Vitamin D and Autism Spectrum Disorder: a Literature Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder
Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Edwards, Laura Ann. 2015. Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder. Doctoral dissertation, Harvard Graduate School of Education. Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:23519638 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Neural Precursors of Language in Infants at High Risk for Autism Spectrum Disorder Laura Ann Edwards Tina A. Grotzer Charles A. Nelson Gigi Luk A Thesis Presented to the Faculty of the Graduate School of Education of Harvard University in Partial Fulfillment of the Requirements for the Degree of Doctor of Education 2015 ii © 2015 Laura Ann Edwards All Rights Reserved iii Acknowledgements This dissertation would not have been possible without the contributions of many, throughout my doctoral career. I would first and foremost like to thank the members of my ad hoc committee—Chuck Nelson, Tina Grotzer, and Gigi Luk. Chuck has been my day-to-day mentor since I arrived at Harvard. He has scaffolded my development as a researcher, enabling me to operate autonomously, while always being available to provide support and advice. I am indebted to him for his prompt and thoughtful attention to me, and his mentorship in my past, current, and future academic endeavors. -

May 9-12 Rotterdam Netherlands
2018 ANNUAL MEETING MAY 9-12 ROTTERDAM NETHERLANDS PROGRAM BOOK www.autism-insar.org INSAR 2018 Sponsors We thank the following organizations for their generous support of the INSAR Annual Meeting. Platinum Sponsor Level Gold Sponsor Level Silver Sponsor Level Autism Science Foundation Hilibrand Foundation Nancy Lurie Marks Family Foundation TABLE OF CONTENTS Sponsorship .................................Inside Front Cover TABLE OF CONTENTS Special Interest Groups Schedule .......................... 6 Speaker Ready Room ............................................ 6 De Doelen Floor Plans ........................................ 7-9 Meeting Information Schedule-At-A-Glance .................................... 10-12 In-Conjunction Events .................................... 13-14 Keynote Speakers .............................................. 15 Awardees ..................................................... 16-19 INSAR MISSION Acknowledgments .......................................... 20-21 STATEMENT To promote the highest quality INSAR Summer Institute .................................... 22 research in order to improve the Abstract Author Index ...................................... 134 lives of people affected by autism. General Information .......................................... 208 Exhibitors ....................................................... 210 Strategic Initiatives Setting the Bar: Increase the quality, AM diversity and relevance of research promoted through annual meetings, journal, Keynote Address ............................................... -

Interagency Autism Coordinating Committee
1 INTERAGENCY AUTISM COORDINATING COMMITTEE FULL COMMITTEE MEETING THURSDAY, July 22, 2021 The full Interagency Autism Coordinating Committee (IACC) convened virtually, at 2:00 p.m., Joshua Gordon, M.D., Ph.D., Chair, presiding. PRESENT: JOSHUA GORDON, M.D., Ph.D., Chair, IACC, Director, National Institute of Mental Health, (NIMH) SUSAN DANIELS, Ph.D., Executive Secretary, IACC, Office of Autism Research Coordination (OARC), NIMH COURTNEY FERRELL AKLIN, Ph.D., National Institutes of Health (NIH)(representing Francis Collins, M.D., Ph.D.) MARIA MERCEDES AVILA, Ph.D., M.S.W., M.Ed. University of Vermont SKYE BASS, L.C.S.W., Indian Health Service (IHS) DIANA BIANCHI, M.D., Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) SAMANTHA CRANE, J.D., Autistic Self Advocacy Network 2 PRESENT: (continued) AISHA DICKERSON, Ph.D., Johns Hopkins University TIFFANY FARCHIONE, M.D., U.S. Food and Drug Administration (FDA) MARIA FRYER, M.S., U.S. Department of Justice (DOJ) DAYANA GARCIA, M.Ed., Administration for Children and Families (ACF) DENA GASSNER, M.S.W., Adelphi University MORÉNIKE GIWA ONAIWU, M.A., Rice University ALYCIA HALLADAY, Ph.D., Autism Science Foundation CRAIG JOHNSON, B.A. Champions