ICD-10 to Deaths During Pregnancy, Childbirth and the Puerperium: ICD-MM
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rapid Reduction of Maternal Mortality in Uganda and Zambia
Serbanescu et al. BMC Pregnancy and Childbirth (2017) 17:42 DOI 10.1186/s12884-017-1222-y RESEARCHARTICLE Open Access Rapid reduction of maternal mortality in Uganda and Zambia through the saving mothers, giving life initiative: results of year 1 evaluation Florina Serbanescu1,7,8* , Howard I. Goldberg1, Isabella Danel1, Tadesse Wuhib2,7, Lawrence Marum3,7, Walter Obiero2,7, James McAuley3,7, Jane Aceng4, Ewlyn Chomba5, Paul W. Stupp1,7 and Claudia Morrissey Conlon6,7 Abstract Background: Achieving maternal mortality reduction as a development goal remains a major challenge in most low-resource countries. Saving Mothers, Giving Life (SMGL) is a multi-partner initiative designed to reduce maternal mortality rapidly in high mortality settings through community and facility evidence-based interventions and district-wide health systems strengthening that could reduce delays to appropriate obstetric care. Methods: An evaluation employing multiple studies and data collection methods was used to compare baseline maternal outcomes to those during Year 1 in SMGL pilot districts in Uganda and Zambia. Studies include health facility assessments, pregnancy outcome monitoring, enhanced maternal mortality detection in facilities, and population-based investigation of community maternal deaths. Population-based evaluation used standard approaches and comparable indicators to measure outcome and impact, and to allow comparison of the SMGL implementation in unique country contexts. Results: The evaluation found a 30% reduction in the population-based maternal mortality ratio (MMR) in Uganda during Year 1, from 452 to 316 per 100,000 live births. The MMR in health facilities declined by 35% in each country (from 534 to 345 in Uganda and from 310 to 202 in Zambia). -

Central African Republic
CENTRAL AFRICAN REPUBLIC DEMOGRAPHICS AND BACKGROUND INFORMATION Total population (000) 4,487 (2011) Causes of under-five deaths, 2010 Under-five mortality rate Globally, undernutrition contributes to more than Deaths per 1,000 live births Total under-five population (000) 659 (2011) one third of child deaths 200 Total number of births (000) 156 (2011) Others 15% 169 Under-five mortality rate (per 1,000 live births) 164 (2011) 164 Measles 0% 160 Total number of under-five deaths (000) 25 (2011) Meningitis 2% Neonatal 28% HIV/AIDS 3% 120 Infant mortality rate (per 1,000 live births) 108 (2011) Injuries 3% Neonatal mortality rate (per 1,000 live births) 46 (2011) 80 HIV prevalence rate (15–49 years old, %) 4.6 (2011) 56 Population below international 63 (2008) Malaria 26% 40 MDG 4 poverty line of US$1.25 per day (%) Pneumonia 13% target GNI per capita (US$) 470 (2011) Diarrhoea 10% 0 1990 1995 2000 2005 2010 2015 Primary school net attendance ratio 47, 56 (2006) (% female, % male) Source: WHO/CHERG, 2012. Source: IGME, 2012. NUTRITIONAL STATUS Burden of malnutrition (2011) Stunted (under-fives, 000) 270 MDG 1 progress No progress Stunting country rank 50 Wasted (under-fives, 000) 46 Underweight (under-fives, 000) 158 Share of world stunting burden (%) <1% Severely wasted (under-fives, 000) 13 Overweight (under-fives, 000) 12 Stunting trends Stunting disparities Underweight trends Percentage of children <5 years old stunted Percentage of children <5 years old stunted, Percentage of children <5 years old underweight by selected background characteristics 100% 100% Boys 44 MDG 1: NO PROGRESS Girls 38 80% 80% Urban 38 60% Rural 42 60% 40% 45 Poorest 20% 45 40% 42 43 41 Second 20% 45 Middle 20% 41 20% 20% 26 Fourth 20% 39 24 22 24 Richest 20% 30 0% 0% 1994–1995 2000 2006 2010 0% 20% 40% 60% 80% 100% 1994–1995 2000 2006 2010 DHS MICS MICS MICS DHS MICS MICS MICS Source: MICS, 2010. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -
Association Between First Caesarean Delivery and Adverse Outcomes In
Hu et al. BMC Pregnancy and Childbirth (2018) 18:273 https://doi.org/10.1186/s12884-018-1895-x RESEARCHARTICLE Open Access Association between first caesarean delivery and adverse outcomes in subsequent pregnancy: a retrospective cohort study Hong-Tao Hu1†, Jing-Jing Xu1†, Jing Lin1, Cheng Li1, Yan-Ting Wu2, Jian-Zhong Sheng3, Xin-Mei Liu4,5* and He-Feng Huang2,4,5* Abstract Background: Few studies have explored the association between a previous caesarean section (CS) and adverse perinatal outcomes in a subsequent pregnancy, especially in women who underwent a non-indicated CS in their first delivery. We designed this study to compare the perinatal outcomes of a subsequent pregnancy in women who underwent spontaneous vaginal delivery (SVD) or CS in their first delivery. Methods: This retrospective cohort study included women who underwent singleton deliveries at the International Peace Maternity and Child Health Hospital from January 2013 to December 2016. Data on the perinatal outcomes of all the women were extracted from the medical records. Multivariate logistic regression was conducted to assessed the association between CS in the first delivery and adverse perinatal outcomes in the subsequent pregnancy. Results: CS delivery in the subsequent pregnancy was more likely for women who underwent CS in their first birth than for women with previous SVD (97.3% versus 13.2%). CS in the first birth was also associated with a significantly increased risk of adverse outcomes in the subsequent pregnancy, especially in women who underwent a non- indicated CS. Adverse perinatal outcomes included pregnancy-induced hypertension [adjusted odds ratio (OR), 95% confidence interval (CI): 2.20, 1.59–3.05], gestational diabetes mellitus (1.82, 1.57–2.11), gestational anaemia (1.27, 1. -
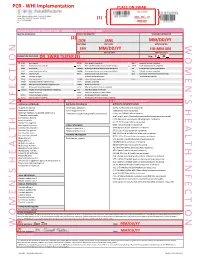
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

