Interagency Autism Coordinating Committee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder
Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Edwards, Laura Ann. 2015. Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder. Doctoral dissertation, Harvard Graduate School of Education. Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:23519638 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder Laura Ann Edwards Tina A. Grotzer Charles A. Nelson Gigi Luk A Thesis Presented to the Faculty of the Graduate School of Education of Harvard University in Partial Fulfillment of the Requirements for the Degree of Doctor of Education 2015 ii © 2015 Laura Ann Edwards All Rights Reserved iii Acknowledgements This dissertation would not have been possible without the contributions of many, throughout my doctoral career. I would first and foremost like to thank the members of my ad hoc committee—Chuck Nelson, Tina Grotzer, and Gigi Luk. Chuck has been my day-to-day mentor since I arrived at Harvard. He has scaffolded my development as a researcher, enabling me to operate autonomously, while always being available to provide support and advice. I am indebted to him for his prompt and thoughtful attention to me, and his mentorship in my past, current, and future academic endeavors. -

May 9-12 Rotterdam Netherlands
2018 ANNUAL MEETING MAY 9-12 ROTTERDAM NETHERLANDS PROGRAM BOOK www.autism-insar.org INSAR 2018 Sponsors We thank the following organizations for their generous support of the INSAR Annual Meeting. Platinum Sponsor Level Gold Sponsor Level Silver Sponsor Level Autism Science Foundation Hilibrand Foundation Nancy Lurie Marks Family Foundation TABLE OF CONTENTS Sponsorship .................................Inside Front Cover TABLE OF CONTENTS Special Interest Groups Schedule .......................... 6 Speaker Ready Room ............................................ 6 De Doelen Floor Plans ........................................ 7-9 Meeting Information Schedule-At-A-Glance .................................... 10-12 In-Conjunction Events .................................... 13-14 Keynote Speakers .............................................. 15 Awardees ..................................................... 16-19 INSAR MISSION Acknowledgments .......................................... 20-21 STATEMENT To promote the highest quality INSAR Summer Institute .................................... 22 research in order to improve the Abstract Author Index ...................................... 134 lives of people affected by autism. General Information .......................................... 208 Exhibitors ....................................................... 210 Strategic Initiatives Setting the Bar: Increase the quality, AM diversity and relevance of research promoted through annual meetings, journal, Keynote Address ............................................... -

Spirituality in the Context of Nonverbal Autism
Spirituality in the Context of Nonverbal Autism Author Hills, Karenne J. Published 2019-10-08 Thesis Type Thesis (PhD Doctorate) School School of Human Serv & Soc Wrk DOI https://doi.org/10.25904/1912/880 Copyright Statement The author owns the copyright in this thesis, unless stated otherwise. Downloaded from http://hdl.handle.net/10072/388655 Griffith Research Online https://research-repository.griffith.edu.au Spirituality in the Context of Nonverbal Autism Karenne Joy Hills Bachelor of Nursing GU – 1997 Bachelor of Counselling UNE – 2001 Master of Counselling CHC – 2012 Graduate Certificate Couple Counselling CHC – 2013 School of Human Services and Social Work Faculty of Health Griffith University Submitted in fulfilment of the requirements of the degree of Doctor of Philosophy April 2019 ii KEYWORDS Spirituality; Nonverbal Autism; Theology; Imago Dei; Language; Silence; Mystery; Inclusion iii ABSTRACT This thesis explored the spirituality of people who are not able to typically express a belief or understanding of traditional religious doctrine. The study is underpinned by the theological premise that honours the inherent value and worth of all human beings as carriers of the Imago Dei – created in the image of God. When the life context of someone prevents the intellectual, communicative or social ingredients generally associated with traditional spiritual or religious involvement, the possibility of a different experience or expression must be considered. This research explored such a possibility through the context of people diagnosed with severe autism, who do not communicate by the use of oral speech. People with nonverbal autism are identified as being on the severe end of the autism spectrum. -
Study of Nonverbal Autism Must Go Beyond Words, Experts Say
Spectrum | Autism Research News https://www.spectrumnews.org NEWS Study of nonverbal autism must go beyond words, experts say BY SARAH DEWEERDT 2 SEPTEMBER 2013 Sound out: Interactive devices do not hinder nonverbal children with autism from learning to speak, and may even help them. Roughly 25 percent of people with autism speak few or no words. A generation ago, that figure was closer to 50 percent. Most researchers agree that the decline is due to the recognition of more people with milder forms of autism, as well as to the advent of early intervention programs that have helped more children develop language than in the past. “One of the primary success stories of early interventions is that they promote language development,” says Helen Tager-Flusberg, director of the Research on Autism & Developmental Disorders program at Boston University. “Nevertheless,” she says, “there are clearly individuals who are diagnosed early, do have access to high-quality interventions, and still fail to acquire spoken language.” Paradoxically, many researchers now argue that in order to better understand and treat this subgroup of nonverbal people with autism, the field needs to move beyond focusing on speech production. Emerging research suggests that seemingly unrelated issues, such as motor skills and joint attention, may instead be key. Language delay gets a lion’s share of the attention perhaps because it is often the first and most 1 / 4 Spectrum | Autism Research News https://www.spectrumnews.org compelling sign of autism. “Parents, pediatricians, psychologists — everyone, we all focus on word production,” says Joe McCleery, lecturer in developmental neuroscience at the University of Birmingham in the U.K. -