Foundation JENNIFER JOHNSON, Ed.D., Administration for Community Living (ACL) CINDY LAWLER, Ph.D., National Institute of Environmental Health Sciences (NIEHS) (representing Rick Woychik, Ph.D.) ALISON MARVIN, Ph.D., Social Security Administration (SSA) LINDSEY NEBEKER,B.A., Freelance Presenter/Trainer SCOTT PATTERSON, Ph.D., U.S. Department of Veterans Affairs (VA)(representing Matthew Miller, Ph.D., M.P.H.) VALERIE PARADIZ, Ph.D., Autism Speaks 3 PRESENT (continued) GEORGINA PEACOCK, M.D., M.P.H., F.A.A.P., Centers for Disease Control and Prevention (CDC) JENNY MAI PHAN, Ph.D., University of Wisconsin-Madison JOSEPH PIVEN, M.D., University of North Carolina-Chapel Hill JALYNN PRINCE, B.F.A., Madison House Autism Foundation LAUREN RAMOS, M.P.H., Health Resources and Services Administration (HRSA) SCOTT MICHAEL ROBERTSON, Ph.D., U.S. -

Spirituality in the Context of Nonverbal Autism
Spirituality in the Context of Nonverbal Autism Author Hills, Karenne J. Published 2019-10-08 Thesis Type Thesis (PhD Doctorate) School School of Human Serv & Soc Wrk DOI https://doi.org/10.25904/1912/880 Copyright Statement The author owns the copyright in this thesis, unless stated otherwise. Downloaded from http://hdl.handle.net/10072/388655 Griffith Research Online https://research-repository.griffith.edu.au Spirituality in the Context of Nonverbal Autism Karenne Joy Hills Bachelor of Nursing GU – 1997 Bachelor of Counselling UNE – 2001 Master of Counselling CHC – 2012 Graduate Certificate Couple Counselling CHC – 2013 School of Human Services and Social Work Faculty of Health Griffith University Submitted in fulfilment of the requirements of the degree of Doctor of Philosophy April 2019 ii KEYWORDS Spirituality; Nonverbal Autism; Theology; Imago Dei; Language; Silence; Mystery; Inclusion iii ABSTRACT This thesis explored the spirituality of people who are not able to typically express a belief or understanding of traditional religious doctrine. The study is underpinned by the theological premise that honours the inherent value and worth of all human beings as carriers of the Imago Dei – created in the image of God. When the life context of someone prevents the intellectual, communicative or social ingredients generally associated with traditional spiritual or religious involvement, the possibility of a different experience or expression must be considered. This research explored such a possibility through the context of people diagnosed with severe autism, who do not communicate by the use of oral speech. People with nonverbal autism are identified as being on the severe end of the autism spectrum. -
Study of Nonverbal Autism Must Go Beyond Words, Experts Say
Spectrum | Autism Research News https://www.spectrumnews.org NEWS Study of nonverbal autism must go beyond words, experts say BY SARAH DEWEERDT 2 SEPTEMBER 2013 Sound out: Interactive devices do not hinder nonverbal children with autism from learning to speak, and may even help them. Roughly 25 percent of people with autism speak few or no words. A generation ago, that figure was closer to 50 percent. Most researchers agree that the decline is due to the recognition of more people with milder forms of autism, as well as to the advent of early intervention programs that have helped more children develop language than in the past. “One of the primary success stories of early interventions is that they promote language development,” says Helen Tager-Flusberg, director of the Research on Autism & Developmental Disorders program at Boston University. “Nevertheless,” she says, “there are clearly individuals who are diagnosed early, do have access to high-quality interventions, and still fail to acquire spoken language.” Paradoxically, many researchers now argue that in order to better understand and treat this subgroup of nonverbal people with autism, the field needs to move beyond focusing on speech production. Emerging research suggests that seemingly unrelated issues, such as motor skills and joint attention, may instead be key. Language delay gets a lion’s share of the attention perhaps because it is often the first and most 1 / 4 Spectrum | Autism Research News https://www.spectrumnews.org compelling sign of autism. “Parents, pediatricians, psychologists — everyone, we all focus on word production,” says Joe McCleery, lecturer in developmental neuroscience at the University of Birmingham in the U.K. -

