Commonly Used ICD-10 Codes in Reproductive Healthcare
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Leucoplakic Vulva: Premalignant Determinants C
Henry Ford Hospital Medical Journal Volume 11 | Number 3 Article 3 9-1963 The Leucoplakic Vulva: Premalignant Determinants C. Paul Hodgkinson Roy B. P. Patton M. A. Ayers Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Hodgkinson, C. Paul; Patton, Roy B. P.; and Ayers, M. A. (1963) "The Leucoplakic Vulva: Premalignant Determinants," Henry Ford Hospital Medical Bulletin : Vol. 11 : No. 3 , 279-287. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol11/iss3/3 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. For more information, please contact [email protected]. Henry Ford Hosp. Med. Bull. Vol. 11, September, 1963 THE LEUCOPLAKIC VULVA Premalignant Determinants C. PAUL HODGKINSON, M.D.,* ROY B. P. PATTON, M.D., AND M. A. AYERS, M.D.* IN A PAPER proposing to discuss the leucoplakic vulva and any predisposing ten dency it may have to the development of squamous cell carcinoma, the term "pre malignant" has presumptuous connotations. This is presumptuous because it implies that more is known about cancer and its mode of development than can be supported by facts. What happens in the cell prior to the stage of carcinoma-in-situ is a burning and unsolved question in cancer research. How to detect and appraise the parameters of malignant potential is the essence of meaning connoted by the word "premalignant". -

Different Influences of Endometriosis and Pelvic Inflammatory Disease On
International Journal of Environmental Research and Public Health Article Different Influences of Endometriosis and Pelvic Inflammatory Disease on the Occurrence of Ovarian Cancer Jing-Yang Huang 1,2,†, Shun-Fa Yang 1,2 , Pei-Ju Wu 1,3,†, Chun-Hao Wang 4,†, Chih-Hsin Tang 5,6,7 and Po-Hui Wang 1,2,3,8,* 1 Institute of Medicine, Chung Shan Medical University, Taichung 402, Taiwan; [email protected] (J.-Y.H.); [email protected] (S.-F.Y.); [email protected] (P.-J.W.) 2 Department of Medical Research, Chung Shan Medical University Hospital, Taichung 402, Taiwan 3 Department of Obstetrics and Gynecology, Chung Shan Medical University Hospital, Taichung 402, Taiwan 4 Department of Medicine, National Taiwan University, Taipei 106, Taiwan; [email protected] 5 School of Medicine, China Medical University, Taichung 404, Taiwan; [email protected] 6 Chinese Medicine Research Center, China Medical University, Taichung 404, Taiwan 7 Department of Medical Laboratory Science and Biotechnology, College of Medical and Health Science, Asia University, Taichung 413, Taiwan 8 School of Medicine, Chung Shan Medical University, Taichung 402, Taiwan * Correspondence: [email protected] † Equal contributions as first authors. Abstract: To compare the rate and risk of ovarian cancer in patients with endometriosis or pelvic inflammatory disease (PID). A nationwide population cohort research compared the risk of ovarian cancer in 135,236 age-matched comparison females, 114,726 PID patients, and 20,510 endometriosis patients out of 982,495 females between 1 January 2002 and 31 December 2014 and ended on the date Citation: Huang, J.-Y.; Yang, S.-F.; of confirmation of ovarian cancer, death, or 31 December 2014. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -
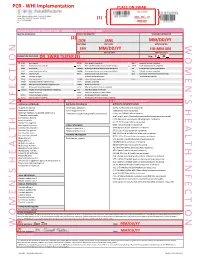
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Vaginitis and Abnormal Vaginal Bleeding
