Lumbar Spinal Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Basic Biomechanics
Posture analysis • A quick evaluation of structure and function • Doctor views patient from behind (P-A) and from the side (lateral) • References points of patient’s anatomy relative to plumb (a position of balance) 9/3/2013 1 Posture analysis • Lateral View – Knees (anterior, posterior, plumb, genu recurvatum) – Trochanter (anterior, posterior, plumb) – Pelvis (anterior, posterior, neutral pelvic tilt) – Lumbar lordosis (hypo-, hyper-, normal) – Mid-axillary line (anterior, posterior, plumb) – Thoracic kyphosis (hyp-, hyper- normal) – Acromion (anterior, posterior, plumb) – Scapulae (protracted, retracted, normal) – Cervical lordosis (hypo-, hyper-, normal) – External auditory meatus (anterior, posterior, plumb) – Occiput (extended, neutral, flexed) 9/3/2013 2 Posture analysis • Posterior – Anterior View – Feet (pronation, supination, normal) – Achilles tendon (bowed in/out, normal) – Knees (genu valga/vera, normal - internal/external rotation) – Popliteal crease heights (low, high, level) – Trochanter heights (low, high, level) – Iliac crest heights (low on the right/left, normal) – Lumbar scoliosis (right/left, or no signs of) – Thoracic scoliosis (right/left, or no signs of) – Shoulder level (low on the right/left, or normal) – Cervical scoliosis (right/left, or no signs of) – Cervical position (rotation, tilt, neutral) – Mastoid (low on the right/left, or normal) 9/3/2013 3 …..poor postures 9/3/2013 4 Functional Anatomy of the Spine • The vertebral curvatures – Cervical Curve • Anterior convex curve (lordosis) develop in infancy -

Low Back Pain in Adolescent Athletes
Low back pain in Adolescent Athletes Claes Göran Sundell Department of Community Medicine and Rehabilitation Umeå 2019 Responsible publischer under Swedish law: The Dean of the Medical Faculty This work is protected by the Swedish Copyright Legislation (Act 1960:729) Dissertation for PhD ISBN: 978-91-7855-024-1 ISSN-0346-6612 New series no: 2014 Copyright © Claes Göran Sundell, 2019 Cover illustration: Stina Norgren, Illustre.se Illustrations: Stina Norgren, Illustre.se, page 1,3,4,12,13,41 Illustration page 2: Permission Encyplopedica Brittanica, page 2 Pictures: 3D4 Medical; www.3D4Medical.com, page 1,3,5,6,7 Article nr .3 "© Georg Thieme Verlag KG." All previously published papers were reproduced with the kind permission of the publishers Electronic version available at: http://umu.diva-portal.org/ Printed by: UmU Print Service, Umeå University Umeå, Sweden, 2019 1 “Listen to the Sound of Silence” Unknown To my family: Doris, Cecilia, David, Johan Contents Abstract .......................................................................................... iv Sammanfattning på svenska ........................................................... vi Preface .......................................................................................... viii Abbreviations ................................................................................. ix Introduction .................................................................................... 1 1.Anatomy ........................................................................................................................ -

Knee Osteoarthritis
BRIGHAM AND WOMEN’S HOSPITAL Department of Rehabilitation Services Standard of Care: _Osteoarthritis of the Knee Case Type / Diagnosis: Knee Osteoarthritis. ICD-9: 715.16, 719.46 Osteoarthritis/Osteoarthrosis (OA) is the most common joint disease causing disability, affecting more than 7 million people in the United States 1. OA is a disease process of axial and peripheral joints. It is characterized by progressive deterioration and loss of articular cartilage and by reactive bone changes at the margins of the joints and in the subchondral bone. Clinical manifestations are characterized by slowly developing joint pain, stiffness, and joint enlargement with limitations of motion. Knee osteoarthritis (OA) results from mechanical and idiopathic factors that alter the balance between degradation and synthesis of articular cartilage and subchondral bone. The etiology of knee OA is not entirely clear, yet its incidence increases with age and in women. 1 The etiology may have genetic factors affecting collagen, or traumatic factors, such as fracture or previous meniscal damage. Obesity is a risk factor for the development and progression of OA. Early degenerative changes predict progression of the disease. Underlying biomechanical factors, such as varum or valgum of the tibial femoral joint may predispose people to OA. However Hunter et al 2reported knee alignment did not predict OA, but rather was a marker of the disease severity. Loss of quadriceps muscle strength is associated with knee pain and disability in OA. Clinical criteria for the diagnosis of OA of the knee has been established by Altman3 Subjects with examination finding consistent with any of the three categories were considered to have Knee OA. -

