Pathology of Soft Tissue and Skin. Bone and Joint Pathology. Pathology of Soft Tissue and Skin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Pathomorpholog.Pdf
Ukrаiniаn Medicаl Stomаtologicаl Аcаdemy THE DEPАRTАMENT OF PАTHOLOGICАL АNАTOMY WITH SECTIONSL COURSE MАNUАL for the foreign students GENERАL PАTHOMORPHOLOGY Poltаvа-2020 УДК:616-091(075.8) ББК:52.5я73 COMPILERS: PROFESSOR I. STАRCHENKO ASSOCIATIVE PROFESSOR O. PRYLUTSKYI АSSISTАNT A. ZADVORNOVA ASSISTANT D. NIKOLENKO Рекомендовано Вченою радою Української медичної стоматологічної академії як навчальний посібник для іноземних студентів – здобувачів вищої освіти ступеня магістра, які навчаються за спеціальністю 221 «Стоматологія» у закладах вищої освіти МОЗ України (протокол №8 від 11.03.2020р) Reviewers Romanuk A. - MD, Professor, Head of the Department of Pathological Anatomy, Sumy State University. Sitnikova V. - MD, Professor of Department of Normal and Pathological Clinical Anatomy Odessa National Medical University. Yeroshenko G. - MD, Professor, Department of Histology, Cytology and Embryology Ukrainian Medical Dental Academy. A teaching manual in English, developed at the Department of Pathological Anatomy with a section course UMSA by Professor Starchenko II, Associative Professor Prylutsky OK, Assistant Zadvornova AP, Assistant Nikolenko DE. The manual presents the content and basic questions of the topic, practical skills in sufficient volume for each class to be mastered by students, algorithms for describing macro- and micropreparations, situational tasks. The formulation of tests, their number and variable level of difficulty, sufficient volume for each topic allows to recommend them as preparation for students to take the licensed integrated exam "STEP-1". 2 Contents p. 1 Introduction to pathomorphology. Subject matter and tasks of 5 pathomorphology. Main stages of development of pathomorphology. Methods of pathanatomical diagnostics. Methods of pathomorphological research. 2 Morphological changes of cells as response to stressor and toxic damage 8 (parenchimatouse / intracellular dystrophies). -

Wednesday Slide Conference 2008-2009
PROCEEDINGS DEPARTMENT OF VETERINARY PATHOLOGY WEDNESDAY SLIDE CONFERENCE 2008-2009 ARMED FORCES INSTITUTE OF PATHOLOGY WASHINGTON, D.C. 20306-6000 2009 ML2009 Armed Forces Institute of Pathology Department of Veterinary Pathology WEDNESDAY SLIDE CONFERENCE 2008-2009 100 Cases 100 Histopathology Slides 249 Images PROCEEDINGS PREPARED BY: Todd Bell, DVM Chief Editor: Todd O. Johnson, DVM, Diplomate ACVP Copy Editor: Sean Hahn Layout and Copy Editor: Fran Card WSC Online Management and Design Scott Shaffer ARMED FORCES INSTITUTE OF PATHOLOGY Washington, D.C. 20306-6000 2009 ML2009 i PREFACE The Armed Forces Institute of Pathology, Department of Veterinary Pathology has conducted a weekly slide conference during the resident training year since 12 November 1953. This ever- changing educational endeavor has evolved into the annual Wednesday Slide Conference program in which cases are presented on 25 Wednesdays throughout the academic year and distributed to 135 contributing military and civilian institutions from around the world. Many of these institutions provide structured veterinary pathology resident training programs. During the course of the training year, histopathology slides, digital images, and histories from selected cases are distributed to the participating institutions and to the Department of Veterinary Pathology at the AFIP. Following the conferences, the case diagnoses, comments, and reference listings are posted online to all participants. This study set has been assembled in an effort to make Wednesday Slide Conference materials available to a wider circle of interested pathologists and scientists, and to further the education of veterinary pathologists and residents-in-training. The number of histopathology slides that can be reproduced from smaller lesions requires us to limit the number of participating institutions. -