UCSF Family Medicine Board Review 2013 Vaginitis and Abnormal • There are no relevant financial relationships with any commercial Vaginal Bleeding interests to disclose Michael Policar, MD, MPH Professor of Ob, Gyn, and Repro Sciences UCSF School of Medicine [email protected] Vulvovaginal Symptoms: CDC 2010: Trichomoniasis Differential Diagnosis Screening and Testing Category Condition • Screening indications – Infections Vaginal trichomoniasis (VT) HIV positive women: annually – Bacterial vaginosis (BV) Consider if “at risk”: new/multiple sex partners, history of STI, inconsistent condom use, sex work, IDU Vulvovaginal candidiasis (VVC) • Newer assays Skin Conditions Fungal vulvitis (candida, tinea) – Rapid antigen test: sensitivity, specificity vs. wet mount Contact dermatitis (irritant, allergic) – Aptima TMA T. vaginalis Analyte Specific Reagent (ASR) Vulvar dermatoses (LS, LP, LSC) • Other testing situations – Vulvar intraepithelial neoplasia (VIN) Suspect trich but NaCl slide neg culture or newer assays – Psychogenic Physiologic, psychogenic Pap with trich confirm if low risk • Consider retesting 3 months after treatment Trichomoniasis: Laboratory Tests CDC 2010: Vaginal Trichomoniasis Treatment Test Sensitivity Specificity Cost Comment Aptima TMA +4 (98%) +3 (98%) $$$ NAAT (like GC/Ct) • Recommended regimen Culture +3 (83%) +4 (100%) $$$ Not in most labs – Metronidazole 2 grams PO single dose Point of care – Tinidazole 2 grams PO single dose •Affirm VP III +3 +4 $$$ DNA probe • Alternative regimen (preferred for HIV infected -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Localised Provoked Vestibulodynia (Vulvodynia): Assessment and Management
FOCUS Localised provoked vestibulodynia (vulvodynia): assessment and management Helen Henzell, Karen Berzins Background hronic vulvar pain (pain lasting more than 3–6 months, but often years) is common. It is estimated to affect 4–8% of Vulvodynia is a chronic vulvar pain condition. Localised C women at any one time and 10–20% in their lifetime.1–3 provoked vestibulodynia (LPV) is the most common subset Little attention has been paid to the teaching of this condition of vulvodynia, the hallmark symptom being pain on vaginal so medical practitioners may not recognise the symptoms, and penetration. Young women are predominantly affected. LPV diagnosis is often delayed.2 Community awareness is low, but is a hidden condition that often results in distress and shame, increasing with media attention. Women can be confused by the is frequently unrecognised, and women usually see a number symptoms and not know how to discuss vulvar pain. The onus is of health professionals before being diagnosed, which adds to on medical practitioners to enquire about vulvar pain, particularly their distress and confusion. pain with sex, when taking a sexual or reproductive health history. Objective Vulvodynia The aim of this article is to inform health providers about the Vulvodynia is defined by the International Society for the Study assessment and management of LPV. of Vulvovaginal Disease (ISSVD) as ‘chronic vulvar discomfort, most often described as burning pain, occurring in the absence Discussion of relevant findings or a specific, clinically identifiable, neurologic 4 Diagnosis is based on history. Examination is used to support disorder’. It is diagnosed when other causes of vulvar pain have the diagnosis. -
Effect of Educational Program on Vulvitis Prevention Among Nursing Students
American Journal of Nursing Science 2018; 7(6): 254-267 http://www.sciencepublishinggroup.com/j/ajns doi: 10.11648/j.ajns.20180706.19 ISSN: 2328-5745 (Print); ISSN: 2328-5753 (Online) Effect of Educational Program on Vulvitis Prevention Among Nursing Students Somaya Ouda Abd EL-Menim 1, Huda Abdalla Moursi 2, Ahlam Elahmady Mohamed Sarhan 2 1Obstetric and Woman Health Nursing, Faculty of Nursing, Benha University, Benha, Egypt 2Community Health Nursing, Benha University, Benha, Egypt Email address: To cite this article: Somaya Ouda Abd EL-Menim, Huda Abdalla Moursi, Ahlam Elahmady Mohamed Sarhan. Effect of Educational Program on Vulvitis