Sonography of the Pelvic Infection Review Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -
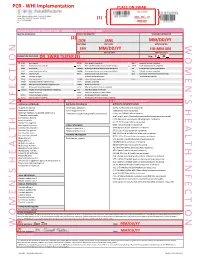
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -
Diagnostic Tests for Vaginosis/Vaginitis
Alberta Heritage Foundation for Medical Research Diagnostic tests for vaginosis/vaginitis Christa Harstall and Paula Corabian October 1998 HTA12 Diagnostic tests for vaginosis/vaginitis Christa Harstall and Paula Corabian October 1998 © Copyight Alberta Heritage Foundation for Medical Research, 1998 This Health Technology Assessment Report has been prepared on the basis of available information of which the Foundation is aware from public literature and expert opinion, and attempts to be current to the date of publication. The report has been externally reviewed. Additional information and comments relative to the Report are welcome, and should be sent to: Director, Health Technology Assessment Alberta Heritage Foundation for Medical Research 3125 Manulife Place, 10180 - 101 Street Edmonton Alberta T5J 3S4 CANADA Tel: 403-423-5727, Fax: 403-429-3509 This study is based, in part, on data provided by Alberta Health. The interpretation of the data in the report is that of the authors and does not necessarily represent the views of the Government of Alberta. ISBN 1-896956-15-7 Alberta's health technology assessment program has been established under the Health Research Collaboration Agreement between the Alberta Heritage Foundation for Medical Research and the Alberta Health Ministry. Acknowledgements The Alberta Heritage Foundation for Medical Research is most grateful to the following persons for their comments on the draft report and for provision of information. The views expressed in the final report are those of the Foundation. Dr. Jane Ballantine, Section of General Practice, Calgary Dr. Deirdre L. Church, Microbiology, Calgary Laboratory Services, Calgary Dr. Nestor N. Demianczuk, Royal Alexandra Hospital, Edmonton Dr. -

Remarks on Pelvic Peritonitis and Pelvic Cellulitis, with Illustrative Cases
Article IV.- Remarks on Pelvic Peritonitis and Pelvic Cellulitis, with Illustrative Cases. By Lauchlan Aitken, M.D. Rather moie than a year ago there appeared from the pen of a well- known of this a gynecologist city very able monograph on the two forms of pelvic inflammation whose names head this article; and it cannot have escaped the recollection of the reader that Dr M. Dun- can, adopting the nomenclature first proposed by Yirchow, has used on his different terms title-page1 than those older appellations I still to retain. Under these propose ^ circumstances I feel at to compelled least to attempt justify my preference for the original names: and I trust to be able to show that are they preferable to, and less con- others that fusing than, any have as yet been proposed, even though we cannot consider them absolutely perfect. 1 Treatise on A Practical Perimetritis and Parametritis (Edin. 1869). 1870.] DR LAUCI1LAN AITKEN ON PELVIC FERITONITIS, ETC. 889 Passing over, then, such terms as 'periuterine cellulitis or phleg- mons periuterins as bad compounds ; others, as inflammation of the broad ligaments, as too limited in meaning ; and others, again, as engorgement periutdrin, as only indicating one of the stages of the affection,?I shall endeavour as succinctly as possible to state my reasons for preferring the older names to those proposed by Virchow. ls?. The two Greek prepositions, peri and para, are employed somewhat arbitrarily to indicate inflammatory processes which are essentially distinct. I say arbitrarily, because I am not aware that para has been generally employed in the form of a compound to ex- press inflammation of the cellular tissue elsewhere.1 By those who remember that the cellular tissue not only separates the serous membrane from the uterus at that part where the cervix and body of the organ meet, but is even abundant there,2 perimetritis might readily be taken to indicate one of the varieties, though indeed not a in for which very common one, of pelvic cellulitis?a variety, fact, the term perimetric cellulitis has been proposed. -