Tern, It Was Felt of Use to Record the Experience in This Matter
PERSISTENT "INSECT BITES" (DERMAL EOSINOPHILIC GRANU- LOMAS) SIMULATING LYMPHOBLASTOMAS, HISTIOCYTOSES, AND SQUAMOUS CELL CARCINOMAS * ARrHUR C. ALLEN, MD. t (From the Army instute of Pathology, Washingtox 25, D.C.) In 1942, opportunity was afforded at the Army Institute of Pathol- ogy to review the histologic slides of a lesion said to have been pro- duced by a tick bite. The microscopic sections seemed at the time indistinguishable from mycosis fungoides or Hodgkin's disee, espe- cialy in view of the presence of multiple lesions in the patient. How- ever, following the study of the cutaneous reactions to arthropods (ticks, mosquitoes, and chiggers), it was quickly appreciated that not only were these diagnoses of neoplasia wrong but that the misinterpretation of these reactions was a common and serious error.' The errors in- volved the misconstruction not only of the dermal reaction but also of the epidermal changes. The latter response was confused with squa- mous cell carcinoma; the dermal infitrate was mistaken for mycosis fungoides, Hodgkin's disease, lymphosacoma, giant follicular lympho- blastoma, and Spiegler-Fendt sarcoid. Undoubtedly the principal rea- son for the failure to attnbute these reactions properly to bites of arachnida and insects was referable to the general impression, despite dear-cut cinical histories, that such reactions last only for days, whereas, in truth, they may persist for as long as 2 years. More re- cently, the problem has been further complicated by introduction into the literature of a lesion called "eosinophilic granuloma of skin," an entity of questionable nosologic justification.' Therefore, because of the major importance of establishing a definitive diagnosis and because of the interest in the pathogenesis of a much mimicked histologic pat- tern, it was felt of use to record the experience in this matter. -
WSC 13-14 Conf 13 Layout
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2013-2014 Conference 13 29 January 2014 CASE I: AVC C3670-13 (JPC 4032590). for 10-12 days and then stopped eating. Most recently, the dog developed diarrhea, non- Signalment: 10-year-old male castrated Shetland regenerative anemia and glucosuria. An Sheepdog (Canis familiaris). abdominal ultrasound revealed a severe and diffuse mottled appearance of the liver with a History: This dog was diagnosed with honeycomb pattern. Liver aspirates were taken dermatomyositis as a puppy; it had footpad for cytology assessment and the footpads were lesions characterized by hyperkeratosis, erythema, biopsied. The animal continued to deteriorate and scaling and crusting. The dog was treated first was euthanized at the owner’s request. The with novalexin and then prednisone; he did well veterinarian obtained permission to perform a postmortem examination. The liver was diffusely nodular; the rest of the abdominal viscera were unremarkable. Samples of liver and skin were submitted for histopathology. Gross Pathology: Two punch skin biopsies (0.7 cm in greatest diameter) with ulcerated surfaces and two fragments of liver (3.5 cm and 2.5 cm in their largest dimension) were submitted for histopathology. The liver samples had a nodular, irregular, capsular surface. Laboratory Results: Parameter Value Reference Interval Albumin 23 G/L 24-55 1-1. Haired skin, dog: This section of skin is covered by a thick parakeratotic serocellular crust (extending down into hair follicles), ALP 1632 U/L 20-150 with marked acanthosis and hyperplasia of basal epithelium. (HE 0.63X) 1 WSC 2013-2014 ALT 442 U/L 10-118 Glucose 9.2 mmol/L 3.3-6.1 WBC 19.1 x 103/ 6.0-17.0 mm3 segmented 94% lymphocytes 3% monocytes 2% bands 1% RBC 4.12 x 106/ 5.50-8.50 mm3 urine glucose 3+ 1-2. -