Applied Anatomy of the Hip RICARDO A
Applied Anatomy of the Hip RICARDO A. FERNANDEZ, MHS, PT, OCS, CSCS • Northwestern University The hip joint is more than just a ball-and- bones fuse in adults to form the easily recog- socket joint. It supports the weight of the nized “hip” bone. The pelvis, meaning bowl head, arms, and trunk, and it is the primary in Latin, is composed of three structures: the joint that distributes the forces between the innominates, the sacrum, and the coccyx pelvis and lower extremities.1 This joint is (Figure 1). formed from the articu- The ilium has a large flare, or iliac crest, Key PointsPoints lation of the proximal superiorly, with the easily palpable anterior femur with the innomi- superior iliac spine (ASIS) anterior with the The hip joint is structurally composed of nate at the acetabulum. anterior inferior iliac spine (AIIS) just inferior strong ligamentous and capsular compo- The joint is considered to it. Posteriorly, the crest of the ilium ends nents. important because it to form the posterior superior iliac spine can affect the spine and (PSIS). With respect to surface anatomy, Postural alignment of the bones and joints pelvis proximally and the PSIS is often marked as a dimple in the of the hip plays a role in determining the femur and patella skin. Clinicians attempting to identify pelvic functional gait patterns and forces associ- distally. The biomechan- or hip subluxations, leg-length discrepancies, ated with various supporting structures. ics of this joint are often or postural faults during examinations use There is a relationship between the hip misunderstood, and the these landmarks. -

Pars Injection for Lumbar Spondylolysis
Pars Injection for Lumbar Spondylolysis Issue 4: March 2016 Review date: February 2019 Following your recent investigations and consultation with your spinal surgeon, a possible cause for your symptoms may have been found. Your X-rays and / or scans have revealed that you have a lumbar spondylolysis. This is a stress fracture of the narrow bridge of bone between the facet joints (pars interarticularis) at the back of the spine, commonly called a pars defect. There may be a hereditary aspect to spondylolysis, for example an individual may be born with thin vertebral bone and therefore be vulnerable to this condition; or certain sports, such as gymnastics, weight lifting and football can put a great deal of stress on the bones through constantly over-stretching the spine. Either cause can result in a stress fracture on one or both sides of the vertebra (bone of the spine). Many people are not aware of their stress fracture or experience any problems but symptoms can occasionally occur including lower back pain, pain in the thighs and buttocks, stiffness, muscle tightness and tenderness. vertebra facet joint pars interarticularis sacrum spondylolysis (pars defect) intervertebral disc If the stress fracture weakens the bone so much that it is unable to maintain its proper position, the vertebra can start to shift out of place. This condition is called spondylolisthesis. Page 3 There is a forward slippage of one lumbar vertebra on the vertebra below it. The degree of spondylolisthesis may vary from mild to severe but if too much slippage occurs, the nerve roots can be stretched where they branch out of the spinal canal. -

