The Erector Spinae Plane Block a Novel Analgesic Technique in Thoracic Neuropathic Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Scapular Winging Is a Rare Disorder Often Caused by Neuromuscular Imbalance in the Scapulothoracic Stabilizer Muscles
SCAPULAR WINGING Scapular winging is a rare disorder often caused by neuromuscular imbalance in the scapulothoracic stabilizer muscles. Lesions of the long thoracic nerve and spinal accessory nerves are the most common cause. Patients report diffuse neck, shoulder girdle, and upper back pain, which may be debilitating, associated with abduction and overhead activities. Accurate diagnosis and detection depend on appreciation on comprehensive physical examination. Although most cases resolve nonsurgically, surgical treatment of scapular winging has been met with success. True incidence is largely unknown because of under diagnosis. Most commonly it is categorized anatomically as medial or lateral shift of the inferior angle of the scapula. Primary winging occurs when muscular weakness disrupts the normal balance of the scapulothoracic complex. Secondary winging occurs when pathology of the shoulder joint pathology. Delay in diagnosis may lead to traction brachial plexopathy, periscapular muscle spasm, frozen shoulder, subacromial impingement, and thoracic outlet syndrome. Anatomy and Biomechanics Scapula is rotated 30° anterior on the chest wall; 20° forward in the sagittal plane; the inferior angle is tilted 3° upward. It serves as the attachment site for 17 muscles. The trapezius muscle accomplishes elevation of the scapula in the cranio-caudal axis and upward rotation. The serratus anterior and pectoralis major and minor muscles produce anterior and lateral motion, described as scapular protraction. Normal Scapulothoracic abduction: As the limb is elevated, the effect is an upward and lateral rotation of the inferior pole of scapula. Periscapular weakness resulting from overuse may manifest as scapular dysfunction (ie, winging). Serratus Anterior Muscle Origin From the first 9 ribs Insert The medial border of the scapula. -

Thoracic Outlet and Pectoralis Minor Syndromes
S EMINARS IN V ASCULAR S URGERY 27 (2014) 86– 117 Available online at www.sciencedirect.com www.elsevier.com/locate/semvascsurg Thoracic outlet and pectoralis minor syndromes n Richard J. Sanders, MD , and Stephen J. Annest, MD Presbyterian/St. Luke's Medical Center, 1719 Gilpin, Denver, CO 80218 article info abstract Compression of the neurovascular bundle to the upper extremity can occur above or below the clavicle; thoracic outlet syndrome (TOS) is above the clavicle and pectoralis minor syndrome is below. More than 90% of cases involve the brachial plexus, 5% involve venous obstruction, and 1% are associate with arterial obstruction. The clinical presentation, including symptoms, physical examination, pathology, etiology, and treatment differences among neurogenic, venous, and arterial TOS syndromes. This review details the diagnostic testing required to differentiate among the associated conditions and recommends appropriate medical or surgical treatment for each compression syndrome. The long- term outcomes of patients with TOS and pectoralis minor syndrome also vary and depend on duration of symptoms before initiation of physical therapy and surgical intervention. Overall, it can be expected that 480% of patients with these compression syndromes can experience functional improvement of their upper extremity; higher for arterial and venous TOS than for neurogenic compression. & 2015 Published by Elsevier Inc. 1. Introduction compression giving rise to neurogenic TOS (NTOS) and/or neurogenic PMS (NPMS). Much less common is subclavian Compression of the neurovascular bundle of the upper and axillary vein obstruction giving rise to venous TOS (VTOS) extremity can occur above or below the clavicle. Above the or venous PMS (VPMS). -

National Imaging Associates, Inc. Clinical Guidelines FACET JOINT
