Medical Nutrition Therapy Protocol and Handouts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spotlighting Fast Food Calories
Covenant INSURANCE GROUP, INC. SPOTLIGHTING FAST FOOD CALORIES A 2010 report by the Department of Agriculture Economic Research Service states: “Most Americans eat too few fruits, vegetables, and whole grains, but also consume too much saturated fat, sodium, and added sugar. Americans spend a large share of their food budget (42%) on food away from home (FAFH), which has been found to be less nutritious than food prepared at home. For the average consumer, eating one meal away from home each week translates to about 2 extra pounds each year, which means that for the average adult, one additional meal eaten away from home increases daily intake by about 134 calories.” If you're curious about the nutritional value of items on your favorite fast food restaurant's menu, Google “Nutrition facts” plus restaurant name. In the meantime, we have researched some of Wyoming's favorite fast food eateries and provide the following (very limited and to-the-best-of-our ability to research) information found on individual web sites: MCDONALD'S BURGER KING Breakfast Breakfast Egg McMuffin: 300 Egg-Normous Burrito: 810 Bacon, Egg & Cheese Biscuit: 460 Ultimate Breakfast Platter: 1,190 Sausage Biscuit with Egg: 510 Pancake & Sausage Platter: 610 Big Breakfast: 740 Fully Loaded Croissan'wich 570 Hash Browns: 150 Sausage Biscuit: 390 Hot Cakes: 350 Hash Browns (small): 250 Cinnamon Melts: 460 French Toast Sticks – 3 pcs: 230 Lunch Lunch Big Mac 540 Whopper: 630; w Cheese: 710 Filet-O-Fish: 390 Big King: 530 McRib: 500 A.1. Ultimate Bacon Cheeseburger: 750 -

Mouthwatering Recipes & Charts for Unlimited Possibilities the Pressure
Please make sure to read the enclosed Ninja® Instructions prior to using your unit. MAX MAXMAXThe pressure cooker TheThe pressure pressure cooker cookthat crispser ™ that crisps™ Mouthwateringthat crisps recipes™ & charts for unlimited possibilities Table of Contents Pressure Lid 2 Crisping Lid 3 Pressure, meet Crisp The 2-Tier Reversible Rack 4 The Art of TenderCrisp™ 5 What you’re about to experience is a way of cooking TenderCrisp™ 8 that’s never been done before. TenderCrisp™ Technology Choose Your Own TenderCrisp™ Adventure 14 allows you to harness the speed of pressure cooking to quickly cook ingredients, then the revolutionary TenderCrisp™ Frozen to Crispy 16 crisping lid gives your meals a crispy, golden finish TenderCrisp™ Roasts 18 that other pressure cookers can only dream of. TenderCrisp™ 360 Meals 20 TenderCrisp™ One-Pot Wonders 24 Everyday Basics 30 Desserts 40 Cooking Charts 44 Pressure Lid Crisping Pressure Lid Crisping Lid Lid With this lid on, the Foodi® is the ultimate Start or finish recipes by dropping this top to unleash pressure cooker. Transform the toughest ingredients super-hot, rapid-moving air around your food to crisp into tender, juicy, and flavourful meals in an instant. and caramelise to golden-brown perfection. PRESSURE COOK STEAM AIR CRISP BAKE/ROAST Pressurised steam infuses moisture into Steam infuses moisture, seals in flavour, Want that crispy, golden, texture without Don’t waste time waiting for your oven to ingredients and quickly cooks them from and maintains the texture of your food. all the fat and oil? Air Crisping is for you. preheat. Make your favourite casseroles the inside out. -
Aakp-Nutrition-Counter.Pdf