Prevention among Nursing Students. American Journal of Nursing Science . Vol. 7, No. 6, 2018, pp. 254-267. doi: 10.11648/j.ajns.20180706.19 Received : November 7, 2018; Accepted : November 23, 2018; Published : January 2, 2019 Abstract: The aim of this study was to evaluate the effect of educational program on vulvitis prevention among nursing students Research design: A quasi-experimental design was utilized. Setting: This study was conducted at Faculty of Nursing, Benha University. Sample: convenient sample included two hundred and fifty nursing students female all enrolled in first academic years. Tools of data collection1) a structured interviewing sheet to collect data about socio-demographic characteristics, menstrual and gynecological history and knowledge of nursing students regarding vulvitis 2) reported practices assessment 3) modified likert scale for students' attitude regarding vulvitis. Results: there were general improvements regarding students' knowledge, attitude and practice regarding prevention of vulvitis with highly significant (P ≤ 0.001) difference after educational Program. The mother was the main sources of knowledge to students (60%). -

Cervical Polypectomy
Cervical Polypectomy Author: Consultant Department: Gynaecology/ Colposcopy Document Number: STHK1225 Version: 4 Review date: 01/10/2022 What is a polyp? Your doctor/nurse has advised you to have a polypectomy, which is the removal of a polyp. A polyp is a flesh-like structure (often described as looking like a cherry on a stalk or a skin tag), which can develop in many places in the body, including the cervix and uterus. It may have blood vessels running through it, which can often be the cause of bleeding. If it is thought the polyp is in your uterus, you will need to have a hysteroscopy (a procedure that uses a narrow camera to look inside the cavity of the uterus). This procedure is carried out as a gynaecology outpatient appointment at the Women’s Centre, and is performed in a special clinic in the Diagnostic Suite. You will receive a further appointment for this treatment and be given a different leaflet to explain the hysteroscopy procedure. If for any reason the polyp cannot be removed or fully removed during either of these treatments, the doctor will advise you of other options. Reasons for the procedure As you know you have been referred to the Colposcopy Clinic because you have a polyp on the cervix. Sometimes the cervical polyp is broad based, where it does not have a stalk but sits on the cervix. Often they cause no symptoms and are found as a result of other examinations. Polyps are usually benign (non-cancerous). Less than 1 % (1 in 100) may have pre-cancerous or cancerous changes within them; it is therefore advisable to have them removed. -

ICD-9-CM and ICD-10-CM Codes for Gynecology and Obstetrics
Diagnostic Services ICD-9-CM and ICD-10-CM Codes for Gynecology and Obstetrics ICD-9 ICD-10 ICD-9 ICD-10 Diagnoses Diagnoses Code Code Code Code Menstral Abnormalities 622.12 Moderate Dysplasia Of Cervix (CIN II) N87.2 625.3 Dysmenorrhea N94.6 Menopause 625.4 Premenstrual Syndrome N94.3 627.1 Postmenopausal Bleeding N95.0 626.0 Amenorrhea N91.2 627.2 Menopausal Symptoms N95.1 626.1 Oligomenorrhea N91.5 627.3 Senile Atrophic Vaginitis N95.2 626.2 Menorrhagia N92.0 627.4 Postsurgical Menopause N95.8 626.4 Irregular Menses N92.6 627.8 Perimenopausal Bleeding N95.8 626.6 Metrorrhagia N92.1 Abnormal Pap Smear Results 626.8 Dysfunctional Uterine Bleeding N93.8 795.00 Abnormal Pap Smear Result, Cervix R87.619 Disorders Of Genital Area 795.01 ASC-US, Cervix R87.610 614.9 Pelvic Inflammatory Disease (PID) N73.9 795.02 ASC-H, Cervix R87.611 616.1 Vaginitis, Unspecified N76.0 795.03 LGSIL, Cervix R87.612 616.2 Bartholin’s Cyst N75.0 795.04 HGSIL, Cervix