Vitamin D and Autism Spectrum Disorder: a Literature Review
nutrients Review Vitamin D and Autism Spectrum Disorder: A Literature Review Hajar Mazahery 1, Carlos A. Camargo Jr. 2, Cathryn Conlon 1, Kathryn L. Beck 1, Marlena C. Kruger 1 and Pamela R. von Hurst 1,* 1 Institute of Food Science and Technology—School of Food and Nutrition, Massey University, Palmerston North 4474, New Zealand; [email protected] (H.M.); [email protected] (C.C.); [email protected] (K.L.B.); [email protected] (M.C.K.) 2 Department of Emergency Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA 02114, USA; [email protected] * Correspondence: [email protected]; Tel.: +64-9-213-6657 Received: 14 March 2016; Accepted: 14 April 2016; Published: 21 April 2016 Abstract: Low vitamin D status in early development has been hypothesised as an environmental risk factor for Autism Spectrum Disorder (ASD), given the concurrent increase in the prevalence of these two conditions, and the association of vitamin D with many ASD-associated medical conditions. Identification of vitamin D-ASD factors may provide indications for primary and secondary prevention interventions. We systematically reviewed the literature for studies on vitamin D-ASD relationship, including potential mechanistic pathways. We identified seven specific areas, including: latitude, season of conception/birth, maternal migration/ethnicity, vitamin D status of mothers and ASD patients, and vitamin D intervention to prevent and treat ASD. Due to differences in the methodological procedures and inconsistent results, drawing conclusions from the first three areas is difficult. Using a more direct measure of vitamin D status—that is, serum 25(OH)D level during pregnancy or childhood—we found growing evidence for a relationship between vitamin D and ASD. -

Download the Book of Abstracts
12th Autism-Europe International Congress September 13-15th 2019 ABSTRACT BOOK TABLE OF CONTENTS Foreword by Zsuzsanna Szilvásy - President of Autism-Europe p. 1 Foreword by Danièle Langloys - President of Autisme France p. 1 Scientific Committee p. 2 Honorary Scientific Committee p. 3 Index by session p. 4 First author index p.17 Index by Keywords p.26 Abstracts p.28 We are glad to invite you to the 12th In- how to shape better lives for autistic people. have happy and fulfilling lives. ternational Congress of Autism-Europe , which is organized in cooperation with Au- On the occasion of this three-day event With kindest regards, tisme France, in the beautiful city of Nice. people from all over the world will come Our congresses are held every three years, together to share the most recent deve- and we are delighted to be back in France, lopments across the field of autism. The 36 years after the congress of Paris. It will congress will address a wide range of is- be a great opportunity to take stock of the sues, including: diagnostic and assess- progress achieved and look at the opportu- ment, language and communication, ac- nities ahead. cess to education, employment, research and ethics, gender and sexuality, inclusion The 2019 congress’ motto is “A new Dyna- and community living, mental and physical mic for Change and Inclusion”, in keeping health, interventions, strategic planning with our aspiration that international scienti- and coordination of services as well as fic research on autism should be translated rights and participation. into concrete changes and foster social in- clusion for autistic people of all ages and We hope you will enjoy this Congress, needs. -