National Imaging Associates, Inc. Clinical guidelines Original Date: July 1, 2015 FACET JOINT INJECTIONS OR BLOCKS Page 1 of 4 “FOR FLORIDA BLUE MEMBERS ONLY” CPT Codes: Last Review Date: May 28, 2015 Cervical/Thoracic Region: 64490 (+ 64491, +64492) Lumbar/Sacral Region: 64493 (+64494, +64495) Medical Coverage Guideline Number: Last Revised Date: 02-61000-30 Responsible Department: Implementation Date: July 2015 Clinical Operations “FOR FLORIDA BLUE MEMBERS ONLY” INTRODUCTION Facet joints (also called zygapophysial joints or z-joints), are posterior to the vertebral bodies in the spinal column and connect the vertebral bodies to each other. They are located at the junction of the inferior articular process of a more cephalad vertebra, and the superior articular process of a more caudal vertebra. These joints provide stability and enable movement, allowing the spine to bend, twist, and extend in different directions. They also restrict hyperextension and hyperflexion. Facet joints are clinically important spinal pain generators in those with chronic spinal pain. Facet joints may refer pain to adjacent structures, making the underlying diagnosis difficult, as referred pain may assume a pseudoradicular pattern. Lumbar facet joints may refer pain to the back, buttocks, and lower extremities while cervical facet joints may refer pain to the head, neck and shoulders. Imaging findings are of little value in determining the source and location of ‘facet joint syndrome’, a term referring to back pain caused by pathology at the facet joints. Imaging studies may detect changes in facet joint architecture, but correlation between radiologic findings and symptoms is unreliable. Although clinical signs are also unsuitable for diagnosing facet joint-mediated pain, they may be of value in selecting candidates for controlled local anesthetic blocks of either the medial branches or the facet joint itself. -

An Anatomical Illustrated Analysis of Yoga Postures Targeting the Back and Spine Through Cadaveric Study of Back Musculature Hana Fatima Panakkat1, Deborah Merrick*2
ISSN 2563-7142 ORIGINAL ARTICLE An Anatomical Illustrated Analysis of Yoga Postures Targeting the Back and Spine Through Cadaveric Study of Back Musculature Hana Fatima Panakkat1, Deborah Merrick*2 Panakkat HF, Merrick D. An Anatomical Illustrated present the findings, unique hand-drawn illustrations Analysis of Yoga Postures Targeting the Back and were used to depict the musculature found to be Spine Through Cadaveric Study of Back Musculature. highly active with each Yoga posture, with the erector Int J Cadaver Stud Ant Var. 2020;1(1):33-38. spinae muscles appearing prominent throughout. The combined approach of using hand-drawn illustrations Abstract with cadaveric dissection to present the anatomical Back pain is a debilitating lifestyle disease that affects analysis has allowed a seamless understanding of a large proportion of the world’s population at some complex anatomical concepts alongside the nuances point in their life. Absences from work due to this of intricate gross anatomy. This study highlights the have a huge economic impact on the patient, their importance of the inclusion of cadaveric dissection employer and the healthcare providers who seek to as a pedagogical tool in medical curriculum through support their recovery. Unfortunately, back pain is exploring the anatomical basis of Yoga, also allowing often resistant to treatment and intervention, therefore the possibility of using the workings of Yoga to aid alternative therapies such as Yoga are being explored. anatomical teaching. A greater understanding of this Within the literature, five Yoga postures were may help guide personalized Yoga regimes, which may identified to be associated with reduced back pain allow alternative therapies to become integrated into in patients suffering from Chronic lower back pain. -

Pain Pattern Explanation Forms
Pain Pattern Explanation Forms 1. Cervical Facet Pain Pattern 2. Cervical Radicular/Dynatome Pain Pattern 3. Costotransverse Joint Pain Pattern 4. Fibromyalgia Points 5. Hip Joint Pain Pattern 6. Lumbar Dermatomes: Chemical Radiculitis 7. Lumbar Dermatomes: Disc Pathology 8. Lumbar Disc Pathology Healed 9. Lumbar Epidural Fibrosis 10. Lumbar Facet Pain Pattern 11. Lumbar Stenosis 12. Sacroiliac Joint Pain Pattern 13. Thoracic Facet Pain Pattern 14. Upper Cervical Joint Pain Pattern The OEA pain pattern handouts are PDF files that can be used for patient education and marketing. They help you explain your diagnosis with original illustrations that the patients can take home with them. There is limited text so you can tell your explanation of the treatment plan. The pain patterns can be printed in color or black and white. Once purchased, our business card will be replaced with yours to personalize each handout. Each