Pelvic Pain Cause, Effect and Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Basic Biomechanics
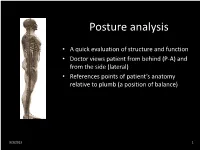
Posture analysis • A quick evaluation of structure and function • Doctor views patient from behind (P-A) and from the side (lateral) • References points of patient’s anatomy relative to plumb (a position of balance) 9/3/2013 1 Posture analysis • Lateral View – Knees (anterior, posterior, plumb, genu recurvatum) – Trochanter (anterior, posterior, plumb) – Pelvis (anterior, posterior, neutral pelvic tilt) – Lumbar lordosis (hypo-, hyper-, normal) – Mid-axillary line (anterior, posterior, plumb) – Thoracic kyphosis (hyp-, hyper- normal) – Acromion (anterior, posterior, plumb) – Scapulae (protracted, retracted, normal) – Cervical lordosis (hypo-, hyper-, normal) – External auditory meatus (anterior, posterior, plumb) – Occiput (extended, neutral, flexed) 9/3/2013 2 Posture analysis • Posterior – Anterior View – Feet (pronation, supination, normal) – Achilles tendon (bowed in/out, normal) – Knees (genu valga/vera, normal - internal/external rotation) – Popliteal crease heights (low, high, level) – Trochanter heights (low, high, level) – Iliac crest heights (low on the right/left, normal) – Lumbar scoliosis (right/left, or no signs of) – Thoracic scoliosis (right/left, or no signs of) – Shoulder level (low on the right/left, or normal) – Cervical scoliosis (right/left, or no signs of) – Cervical position (rotation, tilt, neutral) – Mastoid (low on the right/left, or normal) 9/3/2013 3 …..poor postures 9/3/2013 4 Functional Anatomy of the Spine • The vertebral curvatures – Cervical Curve • Anterior convex curve (lordosis) develop in infancy -

Applied Anatomy of the Hip RICARDO A
Applied Anatomy of the Hip RICARDO A. FERNANDEZ, MHS, PT, OCS, CSCS • Northwestern University The hip joint is more than just a ball-and- bones fuse in adults to form the easily recog- socket joint. It supports the weight of the nized “hip” bone. The pelvis, meaning bowl head, arms, and trunk, and it is the primary in Latin, is composed of three structures: the joint that distributes the forces between the innominates, the sacrum, and the coccyx pelvis and lower extremities.1 This joint is (Figure 1). formed from the articu- The ilium has a large flare, or iliac crest, Key PointsPoints lation of the proximal superiorly, with the easily palpable anterior femur with the innomi- superior iliac spine (ASIS) anterior with the The hip joint is structurally composed of nate at the acetabulum. anterior inferior iliac spine (AIIS) just inferior strong ligamentous and capsular compo- The joint is considered to it. Posteriorly, the crest of the ilium ends nents. important because it to form the posterior superior iliac spine can affect the spine and (PSIS). With respect to surface anatomy, Postural alignment of the bones and joints pelvis proximally and the PSIS is often marked as a dimple in the of the hip plays a role in determining the femur and patella skin. Clinicians attempting to identify pelvic functional gait patterns and forces associ- distally. The biomechan- or hip subluxations, leg-length discrepancies, ated with various supporting structures. ics of this joint are often or postural faults during examinations use There is a relationship between the hip misunderstood, and the these landmarks. -

How to Perform a Transrectal Ultrasound Examination of the Lumbosacral and Sacroiliac Joints
DIAGNOSTIC IMAGING How to Perform a Transrectal Ultrasound Examination of the Lumbosacral and Sacroiliac Joints Erik H.J. Bergman, DVM, Diplomate ECAR, Associate Member LA-ECVDI*; Sarah M. Puchalski, DVM, Diplomate ACVR; and Jean-Marie Denoix, DVM, PhD, Agre´ge´, Associate Member LA-ECVDI Authors’ addresses: Lingehoeve Veldstraat 3 Lienden 4033 AK, The Netherlands (Bergman); Uni- versity of California, Davis, One Shields Avenue, School of Veterinary Medicine, Davis, CA 95616 (Puchalski); E´ cole Nationale Ve´te´rinaire d’Alfort, 7 Avenue du Ge´ne´ral de Gaulle, 94700 Maisons- Alfort, France (Denoix); e-mail: [email protected]. *Corresponding and presenting author. © 2013 AAEP. 1. Introduction have allowed for identification of these structures 5 There is increasing interest in pathology of the and the inter-transverse joints. These authors urge lumbosacral and sacroiliac joints giving rise to stiff- caution in the interpretation of lesions identified on ness and/or lameness and decreased performance radiography in the absence of other diagnostic im- in equine sports medicine.1–3 Pain arising from aging and clinical examination. Nuclear scintigra- these regions can be problematic alone or in con- phy is an important component of work-up for junction with lameness arising from other sites sacroiliac region pain, but limitations exist. Sev- 9,10 (thoracolumbar spine, hind limbs, or forelimbs).4 eral reports exist detailing the anatomy and tech- Localization of pain to this region is critically impor- nique findings in normal horses11,12 and findings in tant through clinical assessment, diagnostic anes- lame horses.13 Patient motion, camera positioning, thesia, and imaging. and muscle asymmetry can cause errors in interpre- In general, diagnostic imaging of the axial skele- tation. -

