Trans-Obturator Cable Fixation of Open Book Pelvic Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -

A Cadaveric Study of Ultrasound-Guided Subpectineal Injectate Spread Around the Obturator Nerve and Its Hip Articular Branches
REGIONAL ANESTHESIA AND ACUTE PAIN Regional Anesthesia & Pain Medicine: first published as 10.1097/AAP.0000000000000587 on 1 May 2017. Downloaded from ORIGINAL ARTICLE A Cadaveric Study of Ultrasound-Guided Subpectineal Injectate Spread Around the Obturator Nerve and Its Hip Articular Branches Thomas D. Nielsen, MD,* Bernhard Moriggl, MD, PhD, FIACA,† Kjeld Søballe, MD, DMSc,‡ Jens A. Kolsen-Petersen, MD, PhD,* Jens Børglum, MD, PhD,§ and Thomas Fichtner Bendtsen, MD, PhD* such high-volume blocks the most appropriate nerve blocks for Background and Objectives: The femoral and obturator nerves are preoperative analgesia in patients with hip fracture, because both assumed to account for the primary nociceptive innervation of the hip joint the femoral and obturator nerves have been found to innervate capsule. The fascia iliaca compartment block and the so-called 3-in-1-block the hip joint capsule.5 have been used in patients with hip fracture based on a presumption that local Several authors have since questioned the reliability of the anesthetic spreads to anesthetize both the femoral and the obturator nerves. FICB and the 3-in-1-block to anesthetize the obturator nerve.6–10 Evidence demonstrates that this presumption is unfounded, and knowledge Recently, a study, using magnetic resonance imaging to visualize about the analgesic effect of obturator nerve blockade in hip fracture patients the spread of the injectate, refuted any spread of local anesthetic to presurgically is thus nonexistent. The objectives of this cadaveric study were the obturator nerve after either of the 2 nerve block techniques.11 to investigate the proximal spread of the injectate resulting from the admin- Consequently, knowledge of the analgesic effect of an obturator istration of an ultrasound-guided obturator nerve block and to evaluate the nerve block in preoperative patients with hip fracture is nonexis- spread around the obturator nerve branches to the hip joint capsule. -

Obturator Hernia: Diagnosis and Treatment in the Modern Era
Original Article Singapore Med J 2009; 50(9) : 866 Obturator hernia: diagnosis and treatment in the modern era Mantoo S K, Mak K, Tan T J ABSTRACT Introduction: Obturator hernia is a rare variety of abdominal hernia that nonetheless is a significant cause of morbidity and mortality, especially in the elderly age group. This article aimed to review the diagnosis and management 2 of obturator hernia by describing the anatomy, - clinical presentation, predisposing factors, diagnostic modalities and management in the modern era. Fig. I Case 1. Axial CT image of the pelvis shows a left obtura - tor hernia. Methods: We managed six cases of obturator hernia between 2003 and 2006. Five out of six cases were diagnosed by a preoperative computed tomography (CT) and the sixth case was diagnosed by ultrasonography. All except one were managed by an exploratory laparotomy and repair of the hernia, and one was treated with laparoscopic repair. SI Results: Correct preoperative diagnosis was made in five out of five (100 percent) patients by clinical signs and CT of the abdomen and pelvis, and the sixth patient was operated on the basis of an ultrasonographical diagnosis and strong i A clinical suspicion. Fig. 2 Case 4. Intraoperative photograph shows the widened right obturator canal. Conclusion: We conclude that the rapid Department of evaluation by CT of the abdomen and pelvis Table I. Demographics of six patients with obturator Surgery, hernia. Alexandra and surgical intervention are possible, thereby Hospital, Patient characteristics Mean (range) 378 Alexandra reducing the morbidity and mortality of patients Road, with obturator hernia. An algorithm for the Singapore 159964 Age (years) 88.8 (76-96) management of obturator hernia is proposed. -

