Biologically Active Metabolites from Hungarian Mushrooms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Mushrooms Have Evolved to Be So Promiscuous: Insights from Evolutionary and Ecological Patterns
fungal biology reviews 29 (2015) 167e178 journal homepage: www.elsevier.com/locate/fbr Review Why mushrooms have evolved to be so promiscuous: Insights from evolutionary and ecological patterns Timothy Y. JAMES* Department of Ecology and Evolutionary Biology, University of Michigan, Ann Arbor, MI 48109, USA article info abstract Article history: Agaricomycetes, the mushrooms, are considered to have a promiscuous mating system, Received 27 May 2015 because most populations have a large number of mating types. This diversity of mating Received in revised form types ensures a high outcrossing efficiency, the probability of encountering a compatible 17 October 2015 mate when mating at random, because nearly every homokaryotic genotype is compatible Accepted 23 October 2015 with every other. Here I summarize the data from mating type surveys and genetic analysis of mating type loci and ask what evolutionary and ecological factors have promoted pro- Keywords: miscuity. Outcrossing efficiency is equally high in both bipolar and tetrapolar species Genomic conflict with a median value of 0.967 in Agaricomycetes. The sessile nature of the homokaryotic Homeodomain mycelium coupled with frequent long distance dispersal could account for selection favor- Outbreeding potential ing a high outcrossing efficiency as opportunities for choosing mates may be minimal. Pheromone receptor Consistent with a role of mating type in mediating cytoplasmic-nuclear genomic conflict, Agaricomycetes have evolved away from a haploid yeast phase towards hyphal fusions that display reciprocal nuclear migration after mating rather than cytoplasmic fusion. Importantly, the evolution of this mating behavior is precisely timed with the onset of diversification of mating type alleles at the pheromone/receptor mating type loci that are known to control reciprocal nuclear migration during mating. -

Boletus Mushrooms La Tia Jackson, Ian C
Genetic Diversity within Alaskan Boletus Mushrooms www.fungi-zette.com La Tia Jackson, Ian C. Herriott, József Geml, Gary A. Laursen, D. Lee Taylor Discussion Abstract •Clade 1 is composed of Alaskan samples from the interior and Northwest and We analyzed the genetic differences within the collection of samples from Europe. Although the species names do not match up they are genetically very similar, and B. citrinovirens is thought to be in what is called the Boletus mushroom from the UAF Fungal Herbarium, representing Identification on Tree Location subtomentosus group. samples from all over Alaska. Upon analyzing the DNA sequence Results DQ066405_Boletus_citrinovirens Europe from 18 samples, we found that most Alaskan Boletus are closely DQ066407_Boletus_spadiceus Europe •Clade 2 is composed of Alaskan samples from Southeast Alaska and GenBank DQ066397_Boletus_citrinovirens Europe samples from Europe, both identified as Boletus mirabilis. related to samples from the same species found in other parts of the world (clades 1,2,5,6,8,12). We also found that some species DQ066410_Boletus_spadiceus Europe •Clade 3 is composed of samples only from Alaska. None of the sequences DQ384578_Boletellus_mirabilis Europe collected in other parts of the world were not found in our sample 1 mycorance.free.fr obtained from GenBank are closely related. These were morphologically collection (clades 4,7,9,10,11). Finally, our results suggested that AJ419187_Boletus_impolitus Spain identified as B. subglabripes. “B. subglabripes” is in GenBank, but only Large 100 DQ131632_Xerocomus_subtomentosus Europe clade 3 on our phylogenetic tree is not represented among the Subunit gene, not Internally Transcribed Spacer gene (reference 2) so comparison AJ889931_Boletus_pruinatus Europe GenBank sequences from other parts of the world and may be a 100 is not possible to determine if morphological species attribution is the same or 2 AM087271_Xerocomus_pruinatus Europe genetic lineage endemic to Alaska. -