Trans-Obturator Cable Fixation of Open Book Pelvic Injuries
www.nature.com/scientificreports OPEN Trans‑obturator cable fxation of open book pelvic injuries Martin C. Jordan 1*, Veronika Jäckle1, Sebastian Scheidt2, Fabian Gilbert3, Stefanie Hölscher‑Doht1, Süleyman Ergün4, Rainer H. Mefert1 & Timo M. Heintel1 Operative treatment of ruptured pubic symphysis by plating is often accompanied by complications. Trans‑obturator cable fxation might be a more reliable technique; however, have not yet been tested for stabilization of ruptured pubic symphysis. This study compares symphyseal trans‑obturator cable fxation versus plating through biomechanical testing and evaluates safety in a cadaver experiment. APC type II injuries were generated in synthetic pelvic models and subsequently separated into three diferent groups. The anterior pelvic ring was fxed using a four‑hole steel plate in Group A, a stainless steel cable in Group B, and a titan band in Group C. Biomechanical testing was conducted by a single‑ leg‑stance model using a material testing machine under physiological load levels. A cadaver study was carried out to analyze the trans‑obturator surgical approach. Peak‑to‑peak displacement, total displacement, plastic deformation and stifness revealed a tendency for higher stability for trans‑ obturator cable/band fxation but no statistical diference to plating was detected. The cadaver study revealed a safe zone for cable passage with sufcient distance to the obturator canal. Trans‑ obturator cable fxation has the potential to become an alternative for symphyseal fxation with less complications. Disruption of the pubic symphysis is commonly seen in pelvic ring injuries of trauma patients 1,2. Te disrup- tion of the anterior pelvic ring might occur in combination with a posterior pelvic ring impairment of variable severity. -

Epithelia Joitns
NAME LOCATION STRUCTURE FUNCTION MOVEMENT Temporomandibular joint Condylar head of ramus of Synovial Diarthrosis Modified hinge joint mandible and glenoid fossa of Rotation and gliding temporal bone Biaxial Zygapophyseal joint Between articular processes of Synovial Diarthrosis Gliding 2 adjacent vertebrae Non axial Atlanto-Occipital joints Atlas and occipital condyle of Synovial Diarthrosis Ellipsoid occipital bone Biaxial Atlantoaxial joints Atlas and axis Synovial Diarthrosis Pivot Uniaxial Joints of vertebral arches Ligaments Fibrous Amphiarthrosis Syndesmoses Intervertebral symphyseal Intervertebral disk between 2 Cartilaginous Amphiarthrosis joints vertebrae Symphysis Costovertebral Head of ribs and body of Synovial Diarthrosis Gliding thoracic vertebra Non axial Costotrasnverse joints Tubercle of rib and transverse Synovial Diarthrosis Gliding process of thoracic vertebra Non axial Lumbosacral Joint Left and right zygopophyseal Laterally Synovial joint Intervertebral symphyseal joint Symphysis SternoclavicularJoint Clavicular notch articulates Synovial Diarthrosis Gliding with medial ends of clavicle Non Axial Manubriosternal Joint Hyaline cartilage junction Cartilaginous Synarthrosis Sternal Angle between manubrium and body Symphysis Xiphisternal Joint Cartilage between xiphoid Synchondrosis Synarthrosis process and body Synostoses Sternocostal Joint (1st) Costocartilage 1 with sternum Cartilaginous Synchondrosis Synarthrosis NAME Location Section Anterior longitudinal runs down anterior surface of vertebral body Vertebral column ligament Posterior longitudinal in canal, runs down posterior surface of vertebral body ligament Interspinous ligament Connects spinous processes Ligamentum flavum Connects laminae ! Intra-articular Disc Between articulating surface of sternum and clavicle Sternoclavicular Joint Costoclavicular ligament 1st rib to clavicle !. -