Anatomy of Pelvic Floor Dysfunction
Anatomy of Pelvic Floor Dysfunction Marlene M. Corton, MD KEYWORDS Pelvic floor Levator ani muscles Pelvic connective tissue Ureter Retropubic space Prevesical space NORMAL PELVIC ORGAN SUPPORT The main support of the uterus and vagina is provided by the interaction between the levator ani (LA) muscles (Fig. 1) and the connective tissue that attaches the cervix and vagina to the pelvic walls (Fig. 2).1 The relative contribution of the connective tissue and levator ani muscles to the normal support anatomy has been the subject of controversy for more than a century.2–5 Consequently, many inconsistencies in termi- nology are found in the literature describing pelvic floor muscles and connective tissue. The information presented in this article is based on a current review of the literature. LEVATOR ANI MUSCLE SUPPORT The LA muscles are the most important muscles in the pelvic floor and represent a crit- ical component of pelvic organ support (see Fig. 1). The normal levators maintain a constant state of contraction, thus providing an active floor that supports the weight of the abdominopelvic contents against the forces of intra-abdominal pressure.6 This action is thought to prevent constant or excessive strain on the pelvic ‘‘ligaments’’ and ‘‘fascia’’ (Fig. 3A). The normal resting contraction of the levators is maintained by the action of type I (slow twitch) fibers, which predominate in this muscle.7 This baseline activity of the levators keeps the urogenital hiatus (UGH) closed and draws the distal parts of the urethra, vagina, and rectum toward the pubic bones. Type II (fast twitch) muscle fibers allow for reflex muscle contraction elicited by sudden increases in abdominal pressure (Fig. -

ANATOMICAL VARIATIONS and DISTRIBUTIONS of OBTURATOR NERVE on ETHIOPIAN CADAVERS Berhanu KA, Taye M, Abraha M, Girma A
https://dx.doi.org/10.4314/aja.v9i1.1 ORIGINAL COMMUNICATION Anatomy Journal of Africa. 2020. Vol 9 (1): 1671 - 1677. ANATOMICAL VARIATIONS AND DISTRIBUTIONS OF OBTURATOR NERVE ON ETHIOPIAN CADAVERS Berhanu KA, Taye M, Abraha M, Girma A Correspondence to Berhanu Kindu Ashagrie Email: [email protected]; Tele: +251966751721; PO Box: 272 Debre Tabor University , North Central Ethiopia ABSTRACT Variations in anatomy of the obturator nerve are important to surgeons and anesthesiologists performing surgical procedures in the pelvic cavity, medial thigh and groin regions. They are also helpful for radiologists who interpret computerized imaging and anesthesiologists who perform local anesthesia. This study aimed to describe the anatomical variations and distribution of obturator nerve. The cadavers were examined bilaterally for origin to its final distribution and the variations and normal features of obturator nerve. Sixty-seven limbs sides (34 right and 33 left sides) were studied for variation in origin and distribution of obturator nerve. From which 88.1% arises from L2, L3 and L4 and; 11.9% from L3 and L4 spinal nerves. In 23.9%, 44.8% and 31.3% of specimens the bifurcation levels of obturator nerve were determined to be intrapelvic, within the obturator canal and extrapelvic, respectively. The anterior branch subdivided into two, three and four subdivisions in 9%, 65.7% and 25.4% of the specimens, respectively, while the posterior branch provided two subdivisions in 65.7% and three subdivisions in 34.3% of the specimens. Hip articular branch arose from common obturator nerve in 67.2% to provide sensory innervation to the hip joint. -