Influence of Tree Species on Richness and Diversity of Epigeous Fungal
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Archive Ouverte en Sciences de l'Information et de la Communication fungal ecology 4 (2011) 22e31 available at www.sciencedirect.com journal homepage: www.elsevier.com/locate/funeco Influence of tree species on richness and diversity of epigeous fungal communities in a French temperate forest stand Marc BUE´Ea,*, Jean-Paul MAURICEb, Bernd ZELLERc, Sitraka ANDRIANARISOAc, Jacques RANGERc,Re´gis COURTECUISSEd, Benoıˆt MARC¸AISa, Franc¸ois LE TACONa aINRA Nancy, UMR INRA/UHP 1136 Interactions Arbres/Microorganismes, 54280 Champenoux, France bGroupe Mycologique Vosgien, 18 bis, place des Cordeliers, 88300 Neufchaˆteau, France cINRA Nancy, UR 1138 Bioge´ochimie des Ecosyste`mes Forestiers, 54280 Champenoux, France dUniversite´ de Lille, Faculte´ de Pharmacie, F59006 Lille, France article info abstract Article history: Epigeous saprotrophic and ectomycorrhizal (ECM) fungal sporocarps were assessed during Received 30 September 2009 7 yr in a French temperate experimental forest site with six 30-year-old mono-specific Revision received 10 May 2010 plantations (four coniferous and two hardwood plantations) and one 150-year-old native Accepted 21 July 2010 mixed deciduous forest. A total of 331 fungal species were identified. Half of the fungal Available online 6 October 2010 species were ECM, but this proportion varied slightly by forest composition. The replace- Corresponding editor: Anne Pringle ment of the native forest by mono-specific plantations, including native species such as beech and oak, considerably altered the diversity of epigeous ECM and saprotrophic fungi. Keywords: Among the six mono-specific stands, fungal diversity was the highest in Nordmann fir and Conifer plantation Norway spruce plantations and the lowest in Corsican pine and Douglas fir plantations. -

Checklist of the Species of the Genus Tricholoma (Agaricales, Agaricomycetes) in Estonia
Folia Cryptog. Estonica, Fasc. 47: 27–36 (2010) Checklist of the species of the genus Tricholoma (Agaricales, Agaricomycetes) in Estonia Kuulo Kalamees Institute of Ecology and Earth Sciences, University of Tartu, 40 Lai St. 51005, Tartu, Estonia. Institute of Agricultural and Environmental Sciences, Estonian University of Life Sciences, 181 Riia St., 51014 Tartu, Estonia E-mail: [email protected] Abstract: 42 species of genus Tricholoma (Agaricales, Agaricomycetes) have been recorded in Estonia. A checklist of these species with ecological, phenological and distribution data is presented. Kokkukvõte: Perekonna Tricholoma (Agaricales, Agaricomycetes) liigid Eestis Esitatakse kriitiline nimestik koos ökoloogiliste, fenoloogiliste ja levikuliste andmetega heiniku perekonna (Tricholoma) 42 liigi (Agaricales, Agaricomycetes) kohta Eestis. INTRODUCTION The present checklist contains 42 Tricholoma This checklist also provides data on the ecol- species recorded in Estonia. All the species in- ogy, phenology and occurrence of the species cluded (except T. gausapatum) correspond to the in Estonia (see also Kalamees, 1980a, 1980b, species conceptions established by Christensen 1982, 2000, 2001b, Kalamees & Liiv, 2005, and Heilmann-Clausen (2008) and have been 2008). The following data are presented on each proved by relevant exsiccates in the mycothecas taxon: (1) the Latin name with a reference to the TAAM of the Institute of Agricultural and Envi- initial source; (2) most important synonyms; (3) ronmental Sciences of the Estonian University reference to most important and representative of Life Sciences or TU of the Natural History pictures (iconography) in the mycological litera- Museum of the Tartu University. In this paper ture used in identifying Estonian species; (4) T. gausapatum is understand in accordance with data on the ecology, phenology and distribution; Huijsman, 1968 and Bon, 1991. -

CZECH MYCOLOGY Publication of the Czech Scientific Society for Mycology
CZECH MYCOLOGY Publication of the Czech Scientific Society for Mycology Volume 57 August 2005 Number 1-2 Central European genera of the Boletaceae and Suillaceae, with notes on their anatomical characters Jo s e f Š u t a r a Prosetická 239, 415 01 Tbplice, Czech Republic Šutara J. (2005): Central European genera of the Boletaceae and Suillaceae, with notes on their anatomical characters. - Czech Mycol. 57: 1-50. A taxonomic survey of Central European genera of the families Boletaceae and Suillaceae with tubular hymenophores, including the lamellate Phylloporus, is presented. Questions concerning the delimitation of the bolete genera are discussed. Descriptions and keys to the families and genera are based predominantly on anatomical characters of the carpophores. Attention is also paid to peripheral layers of stipe tissue, whose anatomical structure has not been sufficiently studied. The study of these layers, above all of the caulohymenium and the lateral stipe stratum, can provide information important for a better understanding of relationships between taxonomic groups in these families. The presence (or absence) of the caulohymenium with spore-bearing caulobasidia on the stipe surface is here considered as a significant ge neric character of boletes. A new combination, Pseudoboletus astraeicola (Imazeki) Šutara, is proposed. Key words: Boletaceae, Suillaceae, generic taxonomy, anatomical characters. Šutara J. (2005): Středoevropské rody čeledí Boletaceae a Suillaceae, s poznámka mi k jejich anatomickým znakům. - Czech Mycol. 57: 1-50. Je předložen taxonomický přehled středoevropských rodů čeledí Boletaceae a. SuiUaceae s rourko- vitým hymenoforem, včetně rodu Phylloporus s lupeny. Jsou diskutovány otázky týkající se vymezení hřibovitých rodů. Popisy a klíče k čeledím a rodům jsou založeny převážně na anatomických znacích plodnic. -