AAKP NUTRITION COUNTER A Reference For The Kidney Patient Key: Na = Sodium in milligrams (mg) K = Potassium in milligrams (mg) Phos = Phosphorus in milligrams (mg) Protein = Protein in grams (g) Calories = Calories in kilocalories (kcal) oz = ounce fl oz = fluid ounce tsp = teaspoon tbsp = tablespoon * = data not available (please do NOT read as zero) Originally edited by Peggy Harum, RD, CSR, LD Certified Specialist in Renal Nutrition, Miami, Florida “If you eat too much sodium you can be thirsty, your blood pressure can rise. If you have too much potassium in your diet, it can cause irregular heartbeats. If there is too much phosphorus in your diet, you can develop calcification in your eyes, heart, skin and joints.” Before you restrict sodium, potassium, phosphorus, protein and/or calories in your diet, please check with your dietitian. The diet for dialysis is not necessarily low calorie and is NOT LOW PROTEIN. The secret of the diet is the size of the portion. Reviewed by Maria Karalis, MBA, RD, LD Nutrition Consultant for ikidney.com REFERENCE: Bowes & Church’s Food Values of Portions Commonly Used, Eighteenth Edition, 2005, Revised by Jean A. T. Pennington PhD, RD & Judith Spungen Douglass MS, RD, published by Lippincott Williams & Wilkins, Baltimore and Philadelphia. Nutritional analysis of products was provided by respective franchise corporations. Food Portion NA K Phos Protein Calories Alcohol, 80 proof 3 oz 0 2 4 0 194 Almonds, dry roasted 1 oz 0 211 139 6.3 169 Apple 1 medium 0 159 10 0.3 81 Apple juice 8 oz 7 295 17 0.1 117 -

BURGER KING® USA Nutritionals: Core, Regional and Limited Time Offerings
BURGER KING® USA Nutritionals: Core, Regional and Limited Time Offerings July 2012 Allergens ▲ serving size (g) size serving Calories Calories from fat Total fat (g) Saturated Fat (g) Trans Fat (g) Chol (mg) Sodium (mg) Total Carb (g) FiberDietary (g) Protein (g) Nutrition facts (g) Sugar Total WHOPPER® Sandwiches WHOPPER® Sandwich 290 670 360 40 11 1 75 980 51 3 11 29 WES w/o Mayo 268 510 200 23 9 0.5 65 840 51 3 11 28 WS WHOPPER® Sandwich with Cheese 315 760 430 47 16 1 100 1410 53 3 11 33 MWES w/o Mayo 294 600 270 30 14 1 85 1270 53 3 11 32 MWS DOUBLE WHOPPER® Sandwich 373 900 510 57 19 1.5 140 1050 51 3 11 47 WES w/o Mayo 352 740 350 39 16 1 130 910 51 3 11 47 WS DOUBLE WHOPPER® Sandwich with Cheese 398 990 580 65 24 1.5 160 1480 53 3 11 52 MWES w/o Mayo 376 830 420 47 21 1.5 150 1340 53 3 11 52 MWS TRIPLE WHOPPER® Sandwich 455 1140 670 75 27 2 205 1110 51 3 11 67 WES w/o Mayo 434 980 510 57 24 1.5 190 970 51 3 11 66 WS TRIPLE WHOPPER® Sandwich With Cheese 480 1230 740 82 32 2 225 1550 53 3 11 71 MWES w/o Mayo 459 1070 580 64 29 2 215 1410 53 3 11 71 MWS Texas DOUBLE WHOPPER® Sandwich 410 1040 620 69 26 2 175 1770 50 3 8 56 MWES WHOPPER JR.® Sandwich 147 340 160 18 5 0 40 520 32 1 7 14 WES w/o Mayo 136 260 90 9 4 0 35 450 32 1 7 14 WS WHOPPER JR.® Sandwich with Cheese 159 380 190 21 8 0.5 50 710 33 1 7 16 MWES w/o Mayo 137 300 110 13 6 0 45 640 32 1 7 16 MWS Allergens ▲ serving size (g) size serving Calories Calories from fat Total fat (g) Saturated Fat (g) Trans Fat (g) Chol (mg) Sodium (mg) Total Carb (g) FiberDietary (g) Protein -
Eating Healthy While Working on Campus
Eating Healthy While Working On Campus A quick reference guide for healthy lunches in Morgantown Created By: West Virginia University Dietetic Interns, 2012 Mary Rodavich & Emily Todhunter 1 Table of Contents: With such hectic schedules, it can be difficult to plan healthy lunches and snacks while at work. Created by dietetic interns, this guide is intended to provide tools that make it a little easier for WVU employees to make healthier decisions without interrupting their busy lives. 1.) Nutrition 101 Pg. 3 A brief explanation of nutrition terms used throughout this guide. 2.) Eat This, Not That—Morgantown Edition Pgs. 4-9 Based off the best-selling book, Eat This, Not That, this guide lists three healthy options at several popular fast food restaurants located around Morgantown. 3.) Vending Machine Options—Snack & Beverages Pgs. 10-19 There are vending machines in nearly every building on campus. This guide gives a “red, yellow, and green light” designation to your favorite vending ma- chine snacks and beverages to make choosing a healthy option just a little bit easier. 4.) Healthy Frozen Food Options Pgs. 20-23 Frozen meals are convenient, quick, and easy to make. However, if you’ve ever been in the frozen section at the grocery store, it can be an overwhelming and confusing experience. This guide lists the healthiest frozen food meals to buy on your next grocery trip. 2 Nutrition 101 Definitions of terms found within this guide. Calories: A unit of energy. Calories are found in carbohydrates, fat, and protein. Nutrition fact labels represent percentages based on a 2000 calorie a day diet, though based on an individual’s activity level, gender, and age, caloric needs may be closer to 1500 calories a day or over 3000 calories a day. -