The Female Pelvic Floor Fascia Anatomy: a Systematic Search and Review
life Systematic Review The Female Pelvic Floor Fascia Anatomy: A Systematic Search and Review Mélanie Roch 1 , Nathaly Gaudreault 1, Marie-Pierre Cyr 1, Gabriel Venne 2, Nathalie J. Bureau 3 and Mélanie Morin 1,* 1 Research Center of the Centre Hospitalier Universitaire de Sherbrooke, Faculty of Medicine and Health Sciences, School of Rehabilitation, Université de Sherbrooke, Sherbrooke, QC J1H 5N4, Canada; [email protected] (M.R.); [email protected] (N.G.); [email protected] (M.-P.C.) 2 Anatomy and Cell Biology, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC H3A 0C7, Canada; [email protected] 3 Centre Hospitalier de l’Université de Montréal, Department of Radiology, Radio-Oncology, Nuclear Medicine, Faculty of Medicine, Université de Montréal, Montreal, QC H3T 1J4, Canada; [email protected] * Correspondence: [email protected] Abstract: The female pelvis is a complex anatomical region comprising the pelvic organs, muscles, neurovascular supplies, and fasciae. The anatomy of the pelvic floor and its fascial components are currently poorly described and misunderstood. This systematic search and review aimed to explore and summarize the current state of knowledge on the fascial anatomy of the pelvic floor in women. Methods: A systematic search was performed using Medline and Scopus databases. A synthesis of the findings with a critical appraisal was subsequently carried out. The risk of bias was assessed with the Anatomical Quality Assurance Tool. Results: A total of 39 articles, involving 1192 women, were included in the review. Although the perineal membrane, tendinous arch of pelvic fascia, pubourethral ligaments, rectovaginal fascia, and perineal body were the most frequently described structures, uncertainties were Citation: Roch, M.; Gaudreault, N.; identified in micro- and macro-anatomy. -

Pelvic Pain Cause, Effect and Treatment
Pelvic Pain Cause, Effect and Treatment Based on clinical research and observations of 22,600 patients over a 22 year period Pelvic Girdle 4 pelvic bones Ilae, Sacrum, Coccyx 8 joints, 2 SIJ’s, Symphasis Pubis, Sacrococcygeal, 2 Iliolumbar, 2 Hip Joints The Sacroiliac joints are triplanar In order to fully correct pelvic position and biomechanics, all 8 joints need to be addressed Posterior pelvic pain • Lumbopelvic pain (torsioned uterosacral ligaments, labour) • Dysmenorrhea • Ligamentous pain (iliolumbar/sacroiliac) • Joint surface pain (teeth on teeth) • Quadratus lumborum pain • Sciatic pain (compression piriformis/obt. internus compression) • Sciatic pain (lumbosacral plexus) • Lumbopelvic pain (labour) • Dyspareunia (Asymmetrical pelvic floor) Pelvic Floor Asymmetry caused by left side flexed and rotated sacrum and coccyx and low left ilium. Shortens and torsions left pelvic floor muscle. Lengthens, stretches and torsions right pelvic floor muscles. Causes Wide and varied • Foetus inutero position • Any significant trauma (e.g. falling of horse; down stairs) • Whiplash • Fractures • Falls on buttocks • Sporting injuries • Abdominal and pelvic surgery • Pelvic infections Common Pelvic Positions Sacral restrictions Ilial bilateral downslips (88%) Ilial bilateral upslips (9%) Ilial bilateral upslip/downslip (3%) • Left down/right up Based on 22,600 patients Green = sacral base and PSIS before treatment Black = after treatment This joint excursion is only possible due to the 3D SIJS Autonomic nervous system activation and reaction -