R87.613 Cervical High-Risk HPV DNA 616.4 Vulvar Abscess N76.4 795.05 R87.810 Test Positive 616.5 Ulcer Of Vulva N76.6 Unsatisfactory Cervical 795.08 R87.615 616.89 Vaginal Ulcer N76.5 Cytology Sample 623.1 Leukoplakia Of Vagina N89.4 795.10 Abnormal Pap Smear Result, Vagina R87.628 Vaginal High-Risk HPV DNA 623.5 Vaginal Discharge N89.8 795.15 R87.811 Test Positive 623.8 Vaginal Bleeding N93.9 Disorders Of Uterus And Ovary 623.8 Vaginal Cyst N89.8 218.9 Uterine Fibroid/Leiomyoma D25.9 Noninflammatory Disorder 623.9 N89.9 Of Vagina 256.39 Ovarian Failure E28.39 624.8 Vulvar Lesion N90.89 256.9 Ovarian -

Having a Cervical Polypectomy
Gynaecology information Having a cervical polypectomy Introduction This leaflet gives you advice and information about having a cervical polypectomy (removal of polyps from the neck of the womb). Please read it before you go home so that you can have your questions answered before you leave. Feel free to discuss any questions or concerns with your nurse or telephone the Colposcopy Clinic on 0118 322 7197 or Sonning Ward on: 0118 322 7181. What is a cervical polypectomy and why do I need one? A cervical polyp is a small piece of tissue, usually on a stalk, that grows on the cervix (neck of the womb). Sometimes the cervical polyp is broad-based, where it does not have a stalk but sits on the cervix. Often they cause no symptoms and are found as a result of other examinations. Polyps are usually benign (non-cancerous). Less than 1% may have pre- cancerous or cancerous changes within them; it is therefore advisable to have them removed. A polypectomy is the removal of polyps. What are the risks of a cervical polypectomy? The procedure is very low risk, but may cause an infection or heavier bleeding. Before being sent for a polypectomy your doctor will have carried out a full pelvic examination, including an examination of your cervix using a speculum and you may have had an ultrasound or scan. What happens during a cervical polypectomy? This is normally done in the outpatient clinic. You will be asked to undress from the waist down and lie down on an examination couch. A speculum (the instrument used to open up the vagina) is passed into the vagina to expose the cervix. -

Menstrual Disorder
Menstrual Disorder N.SmidtN.Smidt--AfekAfek MD MHPE Lake Placid January 2011 The Menstrual Cycle two phases: follicular and luteal Normal Menstruation Regular menstruation 28+/28+/--7days;7days; Flow 4 --7d. 40ml loss Menstrual Disorders Abnormal Beleding –– Menorrhagia ,Metrorrhagia, Polymenorrhagia, Oligomenorrhea, Amenorrhea -- Dysmenorrhea –– Primary Dysmenorrhea, secondary Dysmenorrhea Pre Menstrual Tension –– PMD, PMDD Abnormal Uterine Beleeding Abnormal Bleeding Patterns Menorrhagia --bleedingbleeding more than 80ml or lasting >7days Metrorrhagia --bleedingbleeding between periods Polymenorrhagia -- menses less than 21d apart Oligomenorrhea --mensesmenses greater than 35 dasy apart. (in majority is anovulatory) Amenorrhea --NoNo menses for at least 6months Dysfunctional Uterine Bleeding Clinical term referring to abnormal bleeding that is not caused by identifiable gynecological pathology "Anovulatory Uterine Bleeding“ is usually the cause Diagnosis of exclusion Anovulatory Bleeding Most common at either end of reproductive life Chronic spotting Intermittent heavy bleeding Post Coital Bleeding Cervical ectropion ( most common in pregnancy) Cervicitis Vaginal or cervical malignancy Polyp Common Causes by age Neonatal Premenarchal ––EstrogenEstrogen withdrawal ––ForeignForeign body ––Trauma,Trauma, including sexual abuse Infection ––UrethralUrethral prolapse ––Sarcoma botryoides ––Ovarian tumor ––PrecociousPrecocious puberty Common Causes by age Early postmenarche Anovulation (hypothalamic immaturity) Bleeding