A Multifaceted Examination of Cutaneous Disease Associated
A Multifaceted Examination of Cutaneous Disease Associated With Oncologic Conditions: Atypical Post- Radiation Vascular Proliferation, Cutaneous Neoplasms in Lynch Syndrome Patients, Non-Melanoma Skin Cancer in Children, and Case Studies of Rare Cutaneous Eruptions The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Zhong, Connie S. 2020. A Multifaceted Examination of Cutaneous Disease Associated With Oncologic Conditions: Atypical Post- Radiation Vascular Proliferation, Cutaneous Neoplasms in Lynch Syndrome Patients, Non-Melanoma Skin Cancer in Children, and Case Studies of Rare Cutaneous Eruptions. Doctoral dissertation, Harvard Medical School. Citable link https://nrs.harvard.edu/URN-3:HUL.INSTREPOS:37365212 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA ! ! ! ! ! "!#$%&'()*+&+,!-.)/'0)&'10!1(!2$&)0+1$3!4'3+)3+!"331*')&+,!5'&6!70*1%18'*! 210,'&'1039!"&:;'*)%!<13&=>),')&'10!?)3*$%)@!<@1%'(+@)&'10A!2$&)0+1$3! B+1;%)3/3!'0!C:0*6!D:0,@1/+!;)&'+0&3A!B10=#+%)01/)!DE'0!2)0*+@!'0!26'%,@+0A! )0,!2)3+!D&$,'+3!1(!>)@+!2$&)0+1$3!-@$;&'103F! ! ! ! ! ! ! ! ! ! ! ! G:! ! 2100'+!DF!H6108! ! ! D$G/'&&+,!'0!<)@&')%!I$%('%%/+0&!1(!&6+!>+J$'@+/+0&3!(1@!&6+!#F4F!4+8@++! 5'&6!K101@3!'0!)!D;+*')%!I'+%,!)&!K)@L)@,!#+,'*)%!D*611%! ! ! ! I+G@$)@:!MNA!ONON! Abstract A wide variety of skin conditions can arise in cancer patients, whether from cancer therapy, underlying genetic syndromes, paraneoplastic processes, or immunosuppression. -

Invisible Dermatoses
Invisible Dermatoses To our knowledge, Martin Brownstein and tle else besides a cornoid lamella. Multiple Asher Rabinowitz first used the term "invisi- sections must be searched to find this struc ble dermatoses."* Generations of dermatolo ture (p. 176). gists, however, have struggled with biopsy 3. Ichthyosis-Often the only clue to ich specimens from diseased skin that appear to be thyosis vulgaris is the absence of a granular normal under the microscope. Since normal layer that is associated with compact hy skin is rarely ever biopsied in clinical practice, perkeratosis. In the absence of hyperkera one must assume that some disease is present. tosis, this is an easy diagnosis to miss. Technical problems must be eliminated, such 4. Pigment changes-Vitiligo looks almost as sampling errors where normal skin on an normal, except that melanocytes are miss edge of the biopsy specimen has been sectioned ing (as is melanin). Conditions that have in and the diseased tissue has been left in paraf- creased melanin, but normal numbers of fin. It is wise to check again to see if the cli melanocytes (e.g., freckles and cafe au lait nician might have submitted normal skin (e.g., spots) may be mistaken for normal black pruritus, resolved urticaria, patient insisting skin. that normal spot is painful, and normal skin obtained for IF but submitted for H&E stain ing). At this point, one needs a strategy for studying skin that appears histologically nor Dermal Diseases mal, but must contain disease. We consider the following conditions: 1. Incontinence of pigment-Melanin in the papillary dermis may be the only clue to a der matitis that involved the epidermal-dermal Epidermal Diseases junction (e.g., lichen planus or lupus erythematosus ). -
The Interface Reaction Pattern in the Skin: an Integrated Review of Clinical and Pathological Features☆,☆☆ Maria A