Anatomical Considerations on Surgical Implications of Corona Mortis: an Indian Study
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Firenze University Press: E-Journals IJAE Vol. 122, n. 2: 127-136, 2017 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research article - Basic and applied anatomy Anatomical considerations on surgical implications of corona mortis: an Indian study Minnie Pillay*, Tintu T. Sukumaran, Mahendran Mayilswamy Department of Anatomy, Amrita Institute of Medical Sciences, Amrita University, Kochi, India Abstract The blood vessels traversing the superior pubic ramus are usually vascular connections between obturator and external iliac systems of vessels. Dislocated fractures or iatrogenic injury can cause life threatening bleeding and hence these vascular anomalies are referred to as coro- na mortis meaning ‘crown of death’. Except for a case report, no study on corona mortis has been attempted in India so far and hence the present study was intended at exploring the pos- sible variations, both morphological and topographical, of these vascular connections in Indian population through cadaveric dissection. 24 adult cadavers dissected bilaterally (48 hemipelves) and 19 random hemipelves available in the Department of Anatomy were considered for the study.The vascular connections observed were classified as arterial, venous or both (Types I, II and III). Type III was further classified into subtypes a, b, c, d and e based on various combi- nations of the first two types. In a total of 67 pelvic halves corona mortis was detected in 56 (83.58%) specimens: arterial 7/56 (12.5%), venous 34/56 (60.7%) and both arterial and venous in 15/56 (26.78%) specimens respectively. -
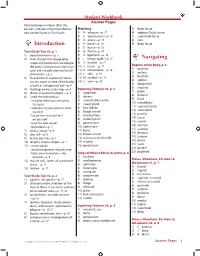
Student Workbook Answer Pages Italicized Page Numbers After the Answers Indicate Where the Informa- Matching 5) Deep Fascia Tion Can Be Found in Trail Guide
Student Workbook Answer Pages Italicized page numbers after the answers indicate where the informa- Matching 5) deep fascia tion can be found in Trail Guide. 1) N adipose—p. 17 6) adipose (fatty) tissue 2) F aponeurosis—p. 13 7) superficial fascia 3) D artery—p. 16 8) skin 4) H bone—p. 10 9) deep fascia Introduction 5) E bursa—p. 16 Tour Guide Tips #1, p. 1 6) B fascia—p. 14 1) bony landmarks—p. 2 7) G ligament—p. 13 2) Even though the topography, 8) I lymph node—p. 17 Navigating shape and proportion are unique, 9) A muscle—p. 11 Regions of the Body, p. 6 the body’s composition and struc- 10) J nerve—p. 17 1) pectoral tures are virtually identical on all 11) K retinaculum—p. 15 2) axillary individuals.—p. 2 12) L skin—p. 10 3) brachial 3) To examine or explore by touch- 13) M tendon—p. 13 4) cubital ing (an organ or area of the body), 14) C vein—p. 16 5) abdominal usually as a diagnostic aid—p. 4 6) inguinal 4) locating, aware, assessing—p. 4 Exploring Textures #1, p. 3 7) pubic 5) directs movement, depth.—p. 4 1) epidermis 8) femoral 6) • read the information 2) dermis 9) facial • visualize what you are trying 3) arrector pili muscle 10) mandibular to access 4) sweat gland 11) supraclavicular • verbalize to your partner what 5) hair follicle 12) antecubital you feel 6) blood vessels 13) patellar • locate the structure first 7) muscle fibers 14) crural on yourself 8) endomysium 15) cranial • read the text aloud 9) perimysium 16) cervical • be patient—p. -

The Anatomy and Clinical Implications of the Obturator Nerve and Its Branches
The anatomy and clinical implications of the obturator nerve and its branches by Zithulele Nkosinathi Tshabalala Dissertation submitted in full fulfilment of the requirements for the degree Master of Science in Anatomy In the Faculty of Health Science University of Pretoria Supervisor: Dr A-N van Schoor Co-supervisor: Mrs R Human-Baron Co-supervisor: Mrs S van der Walt 2015 DECLARATION OF ORIGINALITY UNIVERSITY OF PRETORIA The Department of Anatomy places great emphasis upon integrity and ethical conduct in the preparation of all written work submitted for academic evaluation. While academic staff teach you about referencing techniques and how to avoid plagiarism, you too have a responsibility in this regard. If you are at any stage uncertain as to what is required, you should speak to your lecturer before any written work is submitted. You are guilty of plagiarism if you copy something from another author’s work (e.g. a book, an article or a website) without acknowledging the source and pass it off as your own. In effect you are stealing something that belongs to someone else. This is not only the case when you copy work word-for-word (verbatim), but also when you submit someone else’s work in a slightly altered form (paraphrase) or use a line of argument without acknowledging it. You are not allowed to use work previously produced by another student. You are also not allowed to let anybody copy your work with the intention of passing if off as his/her work. Students who commit plagiarism will not be given any credit for plagiarised work. -