The Relative Risk
Clinical Expert Series Pelvic Inflammatory Disease David E. Soper, MD Obstet Gynecol 2010;116(2) ACCME Accreditation The American College of Obstetricians and Gynecologists (ACOG) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. (Continuing medical education credit for “Pelvic Inflammatory Disease” will be available through August 2013.) AMA PRA Category 1 CreditTM and ACOG Cognate Credit The American College of Obstetricians and Gynecologists (ACOG) designates this educational activity for a maximum of 2 AMA PRA Category 1 CreditsTM or up to a maximum of 2 Category 1 ACOG cognate credits. Physicians should only claim credit commensurate with the extent of their participation in the activity. Disclosure Statement Current guidelines state that continuing medical education (CME) providers must ensure that CME activities are free from the control of any commercial interest. All authors, reviewers, and contributors have disclosed to the College all relevant financial relationships with any commercial interests. The authors, reviewers, and contributors declare that neither they nor any business associate nor any member of their immediate families has financial interest or other relationships with any manufacturer of products or any providers of services discussed in this program. Any conflicts have been resolved through group and outside review of all content. Before submitting this form, please print a completed copy as confirmation of your program participation. ACOG Fellows: To obtain credits, complete and return this form by clicking on “Submit” at the bottom of the page. Credit will be automatically recorded upon receipt and online transcripts will be updated twice monthly. -
Examination of Cases of Metritis
Examination of cases of Metritis VCP II, VCP 411 & VCP 511 Dr Ankesh Kumar Department of Veterinary Clinical complex, BVC, Patna One of the most significant causes of infertility in cattle is the metritis complex of diseases: retained fetal membranes, metritis, endometritis and pyometra. These diseases share common etiological factors, predispose to one another and, to a large extent, share common treatments. THE METRITIS COMPLEX : Metritis ; Endometritis ; Pyometra Metritis : Infection extends into deeper layers of the uterus, which may include extension though the serosa (Perimetritis) or into the broad ligament (Parametritis) There are systemic signs of illness, which may vary from relatively mild to vary severe: the life-threatening cases that occur within a few days of calving are often known as puerperal metritis. Endometritis : 1st, 2nd & 3rd Infection is confined to the endometrium and stratum spongiosum of the submucosa Affected cows show no systemic signs of illness Clinical signs are confined to the presence of purulent material (clinical endometritis) or the presence of leukocytes but no overt pus in uterine or cervical discharges. Mucus of estrum will be cloudy and milky instead of clear & translucent and contain many leucocytes. Bovine cervical mucus in pro-estrous may normally be slightly cloudy On rectal examination the uterus may feel slightly large, heavy, and thick walled The estrous cycle and period are usually normal in length but in occasional cases the cycle may be shortened to 8 to 12v days due to acute endometrial inflammation preventing development of a normal CL. Because of the abnormal endometrium and infection in the uterus the fertilized ovum may die and the cow again came into estrous. -

Severe Parametritis After Vaginal Delivery with Delayed Response to Broad Spectrum Antibiotics: a Case Report