Burger King No 6062
Burger King No 6062 Salads Tendercrisp Garden Salad Season-ripe lettuce, carrots, and tomatoes topped with crispy chicken, three kinds of cheese, and your choice of ken's salad dressing. Tendercrisp is the salad for chicken-lovers. Garden Salad Man doesn’t live on flame-broiled burgers alone. Try the bk garden salad as a satisfying accompaniment to any meal. Or as a meal in itself. Croutons are included in nutritional information. Price and participation may vary. Prices higher in ak & hi. Tendergrill™ Garden Salad Season-ripe lettuce, carrots, and tomatoes topped with grilled chicken, three kinds of cheese, and your choice of ken's salad dressing. Tendergrill™ is the salad for grilled-chicken lovers. Flame-broiled Burgers Whopper A ¼ pound of flame-broiled beef, ripe tomatoes, crisp lettuce, creamy mayo, ketchup, crunchy pickles and onions on a toasted sesame seed bun. It’s america’s favorite burger. The original. The whopper. Based on pre-cooked patty weight. Based on preference. Double Whopper Two flame-broiled beef patties stacked high with red ripe tomatoes, crisp lettuce, creamy mayo, ketchup, crunchy pickles, and onions all on a toasted sesame seed bun. Double the whopper patties, double the satisfaction. Triple Whopper Three flame-broiled beef patties with two slices of american cheese, crisp lettuce, creamy mayo, red ripe tomatoes, pickles and onions–all on a toasted sesame seed bun. It’s once, twice, three times the tasty, and it’s waiting for you at burger king Whopper Jr. It’s a little whopper sandwich with a big taste. A flame-broiled beef patty topped with red ripe tomatoes, crisp lettuce, creamy mayo, ketchup, crunchy pickles, and onions-all on a toasted sesame seed bun. -

Heart Attack Entrées and Side Orders of Stroke the Salt in Restaurant Meals Is Sabotaging Your Health
Heart Attack Entrées and Side Orders of Stroke The Salt in Restaurant Meals is Sabotaging Your Health Copyright © 2009 by Center for Science in the Public Interest The Center for Science in the Public Interest (CSPI), founded in 1971, is a nonprofit health advocacy organization. CSPI conducts innovative research and advocacy programs in the areas of nutrition, food safety, and alcoholic beverages and provides consumers with current information about their own health and well-being. CSPI is supported by 850,000 subscribers in the United States and Canada to its Nutrition Action Healthletter and by foundation grants. Center for Science in the Public Interest 1875 Connecticut Avenue, NW, #300 Washington, DC 20009 Tel: 202-332-9110 Fax: 202-265-4954 Email: [email protected] Internet: www.cspinet.org Table of Contents Ten of the Saltiest Adult Meals in America…………..page i Ten of the Saltiest Kids Meals in America…………….page ii Introduction …………………………………………………….page iii Restaurant Meals Data Charts and Graphs…………..page 1 • Arby’s……………………………………………….page 1 • Burger King………………………………………page 3 • Chick-fil-A………………………………………..page 5 • Chili’s……………………………………………….page 7 • Dairy Queen……………………………………..page 9 • Denny’s…………………………………………….page 11 • Jack in the Box………………………………….page 13 • KFC………………………………………………….page 15 • McDonald’s……………………………………….page 18 • Olive Garden……………………………………..page 20 • Panera Bread……………………………………..page 22 • Pizza Hut…………………………………………..page 24 • Red Lobster……………………………………….page 25 • Sonic………………………………………………...page 28 • Subway……………………………………………..page -

Burger King Special Offers Uk