National Imaging Associates, Inc. Clinical Guidelines FACET JOINT
National Imaging Associates, Inc. Clinical guidelines Original Date: July 1, 2015 FACET JOINT INJECTIONS OR BLOCKS Page 1 of 4 “FOR FLORIDA BLUE MEMBERS ONLY” CPT Codes: Last Review Date: May 28, 2015 Cervical/Thoracic Region: 64490 (+ 64491, +64492) Lumbar/Sacral Region: 64493 (+64494, +64495) Medical Coverage Guideline Number: Last Revised Date: 02-61000-30 Responsible Department: Implementation Date: July 2015 Clinical Operations “FOR FLORIDA BLUE MEMBERS ONLY” INTRODUCTION Facet joints (also called zygapophysial joints or z-joints), are posterior to the vertebral bodies in the spinal column and connect the vertebral bodies to each other. They are located at the junction of the inferior articular process of a more cephalad vertebra, and the superior articular process of a more caudal vertebra. These joints provide stability and enable movement, allowing the spine to bend, twist, and extend in different directions. They also restrict hyperextension and hyperflexion. Facet joints are clinically important spinal pain generators in those with chronic spinal pain. Facet joints may refer pain to adjacent structures, making the underlying diagnosis difficult, as referred pain may assume a pseudoradicular pattern. Lumbar facet joints may refer pain to the back, buttocks, and lower extremities while cervical facet joints may refer pain to the head, neck and shoulders. Imaging findings are of little value in determining the source and location of ‘facet joint syndrome’, a term referring to back pain caused by pathology at the facet joints. Imaging studies may detect changes in facet joint architecture, but correlation between radiologic findings and symptoms is unreliable. Although clinical signs are also unsuitable for diagnosing facet joint-mediated pain, they may be of value in selecting candidates for controlled local anesthetic blocks of either the medial branches or the facet joint itself. -

The Erector Spinae Plane Block a Novel Analgesic Technique in Thoracic Neuropathic Pain
CHRONIC AND INTERVENTIONAL PAIN BRIEF TECHNICAL REPORT The Erector Spinae Plane Block A Novel Analgesic Technique in Thoracic Neuropathic Pain Mauricio Forero, MD, FIPP,*Sanjib D. Adhikary, MD,† Hector Lopez, MD,‡ Calvin Tsui, BMSc,§ and Ki Jinn Chin, MBBS (Hons), MMed, FRCPC|| Case 1 Abstract: Thoracic neuropathic pain is a debilitating condition that is often poorly responsive to oral and topical pharmacotherapy. The benefit A 67-year-old man, weight 116 kg and height 188 cm [body of interventional nerve block procedures is unclear due to a paucity of ev- mass index (BMI), 32.8 kg/m2] with a history of heavy smoking idence and the invasiveness of the described techniques. In this report, we and paroxysmal supraventricular tachycardia controlled on ateno- describe a novel interfascial plane block, the erector spinae plane (ESP) lol, was referred to the chronic pain clinic with a 4-month history block, and its successful application in 2 cases of severe neuropathic pain of severe left-sided chest pain. A magnetic resonance imaging (the first resulting from metastatic disease of the ribs, and the second from scan of his thorax at initial presentation had been reported as nor- malunion of multiple rib fractures). In both cases, the ESP block also pro- mal, and the working diagnosis at the time of referral was post- duced an extensive multidermatomal sensory block. Anatomical and radio- herpetic neuralgia. He reported constant burning and stabbing logical investigation in fresh cadavers indicates that its likely site of action neuropathic pain of 10/10 severity on the numerical rating score is at the dorsal and ventral rami of the thoracic spinal nerves. -

Knee Evaluation
Evaluation of Knee Injuries Dr. Alan A. Zakaria, D.O., M.S. 1080 Kirts Blvd., Suite 400 Troy, Mi., 48084 Team Physician United States Soccer Federation University of Michigan Men’s and Women’s Soccer Objective Identify main anatomic components of the knee Perform basic knee exam along with special tests Identify common knee injury patterns and their physical exam findings. Anatomy ➢ Bony Anatomy ➢ Ligaments ➢ Cartilage ➢ Musculature ➢ Other Soft Tissue Knee Anatomy Two functional joints – Femorotibial – Femoropatellar Femoral condyles – Flex/extend Knee Anatomy Patella – Sesamoid with two concave surfaces and vertical ridge – Increases efficiency of extension Knee Anatomy: Anterior Cruciate Ligament (ACL) Run inferior, anterior, and medially Arises from medial aspect lateral femoral condyle Insert lateral to medial tibial eminence Restrains anterior subluxation of tibia on femur Knee Anatomy: Posterior Cruciate Ligament (PCL) Arises from the posterior intercondylar area of the tibia Inserts at the medial condyle of the femur Restrains posterior subluxation of the tibia on the femur Knee Anatomy: Medial Collateral Ligament (MCL) Postero-superior medial femoral condyle to proximal end of tibia Maximum tension at full extension Restraint to valgus stress Knee Anatomy: Lateral Collateral Ligament (LCL) Posterosuperior lateral femoral condyle to lateral head of fibula Restraint to varus stress Knee Anatomy: Meniscus Load bearing, joint stability, shock absorption Peripheral third vascularized Knee Anatomy: Articular Cartilage Hyaline cartilage -