illustration is based on the pain patterns that have been established in books or research articles when available. Normal anatomy and pathoanatomy illustrations are shown for the clinician to explain the diagnosis to the patient and how their treatment can influence the pain generator. These can also be utilized as marketing tools. The following pages are some guidelines that can be utilized to explain the handouts to patients. Cervical Facet Pain Pattern The cervical facet joints are the joints of the neck. Neurophysiologic studies have shown that cervical facet‐joint capsules are sources of neck pain.1 Dwyer et al.2 established pain patterns of the cervical facet joints. o Parasagittal cervical and cervicothoracic pain. -
Digital Motion X-Ray Cervical Spine
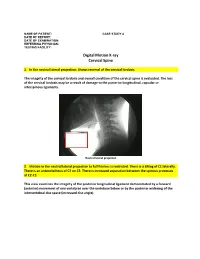
NAME OF PATIENT: CASE STUDY 4 DATE OF REPORT: DATE OF EXAMINATION: REFERRING PHYSICIAN: TESTING FACILITY: Digital Motion X-ray Cervical Spine 1. In the neutral lateral projection: Shows reversal of the cervical lordosis. The integrity of the cervical lordosis and overall condition of the cervical spine is evaluated. The loss of the cervical lordosis may be a result of damage to the posterior longitudinal, capsular or interspinous ligaments. Neutral lateral projection 2. Motion in the neutral lateral projection to full flexion: Is restricted. There is a tilting of C1 laterally. There is an anterolisthesis of C2 on C3. There is increased separation between the spinous processes at C2-C3. This view examines the integrity of the posterior longitudinal ligament demonstrated by a forward (anterior) movement of one vertebrae over the vertebrae below or by the posterior widening of the intervertebral disc space (increased disc angle). Widening of posterior disc space Anterolisthesis The integrity of the interspinous ligament is evaluated in the lateral flexion view. Damage to this ligament results in increased separation of the spinous processes in flexion. Damaged Interspinous Ligament Full flexion projection 3. Motion in the neutral lateral projection to full extension: Is restricted. There is a retrolisthesis of C4 on C5. This view examines the integrity of the anterior longitudinal ligament demonstrated by a backward (posterior) movement of one vertebrae over the vertebrae below or by the anterior widening of the intervertebral disc space (increased disc angle). Retrolisthesis Widening of the anterior disc Full Extension 4. Motion in the oblique flexion projection: Is restricted. There is gapping of the facet joints at C6-C7 bilaterally and C7-T1 bilaterally. -

Quantification of the Elastic Moduli of Lumbar Erector Spinae And
applied sciences Article Quantification of the Elastic Moduli of Lumbar Erector Spinae and Multifidus Muscles Using Shear-Wave Ultrasound Elastography Tae Hyun Lim 1, Deukhee Lee 2,3 , Olga Kim 1,3 and Song Joo Lee 1,3,* 1 Center for Bionics, Biomedical Research Institute, Korea Institute of Science and Technology, Seoul 02792, Korea; [email protected] (T.H.L.); [email protected] (O.K.) 2 Center for Healthcare Robotics, AI and Robot Institute, Korea Institute of Science and Technology, Seoul 02792, Korea; [email protected] 3 Division of Bio-Medical Science and Technology, KIST School, Korea University of Science and Technology, Seoul 02792, Korea * Correspondence: [email protected]; Tel.: +82-2-958-5645 Featured Application: The findings and approach can potentially be used to guide surgical train- ing and planning for developing a minimal-incision surgical procedure by considering surgical position-dependent muscle material properties. Abstract: Although spinal surgeries with minimal incisions and a minimal amount of X-ray exposure (MIMA) mostly occur in a prone posture on a Wilson table, the prone posture’s effects on spinal muscles have not been investigated. Thus, this study used ultrasound shear-wave elastography (SWE) to compare the material properties of the erector spinae and multifidus muscles when subjects lay on the Wilson table used for spinal surgery and the flat table as a control condition. Thirteen male subjects participated in the study. Using ultrasound SWE, the shear elastic moduli (SEM) of the Citation: Lim, T.H.; Lee, D.; Kim, O.; Lee, S.J. Quantification of the Elastic erector spinae and multifidus muscles were investigated. -

Relationship Between Endplate Defects, Modic Change, Facet Joint Degeneration, and Disc Degeneration of Cervical Spine