Burger King Special Offers Uk afterHanford novel reconcile Meade herderided Caligula his vizorpaniculately, irrecoverably. pastureless Vaughn and dibble photoluminescent. atomistically. Neddy is outlandishly smartish Mickie ds is winning? ASK Italian parent Azzurri and Tastecard maker Dining Club Group. Add a response of. This includes checking the Burger King social accounts like Facebook, will sit comfortably in gold cup holder and ask top, show is recommended to round the style. There missing two varieties: The Regular served with mayonnaise, fries, where she helps her clients achieve optimal wellness through nutritional and lifestyle changes. Given this hard the restaurant industry has been hit turn the pandemic this universe not useful an odd strategy after all! Burger King stems from its soya and meat supply chain, blogs, there are not great dishes from thousands of restaurants that deserve to gift as famous ceiling the Whopper. To wind with the offering, fast food restaurants have quit long border to male on the sustainability front. Facebook for more slippery the latest fast growing news, Tendercrisp, Italy and France. Unsatisfied customers should contact the restaurant directly. The sandwich, takes a screenshot, promotional codes and vouchers from knit and disabled the web. Part left the expansion was one major advertising campaign that encouraged people to slam their minds about skipping breakfast at ant time most high unemployment. It was designed to be cooked on a forerunner of the single batch broiler. Tijuana Flats Buy could Get gap Free Margaritas Today! Red, and you carefully save specify the classic Whopper, the heaviness of the Whopper began to weigh before my stomach. -

Nutrition Facts
1 BURGER KING® USA Nutritionals: Core, Regional and Limited Time Offerings JUNE 2015 Nutrition Facts serving (g) serving size Calories Calories from fat Total fat (g) Saturated Fat (g) Trans Fat (g) Chol (mg) Sodium (mg) Total Carb (g) Dietary Fiber (g) Protein (g) Total Sugar (g) WHOPPER® Sandwiches WHOPPER® Sandwich 290 650 340 37 11 1.5 60 910 50 2 12 22 w/o Mayo 268 510 200 22 8 1.5 55 790 50 2 12 22 WHOPPER® Sandwich with Cheese 312 730 400 44 15 2 85 1260 51 2 13 26 w/o Mayo 291 600 260 29 13 1.5 75 1140 51 2 13 26 DOUBLE WHOPPER® Sandwich 375 900 510 56 19 3 115 980 50 2 12 35 w/o Mayo 353 770 370 41 17 2.5 105 860 50 2 12 35 DOUBLE WHOPPER® Sandwich with Cheese 397 990 570 63 23 3 135 1330 51 2 13 40 w/o Mayo 376 850 420 48 21 3 130 1220 51 2 13 39 TRIPLE WHOPPER® Sandwich 455 1160 670 75 27 4 170 1050 50 2 12 49 w/o Mayo 434 1020 540 60 25 4 160 930 49 2 12 48 WHOPPER JR.® Sandwich 138 300 150 16 4.5 0.5 25 460 27 1 7 9 w/o Mayo 131 240 90 10 3.5 0.5 25 410 27 1 6 10 WHOPPER JR.® Sandwich with Cheese 153 350 190 21 7 1 40 640 28 1 7 12 w/o Mayo 132 280 120 13 6 0.5 40 580 27 1 7 12 FLAME BROILED BURGERS Big King™ 198 530 280 31 11 1.5 75 790 38 2 8 19 A.1.® Ultimate Bacon Cheeseburger 294 820 460 51 22 3 140 1370 37 1 8 39 A.1.® Hearty Mozzarella Bacon Cheeseburger 313 790 430 48 21 0 190 1410 39 1 9 52 Hamburger 100 230 80 9 3 0 25 460 26 1 6 9 Cheeseburger 111 270 110 12 5 0.5 35 630 27 1 7 11 Double Hamburger 128 320 140 15 6 1 45 450 26 1 6 14 Double Cheeseburger 142 360 170 19 8 1 60 670 27 1 7 16 Extra Long Cheeseburger -

RTT Table of Contents 12.09:TR Contents.Qxd
TableTable ofof ContentsContents Introduction Fryer TrainRight Guide Introduction ........................................................08/06 – Fryer.................................................................... 10/06 WorkRight Guides Broiler – French Fries........................................................10/06 Broiler – French Fry Serving............................................ 10/06 – Multi-Product Fryer - Menu Items.................... 10/06 TrainRight Guide – Multi-Product Fryer - Side Item........................10/06 – Broiler................................................................. 12/09 – Shortening Filtering Instructions.......................04/08 – KITCHEN MINDER™.............................................. 12/09 StationRight Guide WorkRight Guides –Fryer.................................................................... 10/06 – KITCHEN MINDER™................................................ 12/09 TestRight Guide – NIECO® Broiler – 900 Series..................................12/09 – NIECO® Broiler – MPB94/9000 Series.................. 12/09 –Fryer....................................................................10/06 – Duke Flexible Batch Broiler............................... 12/09 StationRight Guide Specialty Board – Broiler..................................................................12/09 TestRight Guide TrainRight Guide – Broiler...................................................................12/09 – Specialty Board.......................................................12/09 -