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -

The Structure and Movement of Clarinet Playing D.M.A
The Structure and Movement of Clarinet Playing D.M.A. DOCUMENT Presented in Partial Fulfilment of the Requirements for the Degree Doctor of Musical Arts in the Graduate School of The Ohio State University By Sheri Lynn Rolf, M.D. Graduate Program in Music The Ohio State University 2018 D.M.A. Document Committee: Dr. Caroline A. Hartig, Chair Dr. David Hedgecoth Professor Katherine Borst Jones Dr. Scott McCoy Copyrighted by Sheri Lynn Rolf, M.D. 2018 Abstract The clarinet is a complex instrument that blends wood, metal, and air to create some of the world’s most beautiful sounds. Its most intricate component, however, is the human who is playing it. While the clarinet has 24 tone holes and 17 or 18 keys, the human body has 205 bones, around 700 muscles, and nearly 45 miles of nerves. A seemingly endless number of exercises and etudes are available to improve technique, but almost no one comments on how to best use the body in order to utilize these studies to maximum effect while preventing injury. The purpose of this study is to elucidate the interactions of the clarinet with the body of the person playing it. Emphasis will be placed upon the musculoskeletal system, recognizing that playing the clarinet is an activity that ultimately involves the entire body. Aspects of the skeletal system as they relate to playing the clarinet will be described, beginning with the axial skeleton. The extremities and their musculoskeletal relationships to the clarinet will then be discussed. The muscles responsible for the fine coordinated movements required for successful performance on the clarinet will be described. -

The Anatomy and Function of the Equine Thoracolumbar Longissimus Dorsi Muscle
Aus dem Veterinärwissenschaftlichen Department der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Lehrstuhl für Anatomie, Histologie und Embryologie Vorstand: Prof. Dr. Dr. Fred Sinowatz Arbeit angefertigt unter der Leitung von Dr. Renate Weller, PhD, MRCVS The Anatomy and Function of the equine thoracolumbar Longissimus dorsi muscle Inaugural-Dissertation zur Erlangung der tiermedizinischen Doktorwürde der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Vorgelegt von Christina Carla Annette von Scheven aus Düsseldorf München 2010 2 Gedruckt mit der Genehmigung der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Dekan: Univ.-Prof. Dr. Joachim Braun Berichterstatter: Priv.-Doz. Dr. Johann Maierl Korreferentin: Priv.-Doz. Dr. Bettina Wollanke Tag der Promotion: 24. Juli 2010 3 Für meine Familie 4 Table of Contents I. Introduction................................................................................................................ 8 II. Literature review...................................................................................................... 10 II.1 Macroscopic anatomy ............................................................................................. 10 II.1.1 Comparative evolution of the body axis ............................................................ 10 II.1.2 Axis of the equine body ..................................................................................... 12 II.1.2.1 Vertebral column of the horse.................................................................... -

A Biomechanical Model of the Lumbosacral Joint During Lifting Activities
A BIOMECHANICAL MODEL OF THE LUMBOSACRAL JOINT DURING LIFTING ACTIVITIES CHARLES K. ANDERSON,* DON B. CHAFF1N.t GARY D. HERRINt and LARRY S. MATTHEWS% *Back Systems, Inc., 5495 Beltline Road, Suite 390, Dallas, TX 75240. U.S.A.; t Center for Ergonomics. Department of Industrial and Operations Engineering, The University of Michigan, Ann Arbor, MI 48109, U.S.A.; SC4002 Outpatient Building, Box 054. University Hospital, The University of Michigan, Ann Arbor, MI 48109. U.S.A. Abstract-A biomechanical model of the lumbosacral region was constructed for the purpose of systematically studying the combined stresses and strains on the local ligaments, muscles and disc tissue during sagittal plane two-handed lifting. The model was validated in two ways. The first validation was a comparison ofexperimental study results with model predictions. In general predictions compared very reasonably with observed values of several authors with the exception of strain predictions on the articular ligaments. Second, a sensitivity analysis was performed over a wide range of lifting tasks. The predicted stress/strain values followed anticipated patterns and were of reasonable magnitudes. On the basis of the results of the sensitivity analysis it was concluded that typical lifting tasks can lead to excessive disc compressive forces, muscle moment generation requirements, and possibly lumbodorsal fascia strains. Conversely, annulus rupture of a healthy disc due to overstrain appears very unlikely. INTRODUCLION sacral endplate and strain in the posterior aspect of the outermost layer of the annulus. These tissue load The prevalence and cost of industrially-related low parameters were selected on the basis of their purpor- back pain underscores the need for a better under- ted role in the genesis of low-back pain. -