The Bioaccumulation of Some Heavy Metals in the Fruiting Body of Wild Growing Mushrooms
Available online at www.notulaebotanicae.ro Print ISSN 0255-965X; Electronic 1842-4309 Not. Bot. Hort. Agrobot. Cluj 38 (2) 2010, Special Issue, 147-151 Notulae Botanicae Horti Agrobotanici Cluj-Napoca The Bioaccumulation of Some Heavy Metals in the Fruiting Body of Wild Growing Mushrooms Carmen Cristina ELEKES1) , Gabriela BUSUIOC1) , Gheorghe IONITA 2) 1) Valahia University of Targoviste, Faculty of Environmental Engineering and Biotechnologies, Bd. Regele Carol I, no. 2, Romania; [email protected] 2) Valahia University of Targoviste, Faculty of Materials Engineering, Mechatronics and Robotics, Bd. Regele Carol I, no. 2, Romania Abstract Due to their effective mechanism of accumulation of heavy metals from soil, the macrofungi show high concentrations of metals in their fruiting body. According with this ability, the mushrooms can be used to evaluate and control the level of environmental pollution, but also represent danger for human ingestion. We analyzed some macrofungi species from a wooded area to establish the heavy metal concentrations and ability of bioaccumulation and translocation for Zn, Cu and Sn in fruiting body. The metallic content was established by the Inductively Coupled Plasma-Atomic Emission Spectrometry method (ICP-AES). The minimal detection limits of method is 0.4 mg/kg for Zn and Cu and 0.6 mg/kg for Sn. Heavy metals concentrations in the fruiting body ranged between 6.98- 20.10 mg/kg for Zn (the higher value was for Tapinella atrotomentosa); 16.13-144.94 mg/kg for Cu (the higher value was for Hypholoma fasciculare); and 24.36-150.85 mg/kg for Sn (the higher value was for Paxillus involutus). -

And Interspecific Hybridiation in Agaric Fungi
Mycologia, 105(6), 2013, pp. 1577–1594. DOI: 10.3852/13-041 # 2013 by The Mycological Society of America, Lawrence, KS 66044-8897 Evolutionary consequences of putative intra- and interspecific hybridization in agaric fungi Karen W. Hughes1 to determine the outcome of hybridization events. Ronald H. Petersen Within Armillaria mellea and Amanita citrina f. Ecology and Evolutionary Biology, University of lavendula, we found evidence of interbreeding and Tennessee, Knoxville, Tennessee 37996-1100 recombination. Within G. dichrous and H. flavescens/ D. Jean Lodge chlorophana, hybrids were identified but there was Center for Forest Mycology Research, USDA-Forest no evidence for F2 or higher progeny in natural Service, Northern Research Station, Box 137, Luquillo, populations suggesting that the hybrid fruitbodies Puerto Rico 00773-1377 might be an evolutionary dead end and that the Sarah E. Bergemann genetically divergent Mendelian populations from which they were derived are, in fact, different species. Middle Tennessee State University, Department of Biology, PO Box 60, Murfreesboro Tennessee 37132 The association between ITS haplotype divergence of less than 5% (Armillaria mellea 5 2.6% excluding Kendra Baumgartner gaps; Amanita citrina f. lavendula 5 3.3%) with the USDA-Agricultural Research Service, Department of presence of putative recombinants and greater than Plant Pathology, University of California, Davis, California 95616 5% (Gymnopus dichrous 5 5.7%; Hygrocybe flavescens/ chlorophana 5 14.1%) with apparent failure of F1 2 Rodham E. Tulloss hybrids to produce F2 or higher progeny in popula- PO Box 57, Roosevelt, New Jersey 08555-0057 tions may suggest a correlation between genetic Edgar Lickey distance and reproductive isolation. -