How to Perform a Transrectal Ultrasound Examination of the Lumbosacral and Sacroiliac Joints
DIAGNOSTIC IMAGING How to Perform a Transrectal Ultrasound Examination of the Lumbosacral and Sacroiliac Joints Erik H.J. Bergman, DVM, Diplomate ECAR, Associate Member LA-ECVDI*; Sarah M. Puchalski, DVM, Diplomate ACVR; and Jean-Marie Denoix, DVM, PhD, Agre´ge´, Associate Member LA-ECVDI Authors’ addresses: Lingehoeve Veldstraat 3 Lienden 4033 AK, The Netherlands (Bergman); Uni- versity of California, Davis, One Shields Avenue, School of Veterinary Medicine, Davis, CA 95616 (Puchalski); E´ cole Nationale Ve´te´rinaire d’Alfort, 7 Avenue du Ge´ne´ral de Gaulle, 94700 Maisons- Alfort, France (Denoix); e-mail: [email protected]. *Corresponding and presenting author. © 2013 AAEP. 1. Introduction have allowed for identification of these structures 5 There is increasing interest in pathology of the and the inter-transverse joints. These authors urge lumbosacral and sacroiliac joints giving rise to stiff- caution in the interpretation of lesions identified on ness and/or lameness and decreased performance radiography in the absence of other diagnostic im- in equine sports medicine.1–3 Pain arising from aging and clinical examination. Nuclear scintigra- these regions can be problematic alone or in con- phy is an important component of work-up for junction with lameness arising from other sites sacroiliac region pain, but limitations exist. Sev- 9,10 (thoracolumbar spine, hind limbs, or forelimbs).4 eral reports exist detailing the anatomy and tech- Localization of pain to this region is critically impor- nique findings in normal horses11,12 and findings in tant through clinical assessment, diagnostic anes- lame horses.13 Patient motion, camera positioning, thesia, and imaging. and muscle asymmetry can cause errors in interpre- In general, diagnostic imaging of the axial skele- tation. -

Pain Pattern Explanation Forms
Pain Pattern Explanation Forms 1. Cervical Facet Pain Pattern 2. Cervical Radicular/Dynatome Pain Pattern 3. Costotransverse Joint Pain Pattern 4. Fibromyalgia Points 5. Hip Joint Pain Pattern 6. Lumbar Dermatomes: Chemical Radiculitis 7. Lumbar Dermatomes: Disc Pathology 8. Lumbar Disc Pathology Healed 9. Lumbar Epidural Fibrosis 10. Lumbar Facet Pain Pattern 11. Lumbar Stenosis 12. Sacroiliac Joint Pain Pattern 13. Thoracic Facet Pain Pattern 14. Upper Cervical Joint Pain Pattern The OEA pain pattern handouts are PDF files that can be used for patient education and marketing. They help you explain your diagnosis with original illustrations that the patients can take home with them. There is limited text so you can tell your explanation of the treatment plan. The pain patterns can be printed in color or black and white. Once purchased, our business card will be replaced with yours to personalize each handout. Each illustration is based on the pain patterns that have been established in books or research articles when available. Normal anatomy and pathoanatomy illustrations are shown for the clinician to explain the diagnosis to the patient and how their treatment can influence the pain generator. These can also be utilized as marketing tools. The following pages are some guidelines that can be utilized to explain the handouts to patients. Cervical Facet Pain Pattern The cervical facet joints are the joints of the neck. Neurophysiologic studies have shown that cervical facet‐joint capsules are sources of neck pain.1 Dwyer et al.2 established pain patterns of the cervical facet joints. o Parasagittal cervical and cervicothoracic pain. -
Digital Motion X-Ray Cervical Spine
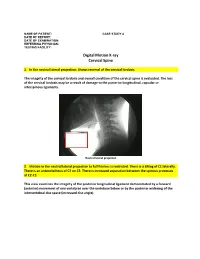
NAME OF PATIENT: CASE STUDY 4 DATE OF REPORT: DATE OF EXAMINATION: REFERRING PHYSICIAN: TESTING FACILITY: Digital Motion X-ray Cervical Spine 1. In the neutral lateral projection: Shows reversal of the cervical lordosis. The integrity of the cervical lordosis and overall condition of the cervical spine is evaluated. The loss of the cervical lordosis may be a result of damage to the posterior longitudinal, capsular or interspinous ligaments. Neutral lateral projection 2. Motion in the neutral lateral projection to full flexion: Is restricted. There is a tilting of C1 laterally. There is an anterolisthesis of C2 on C3. There is increased separation between the spinous processes at C2-C3. This view examines the integrity of the posterior longitudinal ligament demonstrated by a forward (anterior) movement of one vertebrae over the vertebrae below or by the posterior widening of the intervertebral disc space (increased disc angle). Widening of posterior disc space Anterolisthesis The integrity of the interspinous ligament is evaluated in the lateral flexion view. Damage to this ligament results in increased separation of the spinous processes in flexion. Damaged Interspinous Ligament Full flexion projection 3. Motion in the neutral lateral projection to full extension: Is restricted. There is a retrolisthesis of C4 on C5. This view examines the integrity of the anterior longitudinal ligament demonstrated by a backward (posterior) movement of one vertebrae over the vertebrae below or by the anterior widening of the intervertebral disc space (increased disc angle). Retrolisthesis Widening of the anterior disc Full Extension 4. Motion in the oblique flexion projection: Is restricted. There is gapping of the facet joints at C6-C7 bilaterally and C7-T1 bilaterally. -
Evicore Spine Imaging Guidelines
CLINICAL GUIDELINES Spine Imaging Policy Version 2.1 Effective October 1, 2020 eviCore healthcare Clinical Decision Support Tool Diagnostic Strategies:This tool addresses common symptoms and symptom complexes. Imaging requests for individuals with atypical symptoms or clinical presentations that are not specifically addressed will require physician review. Consultation with the referring physician, specialist and/or individual’s Primary Care Physician (PCP) may provide additional insight. CPT® (Current Procedural Terminology) is a registered trademark of the American Medical Association (AMA). CPT® five digit codes, nomenclature and other data are copyright 2020 American Medical Association. All Rights Reserved. No fee schedules, basic units, relative values or related listings are included in the CPT® book. AMA does not directly or indirectly practice medicine or dispense medical services. AMA assumes no liability for the data contained herein or not contained herein. © 2020 eviCore healthcare. All rights reserved. Spine Imaging Guidelines V2.1 Spine Imaging Guidelines Procedure Codes Associated with Spine Imaging 3 SP-1: General Guidelines 5 SP-2: Imaging Techniques 14 SP-3: Neck (Cervical Spine) Pain Without/With Neurological Features (Including Stenosis) and Trauma 22 SP-4: Upper Back (Thoracic Spine) Pain Without/With Neurological Features (Including Stenosis) and Trauma 26 SP-5: Low Back (Lumbar Spine) Pain/Coccydynia without Neurological Features 29 SP-6: Lower Extremity Pain with Neurological Features (Radiculopathy, Radiculitis, or Plexopathy and Neuropathy) With or Without Low Back (Lumbar Spine) Pain 33 SP-7: Myelopathy 37 SP-8: Lumbar Spine Spondylolysis/Spondylolisthesis 40 SP-9: Lumbar Spinal Stenosis 43 SP-10: Sacro-Iliac (SI) Joint Pain, Inflammatory Spondylitis/Sacroiliitis and Fibromyalgia 45 SP-11: Pathological Spinal Compression Fractures 48 SP-12: Spinal Pain in Cancer Patients 50 SP-13: Spinal Canal/Cord Disorders (e.g.