The Female Pelvic Floor Fascia Anatomy: a Systematic Search and Review
life Systematic Review The Female Pelvic Floor Fascia Anatomy: A Systematic Search and Review Mélanie Roch 1 , Nathaly Gaudreault 1, Marie-Pierre Cyr 1, Gabriel Venne 2, Nathalie J. Bureau 3 and Mélanie Morin 1,* 1 Research Center of the Centre Hospitalier Universitaire de Sherbrooke, Faculty of Medicine and Health Sciences, School of Rehabilitation, Université de Sherbrooke, Sherbrooke, QC J1H 5N4, Canada; [email protected] (M.R.); [email protected] (N.G.); [email protected] (M.-P.C.) 2 Anatomy and Cell Biology, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC H3A 0C7, Canada; [email protected] 3 Centre Hospitalier de l’Université de Montréal, Department of Radiology, Radio-Oncology, Nuclear Medicine, Faculty of Medicine, Université de Montréal, Montreal, QC H3T 1J4, Canada; [email protected] * Correspondence: [email protected] Abstract: The female pelvis is a complex anatomical region comprising the pelvic organs, muscles, neurovascular supplies, and fasciae. The anatomy of the pelvic floor and its fascial components are currently poorly described and misunderstood. This systematic search and review aimed to explore and summarize the current state of knowledge on the fascial anatomy of the pelvic floor in women. Methods: A systematic search was performed using Medline and Scopus databases. A synthesis of the findings with a critical appraisal was subsequently carried out. The risk of bias was assessed with the Anatomical Quality Assurance Tool. Results: A total of 39 articles, involving 1192 women, were included in the review. Although the perineal membrane, tendinous arch of pelvic fascia, pubourethral ligaments, rectovaginal fascia, and perineal body were the most frequently described structures, uncertainties were Citation: Roch, M.; Gaudreault, N.; identified in micro- and macro-anatomy. -

Lumbar Spinal Conditions
ANDERc11.qxd 11/16/07 3:53 PM Page 306 CHAPTER 11 Lumbar Spinal Conditions STUDENT OUTCOMES 1. Locate and explain the functional significance of the bony and soft-tissue structures of the lumbar spine. 2. Describe the motion capabilities of the lumbar spine. 3. Identify the factors that contribute to mechanical loading on the spine. 4. Describe specific strategies in activities of daily living to reduce spinal stress in the lumbar region. 5. Identify anatomical variations that can predispose individuals to lumbar spine injuries. 6. Explain the measures used to prevent injury to the lumbar spinal region. 7. Describe the common injuries and conditions of the lumbar spine and low back area in physically active individuals. 8. Describe a thorough assessment of the lumbar spine. 9. Identify rehabilitative exercises for the lumbar region. 306 ANDERc11.qxd 11/16/07 3:53 PM Page 307 CHAPTER 11 Lumbar Spinal Conditions 307 ROLE DELINEATION COMPETENCIES The following Performance Domains and Tasks defined in the National Athletic Trainers’ Associa- tion Board of Certification Role Delineation Study, 5th Edition are addressed in this chapter: BOC COMPETENCIES II. Clinical Evaluation and Diagnosis A. Obtain a history through observation, interview, and/or review of relevant records to assess current or potential injury, illness, or condition. B. Inspect the involved area(s) visually to assess the injury, illness, or health-related condition. C. Palpate the involved area(s) using standard techniques to assess the injury, illness, or health-related condition. D. Perform specific tests in accordance with accepted procedures to assess the injury, illness, or health- related condition. -
Student Workbook Answer Pages Italicized Page Numbers After the Answers Indicate Where the Informa- Matching 5) Deep Fascia Tion Can Be Found in Trail Guide
Student Workbook Answer Pages Italicized page numbers after the answers indicate where the informa- Matching 5) deep fascia tion can be found in Trail Guide. 1) N adipose—p. 17 6) adipose (fatty) tissue 2) F aponeurosis—p. 13 7) superficial fascia 3) D artery—p. 16 8) skin 4) H bone—p. 10 9) deep fascia Introduction 5) E bursa—p. 16 Tour Guide Tips #1, p. 1 6) B fascia—p. 14 1) bony landmarks—p. 2 7) G ligament—p. 13 2) Even though the topography, 8) I lymph node—p. 17 Navigating shape and proportion are unique, 9) A muscle—p. 11 Regions of the Body, p. 6 the body’s composition and struc- 10) J nerve—p. 17 1) pectoral tures are virtually identical on all 11) K retinaculum—p. 15 2) axillary individuals.—p. 2 12) L skin—p. 10 3) brachial 3) To examine or explore by touch- 13) M tendon—p. 13 4) cubital ing (an organ or area of the body), 14) C vein—p. 16 5) abdominal usually as a diagnostic aid—p. 4 6) inguinal 4) locating, aware, assessing—p. 4 Exploring Textures #1, p. 3 7) pubic 5) directs movement, depth.—p. 4 1) epidermis 8) femoral 6) • read the information 2) dermis 9) facial • visualize what you are trying 3) arrector pili muscle 10) mandibular to access 4) sweat gland 11) supraclavicular • verbalize to your partner what 5) hair follicle 12) antecubital you feel 6) blood vessels 13) patellar • locate the structure first 7) muscle fibers 14) crural on yourself 8) endomysium 15) cranial • read the text aloud 9) perimysium 16) cervical • be patient—p.