Download the Book of Abstracts
12th Autism-Europe International Congress September 13-15th 2019 ABSTRACT BOOK TABLE OF CONTENTS Foreword by Zsuzsanna Szilvásy - President of Autism-Europe p. 1 Foreword by Danièle Langloys - President of Autisme France p. 1 Scientific Committee p. 2 Honorary Scientific Committee p. 3 Index by session p. 4 First author index p.17 Index by Keywords p.26 Abstracts p.28 We are glad to invite you to the 12th In- how to shape better lives for autistic people. have happy and fulfilling lives. ternational Congress of Autism-Europe , which is organized in cooperation with Au- On the occasion of this three-day event With kindest regards, tisme France, in the beautiful city of Nice. people from all over the world will come Our congresses are held every three years, together to share the most recent deve- and we are delighted to be back in France, lopments across the field of autism. The 36 years after the congress of Paris. It will congress will address a wide range of is- be a great opportunity to take stock of the sues, including: diagnostic and assess- progress achieved and look at the opportu- ment, language and communication, ac- nities ahead. cess to education, employment, research and ethics, gender and sexuality, inclusion The 2019 congress’ motto is “A new Dyna- and community living, mental and physical mic for Change and Inclusion”, in keeping health, interventions, strategic planning with our aspiration that international scienti- and coordination of services as well as fic research on autism should be translated rights and participation. into concrete changes and foster social in- clusion for autistic people of all ages and We hope you will enjoy this Congress, needs. -
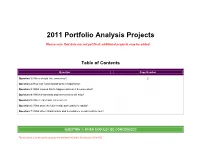
2011 Portfolio Analysis Projects
2011 Portfolio Analysis Projects Please note that data are not yet final; additional projects may be added. Table of Contents Question Page Number Question 1: When should I be concerned? 2 Question 2: How can I understand what is happening? Question 3: What caused this to happen and can it be prevented? Question 4: Which treatments and interventions will help? Question 5: Where can I turn for services? Question 6: What does the future hold, particularly for adults? Question 7: What other infrastructure and surveillance needs must be met? QUESTION 1: WHEN SHOULD I BE CONCERNED? This document is for discussion purposes only and does not reflect the decisions of the IACC 1.S.A Develop, with existing tools, at least one efficient diagnostic instrument (i.e., briefer, less time intensive) that is valid in diverse populations for use in large-scale studies by 2011. IACC Recommended Budget: $5,300,000 over 2 years. Project Title Principal Investigator Institution Funding Funder Biomarkers and diagnostics for ASD Bahn, Sabine Institute of Biotechnology $149,600 Autism Speaks Quantitative analysis of craniofacial dysmorphology in University of Massachusetts Deutsch, Curtis $137,861 Simons Foundation autism Medical School National Institutes Early detection of pervasive developmental disorders Fein, Deborah University of Connecticut $1,025,577 of Health Improving accuracy and accessibility of early autism Howard, National Institutes Total Child Health, Inc. $518,904 screening Barbara of Health Assessing the accuracy of rapid phenotyping of Law, Paul Kennedy Krieger Institute $ 124998 Autism Speaks nonverbal autistic children Autism dysmorphology measure validity study Miles, Judith University of Missouri $195,570 Simons Foundation Southwestern Autism Southwest Autism Validation of a screening questionnaire for ASD in Smith, Research & Resource Center $0 Research & older children Christopher (SARRC) Resource Center Multimedia tool for psychology graduate student ASD Strickland, National Institutes Virtual Reality Aids, Inc. -

May 9-12 Rotterdam Netherlands