Novelty in Biomedicine Case Report Severe Parametritis after Vaginal Delivery with Delayed Response to Broad Spectrum Antibiotics: A Case Report Laleh Eslamian1, Maasoumeh Saleh1*, Behnaz Nouri2 1Department of Obstetrics and Gynecology, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran 2Medical Student, Alborz University of Medical Science, Alborz, Iran Received: 03 January, 2021; Accepted: 20 May, 2021 Abstract Background: Postpartum infections, also known as puerperal fever, are bacterial infections of the female reproductive tract following childbirth or miscarriage. Symptoms usually include a fever greater than 38.0°C (100.4°F), chills, lower abdominal pain, and possibly bad-smelling vaginal discharge. It usually occurs after the first 24 hours and within the first ten days following delivery, but life-threatening infection may occur within hours of delivery. Cases Report: We reported a case of severe parametritis in the first 24 hours of delivery. Cesarean section is a risk factor for postpartum infections, and response to treatment is lower than vaginal delivery. Our case was a severe pelvic infection after vaginal delivery, and its risk factor was prolonged rupture of the membrane. Therefore, rapid diagnosis and treatment are necessary to prevent abscess formation and sepsis. Conclusion: In this case, rapid treatment with broad-spectrum antibiotics prevented abscess formation, sepsis, and hysterectomy. Keywords: Postpartum infections, Puerperal fever, Severe parametritis, Postpartum endometritis *Corresponding Author: Maasoumeh Saleh, Department of Obstetrics and Gynecology, Shariati Hospital, Jalal Al-Ahmad Ave., Tehran, Iran. Tel: (+98) 21 88220050, Email: [email protected] Please cite this article as: Eslamian L, Saleh M, Nouri B. Severe Parametritis after Vaginal Delivery with Delayed Response to Broad Spectrum Antibiotics: A Case Report t. -

Supplemental Information
ARTICLE Supplemental Information SUPPLEMENTAL TABLE 3 Diagnostic Codes for PID Code Description ICD-9 614.0 Acute salpingitis and oophoritis 614.2 Salpingitis and oophoritis not specified as acute, subacute, or chronic 614.3 Acute parametritis and pelvic cellulitis 614.4 Chronic or unspecified parametritis and pelvic cellulitis 614.8 Other specified inflammatory disease of female pelvic organs and tissues 614.9 Unspecified inflammatory disease of female pelvic organs and tissues 615.0 Acute inflammatory diseases of uterus, except cervix 615.9 Unspecified inflammatory disease of uterus 098.10 Gonococcal infection (acute) of upper genitourinary tract, site unspecified 098.16 Gonococcal endometritis (acute) 098.17 Gonococcal salpingitis, specified as acute 098.19 Other gonococcal infection (acute) of upper genitourinary tract 098.86 Gonococcal peritonitis 099.56 Other venereal diseases due to CT, peritoneum ICD-10 N70.01 Acute salpingitis N70.02 Acute oophoritis N70.03 Acute salpingitis and oophoritis N70.91 Salpingitis, unspecified N70.92 Oophoritis, unspecified N70.93 Salpingitis and oophoritis, unspecified N73.0 Acute parametritis and pelvic cellulitis N73.1 Chronic parametritis and pelvic cellulitis N73.2 Unspecified parametritis and pelvic cellulitis N73.8 Other specified female PIDs N73.9 Female PID, unspecified N71.0 Acute inflammatory disease of uterus N71.9 Inflammatory disease of uterus, unspecified A54.21 Gonococcal infection of kidney and ureter A54.24 Gonococcal female PID A54.29 Other gonococcal genitourinary infections A54.85 -
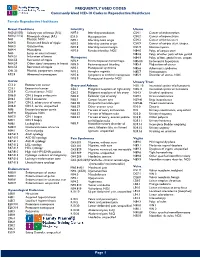
Commonly Used ICD-10 Codes in Reproductive Healthcare
FREQUENTLY USED CODES Commonly Used ICD-10 Codes in Reproductive Healthcare Female Reproductive Healthcare Breast Conditions Infertility Uterus N60.(01/02) Solitary cyst of breast (R/L) N97.0 Infertility-anovulation C54.1 Cancer of endometrium N60.(11/12) Fibrocystic change (R/L) E23.0 Hypopituarism C54.2 Cancer of myometrium N61 Mastitis, NOS N97.1 Infertility-tubal origin C54.3 Cancer of fundus uteri N64.0 Fissure and fistula of nipple N97.2 Infertility-uterine origin C54.9 Cancer of corpus uteri, unspec. N64.3 Galactorrhea N97.8 Infertility-cervical origin D25.9 Uterine myoma N64.4 Mastodynia N97.9 Female infertility, NOS N84.0 Polyp of corpus uteri N63 Lump or mass in breast N84.8 Polyp of other parts of fem genital N64.51 Induration of breast Menopause N84.9 Polyptract of fem. genital tract, unspec. N64.53 Retraction of nipple N92.4 Perimenopausal menorrhagia N85.00 Endometrial hyperplasia N64.59 Other signs/ symptoms in breast N95.0 Postmenopausal bleeding N85.4 Malposition of uterus N64.53 Retraction of nipple N95.1 Menopausal syndrome N85.6 Asherman’s syndrome O91.23 Mastitis, postpartum, unspec. N95.2 Atrophic vaginitis N85.7 Hematometra R92.8 Abnormal mammogram N95.8 Symptoms w artificial menopause N85.9 Disorder of uterus, NOS N95.9 Menopausal disorder NOS Cervix Urinary Tract C53.0 Endocervical cancer Ovary and Adnexa N30. 10 Interstitial cystitis w/o hematuria C53.1 Exocervical cancer C56.1 Malignant neoplasm of right ovary N30.11 Interstitial cystitis w/ hematuria C53.9 Cervical cancer, NOS C56.2 Malignant neoplasm of left -