ABCDE Acronym Blood Transfusion 231 Major Trauma 234 Maternal
Cambridge University Press 978-0-521-26827-1 - Obstetric and Intrapartum Emergencies: A Practical Guide to Management Edwin Chandraharan and Sir Sabaratnam Arulkumaran Index More information Index ABCDE acronym albumin, blood plasma levels 7 arterial blood gas (ABG) 188 blood transfusion 231 allergic anaphylaxis 229 arterio-venous occlusions 166–167 major trauma 234 maternal collapse 12, 130–131 amiadarone, overdose 178 aspiration 10, 246 newborn infant 241 amniocentesis 234 aspirin 26, 180–181 resuscitation 127–131 amniotic fluid embolism 48–51 assisted reproduction 93 abdomen caesarean section 257 asthma 4, 150, 151, 152, 185 examination after trauma 234 massive haemorrhage 33 pain in pregnancy 154–160, 161 maternal collapse 10, 13, 128 atracurium, drug reactions 231 accreta, placenta 250, 252, 255 anaemia, physiological 1, 7 atrial fibrillation 205 ACE inhibitors, overdose 178 anaerobic metabolism 242 automated external defibrillator (AED) 12 acid–base analysis 104 anaesthesia. See general anaesthesia awareness under anaesthesia 215, 217 acidosis 94, 180–181, 186, 242 anal incontinence 138–139 ACTH levels 210 analgesia 11, 100, 218 barbiturates, overdose 178 activated charcoal 177, 180–181 anaphylaxis 11, 227–228, 229–231 behaviour/beliefs, psychiatric activated partial thromboplastin time antacid prophylaxis 217 emergencies 172 (APTT) 19, 21 antenatal screening, DVT 16 benign intracranial hypertension 166 activated protein C 46 antepartum haemorrhage 33, 93–94. benzodiazepines, overdose 178 Addison’s disease 208–209 See also massive -

