa in Light of the ‘One Health’ Concept
pathogens Article Systematic Review of Important Viral Diseases in Africa in Light of the ‘One Health’ Concept Ravendra P. Chauhan 1 , Zelalem G. Dessie 2,3 , Ayman Noreddin 4,5 and Mohamed E. El Zowalaty 4,6,7,* 1 School of Laboratory Medicine and Medical Sciences, College of Health Sciences, University of KwaZulu-Natal, Durban 4001, South Africa; [email protected] 2 School of Mathematics, Statistics and Computer Science, University of KwaZulu-Natal, Durban 4001, South Africa; [email protected] 3 Department of Statistics, College of Science, Bahir Dar University, Bahir Dar 6000, Ethiopia 4 Infectious Diseases and Anti-Infective Therapy Research Group, Sharjah Medical Research Institute and College of Pharmacy, University of Sharjah, Sharjah 27272, UAE; [email protected] 5 Department of Medicine, School of Medicine, University of California, Irvine, CA 92868, USA 6 Zoonosis Science Center, Department of Medical Biochemistry and Microbiology, Uppsala University, SE 75185 Uppsala, Sweden 7 Division of Virology, Department of Infectious Diseases and St. Jude Center of Excellence for Influenza Research and Surveillance (CEIRS), St Jude Children Research Hospital, Memphis, TN 38105, USA * Correspondence: [email protected] Received: 17 February 2020; Accepted: 7 April 2020; Published: 20 April 2020 Abstract: Emerging and re-emerging viral diseases are of great public health concern. The recent emergence of Severe Acute Respiratory Syndrome (SARS) related coronavirus (SARS-CoV-2) in December 2019 in China, which causes COVID-19 disease in humans, and its current spread to several countries, leading to the first pandemic in history to be caused by a coronavirus, highlights the significance of zoonotic viral diseases.