2018 ANNUAL MEETING MAY 9-12 ROTTERDAM NETHERLANDS PROGRAM BOOK www.autism-insar.org INSAR 2018 Sponsors We thank the following organizations for their generous support of the INSAR Annual Meeting. Platinum Sponsor Level Gold Sponsor Level Silver Sponsor Level Autism Science Foundation Hilibrand Foundation Nancy Lurie Marks Family Foundation TABLE OF CONTENTS Sponsorship .................................Inside Front Cover TABLE OF CONTENTS Special Interest Groups Schedule .......................... 6 Speaker Ready Room ............................................ 6 De Doelen Floor Plans ........................................ 7-9 Meeting Information Schedule-At-A-Glance .................................... 10-12 In-Conjunction Events .................................... 13-14 Keynote Speakers .............................................. 15 Awardees ..................................................... 16-19 INSAR MISSION Acknowledgments .......................................... 20-21 STATEMENT To promote the highest quality INSAR Summer Institute .................................... 22 research in order to improve the Abstract Author Index ...................................... 134 lives of people affected by autism. General Information .......................................... 208 Exhibitors ....................................................... 210 Strategic Initiatives Setting the Bar: Increase the quality, AM diversity and relevance of research promoted through annual meetings, journal, Keynote Address ............................................... -
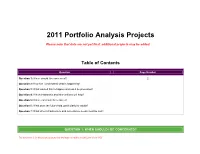
2011 Portfolio Analysis Projects
2011 Portfolio Analysis Projects Please note that data are not yet final; additional projects may be added. Table of Contents Question Page Number Question 1: When should I be concerned? 2 Question 2: How can I understand what is happening? Question 3: What caused this to happen and can it be prevented? Question 4: Which treatments and interventions will help? Question 5: Where can I turn for services? Question 6: What does the future hold, particularly for adults? Question 7: What other infrastructure and surveillance needs must be met? QUESTION 1: WHEN SHOULD I BE CONCERNED? This document is for discussion purposes only and does not reflect the decisions of the IACC 1.S.A Develop, with existing tools, at least one efficient diagnostic instrument (i.e., briefer, less time intensive) that is valid in diverse populations for use in large-scale studies by 2011. IACC Recommended Budget: $5,300,000 over 2 years. Project Title Principal Investigator Institution Funding Funder Biomarkers and diagnostics for ASD Bahn, Sabine Institute of Biotechnology $149,600 Autism Speaks Quantitative analysis of craniofacial dysmorphology in University of Massachusetts Deutsch, Curtis $137,861 Simons Foundation autism Medical School National Institutes Early detection of pervasive developmental disorders Fein, Deborah University of Connecticut $1,025,577 of Health Improving accuracy and accessibility of early autism Howard, National Institutes Total Child Health, Inc. $518,904 screening Barbara of Health Assessing the accuracy of rapid phenotyping of Law, Paul Kennedy Krieger Institute $ 124998 Autism Speaks nonverbal autistic children Autism dysmorphology measure validity study Miles, Judith University of Missouri $195,570 Simons Foundation Southwestern Autism Southwest Autism Validation of a screening questionnaire for ASD in Smith, Research & Resource Center $0 Research & older children Christopher (SARRC) Resource Center Multimedia tool for psychology graduate student ASD Strickland, National Institutes Virtual Reality Aids, Inc. -

How to Talk to an Austistic Kid Free
FREE HOW TO TALK TO AN AUSTISTIC KID PDF Daniel Stefanski | 48 pages | 01 Apr 2011 | Free Spirit Publishing Inc.,U.S. | 9781575423654 | English | Minneapolis, United States What to Say: Answers for Kids With Autism (for Kids) - Nemours KidsHealth Approximately one third of children with autism are nonverbal. This means that they never learn to speak more than a few words in their lives. The primary identifying aspect for nonverbal autism is to determine whether or not the individual speaks clearly or without interference. Although there are individuals with autism that may struggle How to Talk to an Austistic Kid having a back-and-forth conversation, these are not nonverbal autistic people. Autistic children could lose the ability to speak later