Tricholoma (Fr.) Staude in the Aegean Region of Turkey
Turkish Journal of Botany Turk J Bot (2019) 43: 817-830 http://journals.tubitak.gov.tr/botany/ © TÜBİTAK Research Article doi:10.3906/bot-1812-52 Tricholoma (Fr.) Staude in the Aegean region of Turkey İsmail ŞEN*, Hakan ALLI Department of Biology, Faculty of Science, Muğla Sıtkı Koçman University, Muğla, Turkey Received: 24.12.2018 Accepted/Published Online: 30.07.2019 Final Version: 21.11.2019 Abstract: The Tricholoma biodiversity of the Aegean region of Turkey has been determined and reported in this study. As a consequence of field and laboratory studies, 31 Tricholoma species have been identified, and five of them (T. filamentosum, T. frondosae, T. quercetorum, T. rufenum, and T. sudum) have been reported for the first time from Turkey. The identification key of the determined taxa is given with this study. Key words: Tricholoma, biodiversity, identification key, Aegean region, Turkey 1. Introduction & Intini (this species, called “sedir mantarı”, is collected by Tricholoma (Fr.) Staude is one of the classic genera of local people for both its gastronomic and financial value) Agaricales, and more than 1200 members of this genus and T. virgatum var. fulvoumbonatum E. Sesli, Contu & were globally recorded in Index Fungorum to date (www. Vizzini (Intini et al., 2003; Vizzini et al., 2015). Additionally, indexfungorum.org, access date 23 April 2018), but many Heilmann-Clausen et al. (2017) described Tricholoma of them are placed in other genera such as Lepista (Fr.) ilkkae Mort. Chr., Heilm.-Claus., Ryman & N. Bergius as W.G. Sm., Melanoleuca Pat., and Lyophyllum P. Karst. a new species and they reported that this species grows in (Christensen and Heilmann-Clausen, 2013). -