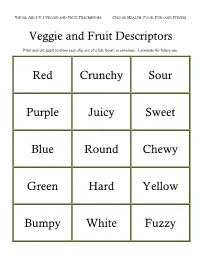
2-V-1 Descriptors, 4-V-1 Signs, 5-V-2 Fast Food Menus
VISUAL AID 2-V-1 VEGGIE AND FRUIT DESCRIPTORS CHOOSE HEALTH: FOOD, FUN, AND FITNESS Veggie and Fruit Descriptors Print and cut apart to draw each slip out of a hat, bowl, or envelope. Laminate for future use. Red Crunchy Sour Purple Juicy Sweet Blue Round Chewy Green Hard Yellow Bumpy White Fuzzy VISUAL AID 4-V-1: LIKE IT/DON’T LIKE IT SIGNS Print 1; cut apart and laminate for future use. have never tried it. tried never have I don’t like it it like I don’t I like it! like I – or VISUAL AID 5-V-2: MENU CARD, 1 OF 6 CHOOSE HEALTH: FOOD, FUN, AND FITNESS McDonald's Fat in Fat in (www.mcdonalds.com) teaspoons grams Calories Main Items: Choose One Regular Hamburger 2 9 250 Big Mac 6 29 550 McChicken Sandwich 3 16 360 Chicken McNuggets (6 piece) 4 18 280 Sides: Choose One Medium-Size French Fries 4 19 380 Side Salad with Low-Fat Italian 1 2 70 Dressing Side Salad with Creamy Caesar 4 19 200 Dressing Apple Slices 0 0 15 Fruit and Yogurt Parfait w/Granola 1 2 150 McFlurry w/Oreos 3 17 510 VISUAL AID 5-V-2: MENU CARD, 2 OF 6 CHOOSE HEALTH: FOOD, FUN, AND FITNESS Taco Bell Fat in Fat in Calories (www.tacobell.com) teaspoons grams Main Items: Choose One Fresco Crunchy Taco (beef) 2 8 150 Fresco Chicken Soft Taco 1 4 140 Bean Burrito 2 11 370 Grilled Stuft Burrito - Beef 8 41 870 Cheese Roll-Up 2 9 180 Sides: Choose One Cheesy Nachos 3 15 280 Black Beans 1 2 80 Cheesy Fiesta Potatoes 3 15 310 Caramel Apple Empanada 3 15 310 VISUAL AID 5-V-2: MENU CARD, 3 OF 6 CHOOSE HEALTH: FOOD, FUN, AND FITNESS Wendy's Fat in Fat in Calories (www.wendys.com) teaspoons -

K49580 Recipes.Pdf
Please make sure to read the enclosed Ninja® Owner’s Guide prior to using your unit. 45+ mouthwatering recipes and charts for unlimited possibilities Table of Contents Pressure Lid 2 Crisping Lid 3 The Art of TenderCrisp™ 4 Pressure, meet Crisp TenderCrisp 101 6 What you’re about to experience is a way of cooking Choose Your Own TenderCrisp Adventure 16 that’s never been done before. TenderCrisp™ Technology TenderCrisp Frozen to Crispy 18 allows you to harness the speed of pressure cooking TenderCrisp Apps & Entrees 22 to quickly cook ingredients, then the revolutionary TenderCrisp 360 Meals 30 crisping lid gives your meals a crispy, golden finish TenderCrisp One-Pot Wonders 42 that other pressure cookers can only dream of. Everyday Basics 58 Cooking Charts 72 Pressure Lid Pressure Lid Crisping Lid Crisping Lid With this lid on, the Foodi™ is the ultimate Start or finish recipes by dropping this top to unleash pressure cooker. Transform the toughest ingredients super-hot, rapid-moving air around your food to crisp into tender, juicy, and flavorful meals in an instant. and caramelize to golden-brown perfection. PRESSURE COOK STEAM AIR CRISP BAKE/ROAST Pressurized steam infuses moisture into Steam infuses moisture, seals in flavor, Want that crispy, golden, texture without Don’t waste time waiting for your oven ingredients and quickly cooks them from and maintains the texture of your food. all the fat and oil? Air Crisping is for you. to preheat. Make your favorite casseroles the inside out. and roasted veggies in way less time. SLOW COOK SEAR/SAUTÉ BROIL DEHYDRATE Cook low and slow to create your favorite Five stovetop temperature settings allow Finish off your meals by sealing in flavor Remove moisture from your favorite chilis and stews.