on as the symptoms of the disorder worsen over time. The individual could also be suffering from apraxia. This can cause the person to not be able to say what they actually want to say. Autistic individuals could also suffer from echolaliawhich is repetition of words and phrases. This could also hinder clear communication. Read: How to treat Echolalia in a Child with Autism. Social symptoms: Social interaction difficulties are a hallmark symptom for autism spectrum disorder. Individuals generally avoid eye contact. These could cause the individual to feel left How to Talk to an Austistic Kid and isolated, and may lead depression. Developmental symptoms: Each individual is unique. Every autistic person develops at a different rate. While a child can develop at a typical rate, their developmental progress could be delayed after the age of 2 or 3. -
Autism Building a Life Skills Toolkit
Building a Life Skills Tool Kit: Helping Prepare the Adolescent on the Autism Spectrum for Adult Life Kevin T. Blake, Ph.D., P.L.C. Tucson, AZ Cross Country Education Brentwood, TN Kevin T. Blake, Ph.D., P.L.C. www.drkevintblake.com 1 All Rights Reserved www.crosscountryeducation.com In the effort to comply with the appropriate boards/associations, I declare that I do have affiliations with or financial interest in a commercial organization that could pose a conflict of interest with my presentation. Building a Life Skills Tool Kit: Helping Prepare the Adolescent on the Autism Spectrum for Adult Life Kevin T. Blake, Ph.D., P.L.C. owns shares in the following companies: Amgen, Inc. Johnson & Johnson, Inc. Cross Country Education Leading the Way in Professional Development. www.CrossCountryEducation.com Kevin T. Blake, Ph.D., P.L.C. www.drkevintblake.com 2 All Rights Reserved www.crosscountryeducation.com Workshop Manual Layout • Workshop Slides (p. 1 - 121) • Helpful Resources: Websites, Books, etc. (p. 122-131) • Workshop Evaluation and scantron directions (p. 132-134) Kevin T. Blake, Ph.D., P.L.C. www.drkevintblake.com 3 All Rights Reserved www.crosscountryeducation.com Seminar Updates • Updates of this seminar, new information on Autism Spectrum Disorders, Learning Disorders, and AD/HD can be found at: www.drkevintblake.com Kevin T. Blake, Ph.D., P.L.C. www.drkevintblake.com 4 All Rights Reserved www.crosscountryeducation.com “Road Rules” and What To Expect 9:30 AM to 9:40 AM Break 11:30 AM to12:30 PM Lunch: On your own 2:00 PM to 2:10 PM Break 3:30 PM Conclusion I have 363 slides to present! Kevin T. -

The Autistic Spectrum: a Guide for Parents and Professionals Pdf, Epub, Ebook
THE AUTISTIC SPECTRUM: A GUIDE FOR PARENTS AND PROFESSIONALS PDF, EPUB, EBOOK Lorna Wing | 240 pages | 30 Jan 2003 | Little, Brown Book Group | 9781841196749 | English | London, United Kingdom The Autistic Spectrum: A Guide for Parents and Professionals PDF Book If a child is playing with cars on the floor, a therapist or parent will sit on the floor and play with the cars. Aug 26, Vic rated it it was amazing. Research found children understand pictures better after the age of three. However, it should be noted that both disorders are extremely rare and are the result of genetic mutations. Leave them in the comments! She has written around published papers, articles and book chapters on these areas, and been awarded multiple research grants to support her research. Most young children will imitate others, especially other children, and want to eat what they eat. Increase eye contact. This recognition of need has been found to be helpful when signposting to other professionals for support. If your child has nonverbal autism, working with a speech-language pathologist is essential for increasing communication with your child. Use goals and strategies taught at school and in therapy during your daily routines. We help kids speak no matter their speech challenges! When a child has a speech delay, parents often wonder whether the speech delay is due to autism. Over time, seconds of space in between your questions can lead to an answer from your child. What are some skills you recommend when anxiety is active for those with ARFID and autism regarding food? Individuals with autism and synesthesia report higher levels of sensory sensitivity.