<I>Gymnopus Fuscotramus</I> (<I>Agaricales</I
ISSN (print) 0093-4666 © 2011. Mycotaxon, Ltd. ISSN (online) 2154-8889 MYCOTAXON http://dx.doi.org/10.5248/117.321 Volume 117, pp. 321–330 July–September 2011 Gymnopus fuscotramus (Agaricales), a new species from southern China Armin Mešić1, Zdenko Tkalčec1*, Chun-Ying Deng2, 3, Tai-Hui Li2, Bruna Pleše 1 & Helena Ćetković1 1Ruđer Bošković Institute, Bijenička 54, HR-10000 Zagreb, Croatia 2Guangdong Provincial Key Laboratory of Microbial Culture Collection and Application, Guangdong Institute of Microbiology, Guangzhou 510070, China 3School of Bioscience and Biotechnology, South China University of Technology, Guangzhou, 510641, China Correspondence to *: [email protected], * [email protected], [email protected], [email protected] & [email protected] Abstract — A new species, Gymnopus fuscotramus, is described from China. It is characterized by brown-incarnate colors in pileus and lamellae, sulcate pileus, free and distant lamellae, floccose-squamulose, mostly black stipe, well-developed black rhizomorphs, repent and diverticulate pileipellis hyphae, abundant clamp connections, diverticulate to coralloid cheilocystidia, moderately thick-walled caulocystidia with obtuse apex, dextrinoid hyphae in cortex of stipe, and gray-brown pileal and hymenophoral trama. Color images of basidiomata and microscopic elements accompany the description. Gymnopus fuscotramus is compared with similar species and its systematic position is also inferred using the ITS rDNA sequence data. Key words — Basidiomycota, biodiversity, Omphalotaceae, taxonomy Introduction During -
9B Taxonomy to Genus
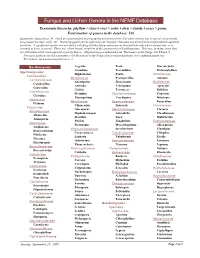
Fungus and Lichen Genera in the NEMF Database Taxonomic hierarchy: phyllum > class (-etes) > order (-ales) > family (-ceae) > genus. Total number of genera in the database: 526 Anamorphic fungi (see p. 4), which are disseminated by propagules not formed from cells where meiosis has occurred, are presently not grouped by class, order, etc. Most propagules can be referred to as "conidia," but some are derived from unspecialized vegetative mycelium. A significant number are correlated with fungal states that produce spores derived from cells where meiosis has, or is assumed to have, occurred. These are, where known, members of the ascomycetes or basidiomycetes. However, in many cases, they are still undescribed, unrecognized or poorly known. (Explanation paraphrased from "Dictionary of the Fungi, 9th Edition.") Principal authority for this taxonomy is the Dictionary of the Fungi and its online database, www.indexfungorum.org. For lichens, see Lecanoromycetes on p. 3. Basidiomycota Aegerita Poria Macrolepiota Grandinia Poronidulus Melanophyllum Agaricomycetes Hyphoderma Postia Amanitaceae Cantharellales Meripilaceae Pycnoporellus Amanita Cantharellaceae Abortiporus Skeletocutis Bolbitiaceae Cantharellus Antrodia Trichaptum Agrocybe Craterellus Grifola Tyromyces Bolbitius Clavulinaceae Meripilus Sistotremataceae Conocybe Clavulina Physisporinus Trechispora Hebeloma Hydnaceae Meruliaceae Sparassidaceae Panaeolina Hydnum Climacodon Sparassis Clavariaceae Polyporales Gloeoporus Steccherinaceae Clavaria Albatrellaceae Hyphodermopsis Antrodiella -
Chemical Elements in Ascomycetes and Basidiomycetes
Chemical elements in Ascomycetes and Basidiomycetes The reference mushrooms as instruments for investigating bioindication and biodiversity Roberto Cenci, Luigi Cocchi, Orlando Petrini, Fabrizio Sena, Carmine Siniscalco, Luciano Vescovi Editors: R. M. Cenci and F. Sena EUR 24415 EN 2011 1 The mission of the JRC-IES is to provide scientific-technical support to the European Union’s policies for the protection and sustainable development of the European and global environment. European Commission Joint Research Centre Institute for Environment and Sustainability Via E.Fermi, 2749 I-21027 Ispra (VA) Italy Legal Notice Neither the European Commission nor any person acting on behalf of the Commission is responsible for the use which might be made of this publication. Europe Direct is a service to help you find answers to your questions about the European Union Freephone number (*): 00 800 6 7 8 9 10 11 (*) Certain mobile telephone operators do not allow access to 00 800 numbers or these calls may be billed. A great deal of additional information on the European Union is available on the Internet. It can be accessed through the Europa server http://europa.eu/ JRC Catalogue number: LB-NA-24415-EN-C Editors: R. M. Cenci and F. Sena JRC65050 EUR 24415 EN ISBN 978-92-79-20395-4 ISSN 1018-5593 doi:10.2788/22228 Luxembourg: Publications Office of the European Union Translation: Dr. Luca Umidi © European Union, 2011 Reproduction is authorised provided the source is acknowledged Printed in Italy 2 Attached to this document is a CD containing: • A PDF copy of this document • Information regarding the soil and mushroom sampling site locations • Analytical data (ca, 300,000) on total samples of soils and mushrooms analysed (ca, 10,000) • The descriptive statistics for all genera and species analysed • Maps showing the distribution of concentrations of inorganic elements in mushrooms • Maps showing the distribution of concentrations of inorganic elements in soils 3 Contact information: Address: Roberto M. -

Fungi of the Fortuna Forest Reserve: Taxonomy and Ecology with Emphasis on Ectomycorrhizal Communities
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.16.045724; this version posted April 18, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Fungi of the Fortuna Forest Reserve: Taxonomy and ecology with emphasis on ectomycorrhizal communities Adriana Corrales1 and Clark L. Ovrebo2 1 Department of Biology, Faculty of Natural Sciences, Universidad del Rosario. Bogota, 111221, Colombia. 2 Department of Biology, University of Central Oklahoma. Edmond, OK. USA. ABSTRACT Panamanian montane forests harbor a high diversity of fungi, particularly of ectomycorrhizal (ECM) fungi, however their taxonomy and diversity patterns remain for the most part unexplored. Here we present state of the art fungal taxonomy and diversity patterns at Fortuna Forest Reserve based on morphological and molecular identification of over 1,000 fruiting body collections of macromycetes made over a period of five years. We compare these new results with previously published work based on environmental sampling of Oreomunnea mexicana root tips. We compiled a preliminary list of species and report 22 new genera and 29 new fungal species for Panama. Based on fruiting body collection data we compare the species composition of ECM fungal communities associated with Oreomunnea stands across sites differing in soil fertility and amount of rainfall. We also examine the effect of a long-term nitrogen addition treatment on the fruiting body production of ECM fungi. Finally, we discuss the biogeographic importance of Panama collections which fill in the knowledge gap of ECM fungal records between Costa Rica and Colombia.