The Anatomical “Core”: a Definition and Functional Classification
Osteopathic Family Physician (2011) 3, 239-245 The anatomical “core”: a definition and functional classification John J. Dougherty, DO, FACOFP, FAOASM From the Department of Family Medicine, Kansas City University of Medicine and Biosciences, Kansas City, MO. KEYWORDS: The anatomic core is important in the functional stabilization of the body during static and dynamic Core; movement. This functional stabilization is an integral component of proprioception, balance perfor- Static function; mance, and compensatory postural activation of the trunk muscles. The structures that define the core Dynamic function; and its functions are presented here. By understanding the contributing components and responsibilities Sensory-motor control of the core, it is hoped that the physician will have a better understanding of core function as it relates to the performance of their patients’ activities of daily living. © 2011 Elsevier Inc. All rights reserved. Core training has found its way into the lexicon of functional unit, synergistically adjusting the entire body to countless exercise regimens. However, clinically there has maintain balance, postural stabilization, and mobility. These been little comprehensive definition and even less practical abilities are essential in the performance of basic activities characterization of this “core.” The word core derives from of daily living (ADLs).7 the Greek word kormos, which loosely translates to “trunk Neurologic and musculoskeletal impairments can alter of a tree.” An additional word origin comes from the Span- these normal biomechanical relationships.8-10 Such impair- ish word for heart, corazon. George Lucas selected “Cora- ment effects a functional shift of the structural burden to the zon” as the name for the planet at the center of his “Star components of the core.1 The resultant alterations impose Wars” universe. -

Sample Notes
1 HBS2ALT: Sample Notes Gluteal Osteology and Overview Bony features of the gluteal region correspond to those of the posterior pelvis, particularly the surface of the ilium and ischium - Iliac Crest → from ASIS to PSIS - Ischium: Greater Sciatic Notch, Ischial Spine, Lesser Sciatic Notch and Ischial Tuberosity Ligaments 1. Posterior Sacroiliac Ligament. Function: Stabilises the SIJ 2. Sacrotuberous Ligament: Posterior/Lateral Sacrum, Coccyx, SIJ to Ischial Tuberosity 3. Sacrospinous Ligament:/Posterior/Lateral Sacrum to Ischial Spine - Broad structure of ligament 2&3 allows muscles to attach. (Most notably gluteus maximus) Gluteal Region Surface Anatomy - Exists from level of the iliac crest superiorly to Gluteal Folds inferiorly. - Exists from intergluteal/natal/gluteal cleft medially to the greater trochanter laterally. Skin: - coarse and thick particularly in males Adipose - hypodermis (formerly known as superficial fascia). Characteristic shape of buttocks is largely due to the pad of adipose tissue in the gluteal region. Both males and females deposit adipose in the gluteal region. This deposition can be highly variable between genders. Deep Fascia - Fascia Lata- deep fascia of the gluteal region and thigh→ Continuation of the fascia of the thigh (also called the fascia lata). Encircles the thigh and covers the gluteal region. Attaches to bones prominances and also encloses the gluteus maximus and tensor fascia lata muscles, both muscles insert into the iliotibial tract. - Iliotibial tract (ITT) is presented as a lateral thickening of the fascia lata, as it extends laterally from the ilium to the tibia. - Although its superficial, it blends with the lateral intermuscular septum (IMS) of the thigh. - The lateral intermuscular septum attaches to the linea aspera on the posterior femur.