Human Pathology (2019) 91,86–113 www.elsevier.com/locate/humpath Current topics The interface reaction pattern in the skin: an integrated review of clinical and pathological features☆,☆☆ Maria A. Deschaine MD a, Julia S. Lehman MD a,b,⁎ aDepartment of Dermatology, Mayo Clinic, Rochester, MN 55905 bDepartment of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN 55905 Received 9 May 2019; revised 18 June 2019; accepted 20 June 2019 Keywords: Summary Not uncommonly, pathologists encounter biopsies displaying inflammation at the dermoepi- Interface; dermal junction and confronted with its numerous diagnostic possibilities. As with other inflammatory Lichenoid; dermatoses, the correct diagnosis relies on careful integration of clinical, laboratory, and histopathologi- Vacuolar; cal features. Knowledge of clinical aspects of these disorders is crucial, and at times, lack of training Inflammatory dermatoses in clinical dermatology can make clinicopathological correlation challenging for the pathologist. This re- view is organized following the classical classification of cell-poor (vacuolar) and cell-rich (lichenoid) interface processes. The various entities are described based on their clinical presentation along their clinical differential diagnosis followed by their histopathological features and pathological differential diagnosis. Our aim is to provide an updated, clinically relevant review that integrates nuanced clinical and pathological features, with an emphasis on clues that may help differentiate entities in the differential -

Cutaneous Manifestations of Systemic Disease
Cutaneous Manifestations of Systemic Disease Dr. Lloyd J. Cleaver D.O. FAOCD Northeast Regional Medical Center A.T.Still University/KCOM Assistant Vice President/Professor ABOIM Board Review Disclosure I have no financial relationships to disclose I will not discuss off label use and/or investigational use in my presentation I do not have direct knowledge of AOBIM questions I have been granted approvial by the AOA to do this board review Dermatology on the AOBIM ”1-4%” of exam is Dermatology Table of Test Specifications is unavailable Review Syllabus for Internal Medicine Large amount of information Cutaneous Multisystem Cutaneous Connective Tissue Conditions Connective Tissue Diease Discoid Lupus Erythematosus Subacute Cutaneous LE Systemic Lupus Erythematosus Scleroderma CREST Syndrome Dermatomyositis Lupus Erythematosus Spectrum from cutaneous to severe systemic involvement Discoid LE (DLE) / Chronic Cutaneous Subacute Cutaneous LE (SCLE) Systemic LE (SLE) Cutaneous findings common in all forms Related to autoimmunity Discoid LE (Chronic Cutaneous LE) Primarily cutaneous Scaly, erythematous, atrophic plaques with sharp margins, telangiectasias and follicular plugging Possible elevated ESR, anemia or leukopenia Progression to SLE only 1-2% Heals with scarring, atrophy and dyspigmentation 5% ANA positive Discoid LE (Chronic Cutaneous LE) Scaly, atrophic plaques with defined margins Discoid LE (Chronic Cutaneous LE) Scaly, erythematous plaques with scarring, atrophy, dyspigmentation DISCOID LUPUS Subacute Cutaneous -

37 Histopathology of Irritant Contact Dermatitis
345 37 Histopathology of Irritant Contact Dermatitis Carolyn M. Willis Contents the skin [1], and with a histopathology largely indis- tinguishable from that of the majority of chronic in- 37.1 Introduction . 345 flammatory dermatoses. 37.2 Acute Irritant Contact Dermatitis . 346 When considering the histopathology of ICD, it is 37.2.1 Epidermal Features . 346 important to bear in mind that all of the following pa- 37.2.2 Dermal Features . 348 rameters will influence the histopathological changes 37.2.3 Leukocyte Infiltration . 349 observed under the light microscope: 37.3 Chronic Irritant Contact Dermatitis . 350 37.3.1 Epidermal Features . 350 37.3.2 Dermal Features . 350 1. Chemical nature and concentration of irritant References . 