Accounting for the Preference for Literal Meanings in ASC
Accounting for the preference for literal meanings in ASC Abstract Impairments in pragmatic abilities, that is, difficulties with appropriate use and interpretation of language – in particular, non-literal uses of language – are considered a hallmark of Autism Spectrum Conditions (ASC). Despite considerable research attention, these pragmatic difficulties are poorly understood. In this paper, we discuss and evaluate existing hypotheses regarding the literalism of ASC individuals, that is, their tendency for literal interpretations of non-literal communicative intentions, and link them to accounts of pragmatic development in neurotypical children. We present evidence that reveals a developmental stage at which neurotypical children also have a tendency for literal interpretations and provide a possible explanation for such behaviour, one that links it to other behavioural, rule-following, patterns typical of that age. We then discuss extant evidence that shows that strict adherence to rules is also a widespread feature in ASC, and suggest that literalism might be linked to such rule- following behaviour. 1. Introduction What a speaker means by an utterance typically goes beyond the literal meanings of the words and sentences she has used. A key assumption underlying contemporary theories of human communication is that appropriate use and interpretation of language involves pragmatics skills – that is, the inferential capacities that enable us to bridge the gap between linguistic (literal/conventional) meanings and speaker meanings in context (see, e.g., Carston, 2002; Sperber & Wilson, 1986/1995). Impairments in such pragmatic reasoning abilities, that is, difficulties with appropriate use and interpretation of language, are considered a hallmark of Autism Spectrum Conditions (ASC) (Tager-Flusberg, Paul, & Lord, 2005). -
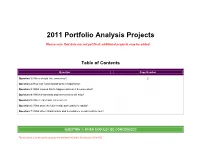
2011 Portfolio Analysis Projects
2011 Portfolio Analysis Projects Please note that data are not yet final; additional projects may be added. Table of Contents Question Page Number Question 1: When should I be concerned? 2 Question 2: How can I understand what is happening? Question 3: What caused this to happen and can it be prevented? Question 4: Which treatments and interventions will help? Question 5: Where can I turn for services? Question 6: What does the future hold, particularly for adults? Question 7: What other infrastructure and surveillance needs must be met? QUESTION 1: WHEN SHOULD I BE CONCERNED? This document is for discussion purposes only and does not reflect the decisions of the IACC 1.S.A Develop, with existing tools, at least one efficient diagnostic instrument (i.e., briefer, less time intensive) that is valid in diverse populations for use in large-scale studies by 2011. IACC Recommended Budget: $5,300,000 over 2 years. Project Title Principal Investigator Institution Funding Funder Biomarkers and diagnostics for ASD Bahn, Sabine Institute of Biotechnology $149,600 Autism Speaks Quantitative analysis of craniofacial dysmorphology in University of Massachusetts Deutsch, Curtis $137,861 Simons Foundation autism Medical School National Institutes Early detection of pervasive developmental disorders Fein, Deborah University of Connecticut $1,025,577 of Health Improving accuracy and accessibility of early autism Howard, National Institutes Total Child Health, Inc. $518,904 screening Barbara of Health Assessing the accuracy of rapid phenotyping of Law, Paul Kennedy Krieger Institute $ 124998 Autism Speaks nonverbal autistic children Autism dysmorphology measure validity study Miles, Judith University of Missouri $195,570 Simons Foundation Southwestern Autism Southwest Autism Validation of a screening questionnaire for ASD in Smith, Research & Resource Center $0 Research & older children Christopher (SARRC) Resource Center Multimedia tool for psychology graduate student ASD Strickland, National Institutes Virtual Reality Aids, Inc. -

May 9-12 Rotterdam Netherlands
2018 ANNUAL MEETING MAY 9-12 ROTTERDAM NETHERLANDS PROGRAM BOOK www.autism-insar.org INSAR 2018 Sponsors We thank the following organizations for their generous support of the INSAR Annual Meeting. Platinum Sponsor Level Gold Sponsor Level Silver Sponsor Level Autism Science Foundation Hilibrand Foundation Nancy Lurie Marks Family Foundation TABLE OF CONTENTS Sponsorship .................................Inside Front Cover TABLE OF CONTENTS Special Interest Groups Schedule .......................... 6 Speaker Ready Room ............................................ 6 De Doelen Floor Plans ........................................ 7-9 Meeting Information Schedule-At-A-Glance .................................... 10-12 In-Conjunction Events .................................... 13-14 Keynote Speakers .............................................. 15 Awardees ..................................................... 16-19 INSAR MISSION Acknowledgments .......................................... 20-21 STATEMENT To promote the highest quality INSAR Summer Institute .................................... 22 research in order to improve the Abstract Author Index ...................................... 134 lives of people affected by autism. General Information .......................................... 208 Exhibitors ....................................................... 210 Strategic Initiatives Setting the Bar: Increase the quality, AM diversity and relevance of research promoted through annual meetings, journal, Keynote Address ............................................... -
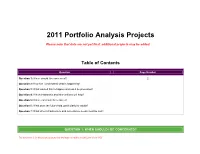
2011 Portfolio Analysis Projects
2011 Portfolio Analysis Projects Please note that data are not yet final; additional projects may be added. Table of Contents Question Page Number Question 1: When should I be concerned? 2 Question 2: How can I understand what is happening? Question 3: What caused this to happen and can it be prevented? Question 4: Which treatments and interventions will help? Question 5: Where can I turn for services? Question 6: What does the future hold, particularly for adults? Question 7: What other infrastructure and surveillance needs must be met? QUESTION 1: WHEN SHOULD I BE CONCERNED? This document is for discussion purposes only and does not reflect the decisions of the IACC 1.S.A Develop, with existing tools, at least one efficient diagnostic instrument (i.e., briefer, less time intensive) that is valid in diverse populations for use in large-scale studies by 2011. IACC Recommended Budget: $5,300,000 over 2 years. Project Title Principal Investigator Institution Funding Funder Biomarkers and diagnostics for ASD Bahn, Sabine Institute of Biotechnology $149,600 Autism Speaks Quantitative analysis of craniofacial dysmorphology in University of Massachusetts Deutsch, Curtis $137,861 Simons Foundation autism Medical School National Institutes Early detection of pervasive developmental disorders Fein, Deborah University of Connecticut $1,025,577 of Health Improving accuracy and accessibility of early autism Howard, National Institutes Total Child Health, Inc. $518,904 screening Barbara of Health Assessing the accuracy of rapid phenotyping of Law, Paul Kennedy Krieger Institute $ 124998 Autism Speaks nonverbal autistic children Autism dysmorphology measure validity study Miles, Judith University of Missouri $195,570 Simons Foundation Southwestern Autism Southwest Autism Validation of a screening questionnaire for ASD in Smith, Research & Resource Center $0 Research & older children Christopher (SARRC) Resource Center Multimedia tool for psychology graduate student ASD Strickland, National Institutes Virtual Reality Aids, Inc. -

Managing Affective-Learning Through Intelligent Atoms and Smart Interactions
Managing Affective-learning THrough Intelligent atoms and Smart InteractionS D8.2 Report on Autism Spectrum Case pilots Workpackage WP8 – Pilots in Education Annaleda Mazzucato, Alessandra Fratejacci (FMD) Editor(s): Gosia Kwiatkowska (RIX@UEL) Marisé Gálvez Trigo, Penny Standen (UoN) Maria A. Blanco, Ana Cabero, Javier Torres(JCYL) Elena Milli, Stefano Cobello (PE) Marco Traversi (LCS) Ana Piñuela Marcos (ATOS) David Brown, Mohammad Taheri, Matthew Belmonte, Tom Hughes- Roberts, Helen Boulton (NTU) Responsible Partner: Fondazione Mondo Digitale Quality Reviewers Mohammad Taheri (NTU), Stefano Cobello (PE) Status-Version: Final – v1.0 Due Date: 30/11/2017 Submission Date 20/12/2017 EC Distribution: PU Abstract: This deliverable reports on the preparation, execution and evaluation of the MaTHiSiS Autism Spectrum Case assisted pilot. Keywords: Assisted Pilots; Autism Spectrum Case, Learning Graph, Smart Learning Atom, Learning Materials. Related Deliverable(s) D2.1 Formation of stakeholder groups; D2.2 Full scenarios of all use cases; D2.5 Evaluation strategy; D3.3 The MaTHiSiS Learning Graphs, D8.1 Report on Autism Spectrum Case pilots This document is issued within the frame and for the purpose of the MATHISIS project. This project has received funding from the European Union’s Horizon 2020 Programme (H2020-ICT-2015) under Grant Agreement No. 687772 D8.2 - Report on Autism Spectrum Case pilots Document History Version Date Change editors Changes 0.1 14/11/2017 Annaleda Mazzucato (FMD) Executive summary Introduction Case description and -

How Is Sex Related to Autism?
How is Sex Related to Autism? Meng-Chuan Lai Girton College University of Cambridge This dissertation is submitted for the degree of Doctor of Philosophy August 2011 Preface The works in this dissertation were carried out at the Autism Research Centre, Department of Psychiatry, University of Cambridge between October 2008 and August 2011, and was supported by funding from the Ministry of Education, Taiwan. Professor Simon Baron-Cohen acted as my primary supervisor and Professor John Suckling acted as co-supervisor. The dissertation is the result of my own work and includes nothing which is the outcome of work done in collaboration, except that the recruitment and testing of the male participants were carried out between July 2007 and November 2008 by the Medical Research Council Autism Imaging Multicentre Study (MRC AIMS) Consortium project. This dissertation is less than 60,000 words. Chapter 2 and parts of Chapter 1 are published in: Meng-Chuan Lai, Michael V. Lombardo, Greg Pasco, Amber N. V. Ruigrok, Sally J. Wheelwright, Susan A. Sadek, Bhismadev Chakrabarti, MRC AIMS Consortium and Simon Baron-Cohen. (2011). A behavioral comparison of male and female adults with high functioning autism spectrum conditions. PLoS ONE 6(6):e20835. Chapter 6 Study 1 is published in: Meng-Chuan Lai, Michael V. Lombardo, Bhismadev Chakrabarti, Susan A. Sadek, Greg Pasco, Sally J. Wheelwright, Edward T. Bullmore, Simon Baron-Cohen, MRC AIMS Consortium and John Suckling. (2010). A shift to randomness of brain oscillations in people with autism. Biological Psychiatry 68(12):1092-1099. i Chapter 3 is currently in preparation for publication as: Meng-Chuan Lai, Michael V.