Ask the Experts Amniotic Fluid Embolism Steven L. Clark, MD
Ask the Experts Questions have been written by: Amniotic Fluid Embolism Angela K. Hardyk, MD Mount Nittany Physician Group Ob/Gyn Steven L. Clark, MD State College, PA (Obstet Gynecol 2014;123:337–48) Responses have been written by: Steven L. Clark, MD Hospital Corporation of America Nashville, TN Question 1: How would you counsel a patient about a future pregnancy if she has been lucky enough to survive an amniotic fl uid embolism (AFE)? Would there be any special precautions she would need to take for her next pregnancy? Response from Dr. Clark: The available data in this area consist only of several very small series and case reports. These data suggest that the risks of recurrence are low. In addition, a pathophysiologic mechanism of disease that hinges on a maternal reaction to a specif- ic set of fetal antigens would suggest that recurrence ought to be uncommon. On the other hand, having dodged one bullet, is it really wise to spin the wheel again? My counseling goes something like this: “Available data suggest that the risk of recurrence is low, and there are a number of reports of successful pregnancy outcome after AFE survival. However, given the potential severity of AFE if it does recur, and a lack of really good data regarding risks, I advise you to undertake another pregnancy only if you are willing to accept a small risk of catastrophic outcome including death.” If a patient chooses to undertake pregnancy, I do not alter my management in any way, other than delivery in a tertiary center. -

Maternal Mortality in the United States, 1935 to 2007
Maternal Mortality in the United States, 1935-2007: Substantial Racial/Ethnic, Socioeconomic, and Geographic Disparities Persist Gopal K. Singh, PhD U.S. Department of Health and Human Services Health Resources and Services Administration Maternal and Child Health Bureau Figure 1: Maternal Mortality by Race, United States, Figure 2: Maternal Mortality Rate by Race/Ethnicity, 1935–2007 United States, 2005-2007 Trends in Maternal Mortality by Race Maternal mortality in the United States has declined Maternal deaths are those related to or aggravated by dramatically over the past century (1-4). The rate declined pregnancy or pregnancy management and which occur from 607.9 maternal deaths per 100,000 live births in 1915 during or within 42 days after the end of pregnancy (3). to 12.7 in 2007 (1-3). However, maternal mortality in the Although mortality trend data extend farther back in time United States has changed very little in the past 25 years for the entire United States and the birth registration area (1, 3). Achieving further reductions in the maternal mortality (1, 2), we chose 1935 as the start of the time trend analysis rate is an important public health priority for the nation as since it coincided with the inception of Title V of the Social the rates for certain ethnic minority and socioeconomic Security Act, a national public health legislation aimed at groups remain relatively high (3, 4, 5). A cross-national promoting and improving the health and welfare services comparison of the 2005 statistics by the World Health for all mothers and children. The maternal mortality rates in Organization (WHO) reveals that the U.S. -

Managing the Risk of Uterine Rupture During a Trial of Labor After Cesarean Section
Managing the Risk of Uterine Rupture During a Trial of Labor After Cesarean Section By NORCAL Mutual Insurance Company Introduction While a successful vaginal birth after cesarean section (VBAC) is associated with less morbidity and mortality than repeat cesarean section (C-section), an unsuccessful VBAC is associated with a small but significant risk of uterine rupture that can result in death or serious injury to both the mother and the infant.1 When a trial of labor after C-section (TOLAC) ends in uterine rupture, emergency C-section, and the delivery of an infant with brain injuries, there is a good chance that the child’s This article originally appeared in the parents will file a lawsuit, or at least September 2011 issue of Claims Rx. It consider it. It should be noted that has been edited by Drs. Mark Zakowski, a plaintiff’s attorney is supposed to Patricia Dailey and Stephen Jackson prove duty (responsibility of the to meet the educational needs of physicians involved), negligence anesthesiologists, and is reprinted, as (care provided was below the changed, with permission. ©Copyright standard of care) and causation 2011, NORCAL Mutual Insurance Co. (negligence led to the injury) All Rights Reserved. Reproduction as well as injury. However, the permissible with written permission plaintiffs probably won’t focus on and credit. whether the standard of care was met, and their attorney might not either. In these types of cases, the degree of the infant’s brain injuries tends to over- shadow other liability issues. This can carry through to trial because juries are generally biased toward severely brain-injured infants and the parents who must provide for them. -

Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia
Open Access Original Article DOI: 10.7759/cureus.17218 Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia Deena Dahshan 1 , Mohamed Suliman 2 , Ebad U. Rahman 3 , Zachary Curtis 1 , Ellen Thompson 2 1. Internal Medicine, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 2. Cardiology, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 3. Internal Medicine, St. Mary's Medical Center, Huntington, USA Corresponding author: Deena Dahshan, [email protected] Abstract Introduction Due to high levels of intravenous drug use (IVDU) in West Virginia (WV), there are increasing numbers of hospitalizations for infective endocarditis (IE). More specifically, pregnant patients with IE are a uniquely challenging population, with complex management and a clinical course that further affects the health of the fetus, with high morbidity and mortality. Timely recognition and awareness of the most common bacterial causes will provide hospitals and clinicians with valuable information to manage future patients. Methods This retrospective study analyzed the clinical course of pregnant patients admitted with IE and IVDU history presenting at Cabell Huntington Hospital from 2013 to 2018. Inclusion criteria were women between 16 and 45 years of age confirmed to be pregnant by urine pregnancy test and ultrasonography with at least eight weeks gestation, with a first-time diagnosis of endocarditis and an identified history of IVDU. We excluded charts with pre-existing risk factors including a history of valvular disease, rheumatic heart disease, surgical valve repair or mechanical valve replacement, or a diagnosis of coagulopathies. The resulting charts were evaluated for isolated organisms, reported clinical course, and complications of the pregnancy. -

Managing Complications in Pregnancy and Childbirth Fetal
IMPAC FEtal distress in labour WHO Home | Reproductive Health Home | HRP | What's new | Resources | Contact | Search Department of Reproductive Health and Research (RHR), World Health Organization z Abbreviations Managing Complications in Pregnancy and Childbirth z Index A guide for midwives and doctors z List of diagnoses z MCPC Home Section 2 - Symptoms Clinical principles Rapid initial assessment Fetal distress in labour Talking with women and their families Emotional and psychological support PROBLEMS Emergencies z Abnormal fetal heart rate (less than 100 or more than 180 beats per minute). General care principles Clinical use of blood, blood products and z Thick meconium-stained amniotic fluid. replacement fluids Antibiotic therapy Anaesthesia and analgesia GENERAL MANAGEMENT Operative care principles z Prop up the woman or place her on her left side. Normal Labour and childbirth Newborn care principles z Stop oxytocin if it is being administered. Provider and community linkages ABNORMAL FETAL HEART RATE Symptoms BOX S-7 Abnormal fetal heart rate Shock Vaginal bleeding in early pregnancy z A normal fetal heart rate may slow during a contraction but usually recovers to normal as Vaginal bleeding in later pregnancy and soon as the uterus relaxes. labour z A very slow fetal heart rate in the absence of contractions or persisting after contractions is Vaginal bleeding after childbirth suggestive of fetal distress. Headache, blurred vision, convulsions or loss of consciousness, elevated blood z A rapid fetal heart rate may be a response to maternal fever, drugs causing rapid maternal pressure heart rate (e.g. tocolytic drugs), hypertension or amnionitis. In the absence of a rapid maternal Unsatisfactory progress of Labour heart rate, a rapid fetal heart rate should be considered a sign of fetal distress. -
Low-Lying Placenta
LOW- LYING PLACENTA LOW-LYING PLACENTA WHAT IS PLACENTA PRAEVIA? The placenta develops along with the baby in the uterus (womb) during pregnancy. It connects the baby with the mother’s blood system and provides the baby with its source of oxygen and nourishment. The placenta is delivered after the baby and is also called the afterbirth. In some women the placenta attaches low in the uterus and may be near, or cover a part, or lie over the cervix (entrance to the womb). If it is shown in early ultrasound scans, it is called a low-lying placenta. In most cases, the placenta moves upwards as the uterus enlarges. For some women the placenta continues to lie in the lower part of the uterus in the last months of pregnancy. This condition is known as placenta praevia. If the placenta covers the cervix, this is known as major placenta praevia. Normal Placenta Placenta Praevia Major Placenta Praevia WHAT ARE THE RISKS TO MY BABY AND ME? When the placenta is in the lower part of the womb, there is a risk that you may bleed in the second half of pregnancy. Bleeding from placenta praevia can be heavy, and so put the life of the mother and baby at risk. However, deaths from placenta praevia are rare. You are more likely to need a caesarean section because the placenta is in the way of your baby being born. HOW IS PLACENTA PRAEVIA DIAGNOSED? A low-lying placenta may be suspected during the routine 20-week ultrasound scan. Most women who have a low-lying placenta at the routine 20-week scan will not go on to have a low-lying placenta later in the pregnancy – only 1 in 10 go on to have a placenta praevia.