Neurospine 2020;17(2):443-452. Neurospine https://doi.org/10.14245/ns.2040076.038 pISSN 2586-6583 eISSN 2586-6591 Original Article Relationship Between Endplate Corresponding Author Defects, Modic Change, Facet Joint Dong Wuk Son https://orcid.org/0000-0002-9154-1923 Degeneration, and Disc Degeneration Department of Neurosurgery, Pusan of Cervical Spine National University Yangsan Hospital, 20 Geumo-ro, Mulgeum-eup, Yangsan 50612, Su-Hun Lee1,2, Dong Wuk Son1,2, Jun-Seok Lee1,2, Soon-Ki Sung1,2, Sang Weon Lee1,2, Korea Geun Sung Song1,2 E-mail: [email protected] 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea Received: February 11, 2020 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Revised: February 26, 2020 Hospital, Yangsan, Korea Accepted: February 27, 2020 Objective: The ‘‘disc degeneration precedes facet joint osteoarthritis’’ hypothesis and multi- dimensional analysis were actively discussed in lumbar spine. However, in cervical spine degeneration, the multifactorial analyzes of disc degeneration (DD), Modic changes (Mcs), facet degeneration, and endplate degeneration (ED) is still limited. In this cross-sectional study, we aimed to analyze the prevalence and interrelationship of cervical DD parameters. Methods: We retrospectively recruited 62 patients aged between 60 and 70 years. The disc height, segmental angle, ossified posterior longitudinal ligament (OPLL), ED, facet joint degeneration -
Scapular Dyskinesis
Scapular Dyskinesis Presented by: Scott Sevinsky MSPT Presented by: Scott Sevinsky SPT 1 What is Scapular Dyskinesis? Alteration in the normal static or dynamic position or motion of the scapula during coupled scapulohumeral movements. Other names given to this catch-all phrase include: “floating scapula” and “lateral scapular slide”.1, 2 1 Alterations in scapular position and motion occur in 68 – 100% of patients with shoulder injuries. Scapular Dyskinesis Classification System 1, 3 Pattern Definitions Inferior angle At rest, the inferior medial scapular border may be prominent dorsally. During arm motion, the inferior (type I) angle tilts dorsally and the acromion tilts ventrally over the top of the thorax. The axis of the rotation is in the horizontal plane. Medial border At rest, the entire medial border may be prominent dorsally. During arm motion, the medial scapular (type II) border tilts dorsally off the thorax. The axis of the rotation is vertical in the frontal plane. Superior border At rest, the superior border of the scapula may be elevated and the scapula can also be anteriorly (type III) displaced. During arm motion, a shoulder shrug initiates movement without significant winging of the scapula occurring. The axis of this motion occurs in the sagittal plane. Symmetric At rest, the position of both scapula are relatively symmetrical, taking into account that the dominant scapulohumeral arm may be slightly lower. During arm motion, the scapulae rotate symmetrically upward such that the (type IV) inferior angles translate laterally away from the midline and the scapular medial border remains flush against the thoracic wall. The reverse occurs during lowering of the arm. -
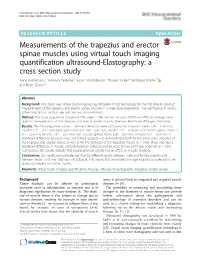
Measurements of the Trapezius and Erector Spinae Muscles Using Virtual Touch Imaging Quantification Ultrasound-Elastography
Heizelmann et al. BMC Musculoskeletal Disorders (2017) 18:370 DOI 10.1186/s12891-017-1733-8 RESEARCHARTICLE Open Access Measurements of the trapezius and erector spinae muscles using virtual touch imaging quantification ultrasound-Elastography: a cross section study Anne Heizelmann1, Sümeyra Tasdemir1, Julian Schmidberger1, Tilmann Gräter2, Wolfgang Kratzer1* and Beate Grüner3 Abstract Background: This study uses virtual touch imaging quantification (VTIQ) technology for the first time to conduct measurements of the trapezius and erector spinae muscles in a large study population. The significance of various influencing factors, such as age and sex, are also examined. Method: The study population comprised 278 subjects. The Siemens Acuson S3000 and VTIQ technology were used for measurements of the trapezius and erector spinae muscles (Siemens Healthcare, Erlangen, Germany). Results: The following mean values ± standard deviation were calculated: left trapezius: males 2.89 ± 0.38 m/s, females 2.71 ± 0.37 m/s; right trapezius: males 2.84 ± 0.41 m/s, females 2.70 ± 0.38 m/s; left erector spinae: males 2. 97 ± 0.50 m/s, females 2.81 ± 0.57 m/s; right erector spinae: males 3.00 ± 0.52 m/s, females 2.77 ± 0.59 m/s. A significant difference between male and female subjects was demonstrated both for the shear wave velocities of the trapezius and erector spinae as well as for the thickness of the trapezius muscle (p < 0.05). There was also a significant difference in muscle elasticity between subjects over 60 years of age and those under 60 (p < 0.05). Furthermore, the results indicate that regular physical activity has an effect on muscle elasticity. -

Erector Spinae Plane Block Versus Retrolaminar Block a Magnetic Resonance Imaging and Anatomical Study
Regional Anesthesia & Pain Medicine: first published as 10.1097/AAP.0000000000000798 on 1 October 2018. Downloaded from REGIONAL ANESTHESIA AND ACUTE PAIN BRIEF TECHNICAL REPORT Erector Spinae Plane Block Versus Retrolaminar Block A Magnetic Resonance Imaging and Anatomical Study Sanjib Das Adhikary, MD,* Stephanie Bernard, MD,† Hector Lopez, MD,‡ and Ki Jinn Chin, FRCPC§ As with the ESP block, it has been postulated that the clinical ef- Background and Objectives: The erector spinae plane (ESP) and fects of the retrolaminar block may be explained by spread of lo- retrolaminar blocks are ultrasound-guided techniques for thoracoabdominal cal anesthetic into the paravertebral space,6 but this mechanism wall analgesia involving injection into the musculofascial plane between has never been systematically investigated. However, there are the paraspinal back muscles and underlying thoracic vertebrae. The ESP significant anatomical and technical differences between the 2 block targets the tips of the transverse processes, whereas the retrolaminar techniques: the retrolaminar block targets the lamina instead of block targets the laminae. We investigated if there were differences in the transverse process, and thus the injection point is more medial injectate spread between the 2 techniques that would have implications and deeper. The muscle layer over the lamina and adjacent to the for their clinical effect. spinous processes is thicker, being composed of the spinalis portion Methods: The blocks were performed in 3 fresh cadavers. The ESP and of the erector spinae muscle group as well as the transversospinalis retrolaminar blocks were performed on opposite sides of each cadaver at muscle group, which comprises the multifidus, rotatores, semis- the T5 vertebral level. -

Ossification of the Posterior Longitudinal Ligament: Pathogenesis, Management, and Current Surgical Approaches
Neurosurg Focus 30 (3):E10, 2011 Ossification of the posterior longitudinal ligament: pathogenesis, management, and current surgical approaches A review ZACHARY A. SMITH, M.D.,1 COLIN C. BUCHANAN, M.D.,2 DAN RAPHAEL, P.A.-C.,1 AND LARRY T. KHOO, M.D.1 1Division of Neurosurgery, The Spine Clinic of Los Angeles, Good Samaritan Hospital, An Affiliate Hospital of the University of Southern California Medical School; and 2Department of Neurosurgery, Ronald Reagan–UCLA Medical Center, David Geffen School of Medicine at UCLA, Los Angeles, California Ossification of the posterior longitudinal ligament (OPLL) is an important cause of cervical myelopathy that results from bony ossification of the cervical or thoracic posterior longitudinal ligament (PLL). It has been estimated that nearly 25% of patients with cervical myelopathy will have features of OPLL. Patients commonly present in their mid-40s or 50s with clinical evidence of myelopathy. On MR and CT imaging, this can be seen as areas of ossification that commonly coalesce behind the cervical vertebral bodies, leading to direct ventral compression of the cord. While MR imaging will commonly demonstrate associated changes in the soft tissue, CT scanning will better define areas of ossification. This can also provide the clinician with evidence of possible dural ossification. The surgical management of OPLL remains a challenge to spine surgeons. Surgical alternatives include anterior, posterior, or circumferential decompression and/or stabilization. Anterior cervical stabilization options include cervical corpectomy or multilevel anterior cervical corpectomy and fusion, while posterior stabilization approaches include instrumented or noninstru- mented fusion or laminoplasty. Each of these approaches has distinct advantages and disadvantages.