Inflammatory Diseases of Female Pelvic Organs (N70-N77)
Inflammatory diseases of female pelvic organs (N70-N77) Excludes1: inflammatory diseases of female pelvic organs complicating: abortion or ectopic or molar pregnancy (O00-O07, O08.0) pregnancy, childbirth and the puerperium (O23.-, O75.3, O85, O86.-) N70 Salpingitis and oophoritis Includes: abscess (of) fallopian tube abscess (of) ovary pyosalpinx salpingo-oophoritis tubo-ovarian abscess tubo-ovarian inflammatory disease Use additional code (B95-B97), to identify infectious agent B95-B97 Excludes1: gonococcal infection (A54.24) tuberculous infection (A18.17) N70.0 Acute salpingitis and oophoritis N70.01 Acute salpingitis N70.02 Acute oophoritis N70.03 Acute salpingitis and oophoritis N70.1 Chronic salpingitis and oophoritis Hydrosalpinx N70.11 Chronic salpingitis N70.12 Chronic oophoritis N70.13 Chronic salpingitis and oophoritis N70.9 Salpingitis and oophoritis, unspecified N70.91 Salpingitis, unspecified N70.92 Oophoritis, unspecified N70.93 Salpingitis and oophoritis, unspecified N71 Inflammatory disease of uterus, except cervix Includes: endo (myo) metritis metritis myometritis pyometra uterine abscess Use additional code (B95-B97), to identify infectious agent B95-B97 Excludes1: hyperplastic endometritis (N85.0-) infection of uterus following delivery (O85, O86.-) N71.0 Acute inflammatory disease of uterus N71.1 Chronic inflammatory disease of uterus N71.9 Inflammatory disease of uterus, unspecified N72 Inflammatory disease of cervix uteri Includes: cervicitis (with or without erosion or ectropion) endocervicitis (with or without erosion or ectropion) exocervicitis (with or without erosion or ectropion) Use additional code (B95-B97), to identify infectious agent Excludes1: erosion and ectropion of cervix without cervicitis (N86) N73 Other female pelvic inflammatory diseases Use additional code (B95-B97), to identify infectious agent. -

FOURNIER GANGRENE in PUERPERAS AFTER CESAREAN SECTION Ryzhkov V
clinical case клинический случай © Group of authors, 2021 UDC 618.5-089.888.61:616-002 DOI – https://doi.org/10.14300/mnnc.2021.16050 ISSN – 2073-8137 FOURNIER GANGRENE IN PUERPERAS AFTER CESAREAN SECTION Ryzhkov V. V. 1, Gasparyan S. A. 1, Derevyanko T. I. 1, Kopylov A. V. 1, Papikova K. A. 1, Pydra A. R. 1, Pivovarova N. I. 2, Gordeeva L. P. 2 1 Stavropol State Medical University, Russian Federation 2 City clinical hospital of the emergency medical services, Stavropol, Russian Federation ГАНГРЕНА ФуРНЬЕ у РОДИЛЬНИЦЫ пОСЛЕ ОпЕРАЦИИ КЕСАРЕВА СЕЧЕНИЯ В. В. Рыжков 1, С. А. Гаспарян 1, Т. И. Деревянко 1, А. В. Копылов 1, К. А. папикова 1, А. Р. пыдра 1, Н. И. пивоварова 2, Л. п. Гордеева 2 1 Ставропольский государственный медицинский университет, Российская Федерация 2 Городская клиническая больница скорой медицинской помощи, Ставрополь, Российская Федерация Fournier gangrene is a form of necrotizing fasciitis that mainly affects men suffering from immunodeficiency after surgeries of the genitals and perineum. Literature data on the occurrence of this complication in women are rare, and there are no data in obstetric practice. Herein, we present a clinical case of severe sepsis with an unfavorable outcome owing to anterior abdominal wall phlegmon (Fournier phlegmon) in a puerperal woman after cesarean section. Keywords: cesarean section, fournier gangrene, sepsis В современных условиях гангрена Фурнье (эпифасциальный некроз) трактуется как специфическая форма некро- тизирующего фасциита, поражающая преимущественно мужчин, страдающих иммунодефицитом, после операций на половых органах и промежности. Данные литературы о возможности наличия этого осложнения у женщин единичные, а в акушерской практике отсутствуют.