350 chemical In addition to the physicochemical properties of an irritant, which have a direct bearing on the nature of the cellular damage inflicted, concentration effects are also profound. At sufficiently high concentration, 37.1 Introduction many irritants will cause overt tissue necrosis. Lower concentrations produce more subtle changes, partic- Irritant contact dermatitis is a heterogeneous inflam- ularly in the epidermis. matory condition, both clinically and histopathologi- cally. Arising primarily from contact with chemicals, 2. Mode and duration of exposure the inflammation may be acute or chronic in nature, The circumstances of irritant exposure, such as single, depending upon the irritation potential of the sub- occlusive patch testing or repetitive open testing, and stance and the circumstances of exposure. Chemicals the length of time the chemical is in contact with the such as acids, alkalis, and detergents will, at high con- skin, will all influence the severity and nature of re- centration, cause sufficient damage to the skin to in- sponse, and hence the histological picture. -

1 Pathology Week X
Pathology week x – Skin ver. -
Current Concepts in Dermatology
CURRENT CONCEPTS IN DERMATOLOGY KARTHIK KRISHNAMURTHY, D.O., FAOCD ACTIVITY CHAIR Acknowledgement of Commercial Support 2017 American Osteopathic College of Dermatology Corporate Members Diamond Level Galderma • Pfizer Platinum Level Lilly USA, LLC Gold Level AbbVie • Valeant Pharmaceuticals Bronze Level Allergan • Dermpath Lab of Central States Pearl Level Aclaris Therapeutics • Dermpath Diagnostics • Novartis • Sun Dermatology Sponsors/Unrestricted Educational Grants Dermpath Lab of Central States • Lilly USA, LLC • Sagis Diagnostics • Valeant Pharmaceuticals Product Theater AbbVie • Lilly USA, LLC • Pfizer • Valeant Pharmaceuticals 2017 American Osteopathic College of Dermatology Spring Meeting Exhibitors 3Gen, Inc. DermTech Pfizer/Eucrisa AbbVie D-Path ProPath Services LLP Aclaris Therapeutics, Inc. Encore Dermatology Ra Medical Systems, Inc. Advanced Dermatology & Cosmetic Surgery Galderma Laboratories Sagis Diagnostics Allergan Heartland Payment Systems Sensus Healthcare Anne Arundel Dermatology Hill Dermaceuticals, Inc. Skin Path Solutions Aurora Diagnostics Janssen Biotech, Inc. Strata Skin Sciences Bayer Healthcare Leo Pharma Sun Dermatology Celgene Lilly USA, LLC Valeant Pharmaceuticals Dermpath Diagnostics Medimetriks Pharmaceuticals Dermpath Lab of Central States Novartis Continuing Medical Education Statements This activity will change your practice and improve patient outcomes! AOA Statement: The American Osteopathic College of Dermatology is accredited by the American Osteopathic Association to provide osteopathic continuing -
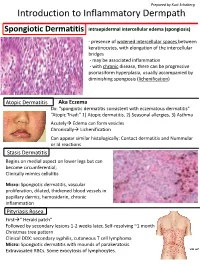
Introduction to Inflammatory Dermpath
Prepared by Kurt Schaberg Introduction to Inflammatory Dermpath Spongiotic Dermatitis intraepidermal intercellular edema (spongiosis) - presence of widened intercellular spaces between keratinocytes, with elongation of the intercellular bridges - may be associated inflammation - with chronic disease, there can be progressive psoriasiform hyperplasia, usually accompanied by diminishing spongiosis (lichenification) Atopic Dermatitis Aka Eczema Dx: “spongiotic dermatitis consistent with eczematous dermatitis” “Atopic Triad:” 1) Atopic dermatitis, 2) Seasonal allergies, 3) Asthma Acutely Edema can form vesicles Chronically Lichenification Can appear similar histologically: Contact dermatitis and Nummular or Id reactions Stasis Dermatitis Begins on medial aspect on lower legs but can become circumferential; Clinically mimics cellulitis Micro: Spongiotic dermatitis, vascular proliferation, dilated, thickened blood vessels in papillary dermis, hemosiderin, chronic inflammation Pityriasis Rosea First“ Herald patch” Followed by secondary lesions 1-2 weeks later, Self-resolving ~1 month Christmas tree pattern Clinical DDX: secondary syphilis, cutaneous T cell lymphoma Micro: Spongiotic dermatitis with mounds of parakeratosis. Extravasated RBCs. Some exocytosis of lymphocytes. Lichenoid Dermatitis Interface Dermatitis Band-like infiltrate that hugs the Basal keratinocyte hydropic change with dermoepidermal junction vacuolization and variable lymphocytic inflammation Lichen Planus Common entity, unknown etiology; Pruritic, purple, papules Micro: