Thrombocytopenia in Older Adults Melissa (Kah Poh) Loh, MD
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protein S Deficiency Presenting with Hemorrhage in a Term Neonate
: Curre re nt a R C e Ayari et al., Health Care Current Reviews 2018, 6:1 h v t i l e a w DOI: 10.4172/2375-4273.1000219 e s H Health Care: Current Reviews ISSN: 2375-4273 Review Article Open Access Protein S Deficiency Presenting with Hemorrhage in a Term Neonate Fairouz Ayari*, Takoua Bensmail, Essid Latifa, Wiem Barbaria and Samia Kacem Neonatology Intensive Care Unit of the Maternity and Neonatology Center, Tunis, Tunisia Abstract Unexplained bleeding symptoms in otherwise healthy full-term usually present a diagnostic challenge for treating physicians requiring prompt and accurate laboratory investigations to ensure appropriate treatment and possibly avoid long-term morbidity. We report a case of a term neonate with severe protein S deficiency manifested by systemic hemorrhage and multiple organ failure at 9 days of age. We review how protein S influences the coagulation and the fibrinolytic pathways, discussing therapeutic approaches of neonates with purpura fulminans. Keywords: Protein S deficiency; Blood sample; Thrombophilic dis- resuscitation with 20 ml/kg bodyweight (BW) saline solution and, after order blood sampling, intravenous administration of 10 mg vitamin K, 20 ml/kg BW fresh frozen plasma, 20 ml/kg BW packed red blood cells Introduction (5 transfusion cycles), 20 mg/kg BW Phenobarbital and vasoactive Protein S (PS) is an antithrombotic plasma protein that acts mainly drugs. Cerebral ultrasound revealed intraventricular haemorrhage, as a cofactor of activated protein C (APC) anticoagulant activity in the abdominal ultrasound showed splenic hemorrhage and cardiac degradation of factor Va and activated factor VIII [1]. PS circulates in ultrasound showed a floating intracardiac thrombus. -

Urticarial Vasculitis Associated with Essential Thrombocythaemia
Acta Derm Venereol 2014; 94: 244–245 SHORT COMMUNICATION Urticarial Vasculitis Associated with Essential Thrombocythaemia Annabel D. Scott, Nicholas Francis, Helen Yarranton and Sarita Singh Dermatology Registrar, Department of Dermatology, Chelsea and Westminster Hospital, 369 Fulham Road, London SW10 9NH, United Kingdom. E-mail: [email protected] Accepted Apr 3, 2013; Epub ahead of print Aug 27, 2013 Urticarial vasculitis is a form of leucocytoclastic vas- prednisolone 30 mg once daily, which controlled her culitis whereby the skin lesions resemble urticaria. It is symptoms. associated with systemic lupus erythematosus, Sjögren’s A biopsy was taken from an uticarial lesion on the syndrome, hepatitis B and C viruses (1). Rarely it is asso- arm. Histology showed numerous perivascular neutro- ciated with an underlying haematological disorders and, phils and eosinophils with margination of neutrophils to the best of our knowledge, has never been reported in in the lumen of vessels and some leucocytoclasis with association with essential thrombocythaemia. We present red cell extravasation in keeping with an urticarial a case report of urticarial vasculitis associated with es- vasculitis (Fig. 2). sential thrombocythaemia. Blood tests revealed an erythrocyte sedimentation rate of 47 mm/h (normal range 1–12), a platelet count of 1,098 × 109/l (normal range 135–400) and an eosi- CASE REPORT nophilia of 1.0 × 109/l (normal range 0–0.2). Comple- A 32-year-old woman presented with a several month ment levels, thyroid function, serum iron, haemoglobin, history of recurrent urticaria without angioedema, 4 C-reactive protein, anti-nuclear antibody, anti-nuclear months post-partum. -

Outcomes of Patients with Thrombocytopenia Evaluated at Hematology Subspecialty Clinics
Henry Ford Health System Henry Ford Health System Scholarly Commons Hematology Oncology Articles Hematology-Oncology 2-11-2021 Outcomes of patients with thrombocytopenia evaluated at hematology subspecialty clinics Zaid H. Abdel Rahman Kevin C. Miller H Jabbour Yaser Alkhatib Vijayalakshmi Donthireddy Follow this and additional works at: https://scholarlycommons.henryford.com/ hematologyoncology_articles Hematol Oncol Stem Cell Ther xxx (xxxx) xxx Available at www.sciencedirect.com ScienceDirect journal homepage: www.elsevier.com/locate/hemonc Outcomes of patients with thrombocytopenia evaluated at hematology subspecialty clinics Zaid H. Abdel Rahman a,*, Kevin C. Miller b, Hiba Jabbour c, Yaser Alkhatib c, Vijaya Donthireddy c a Division of Hematology and Medical Oncology, Mayo Clinic, Jacksonville, FL, USA b Department of Medicine, Massachusetts General Hospital, Boston, MA, USA c Division of Hematology and Medical Oncology, Henry Ford Hospital, Detroit, MI, USA Received 6 October 2020; received in revised form 9 December 2020; accepted 15 January 2021 KEYWORDS Abstract Hematology; Background: Thrombocytopenia is a frequently encountered laboratory abnormality and a Malignancy; common reason for hematology referrals. Workup for thrombocytopenia is not standardized Platelets; and frequently does not follow an evidence-based algorithm. We conducted a systematic anal- Referrals; Thrombocytopenia ysis to evaluate the laboratory testing and outcomes of patients evaluated for thrombocytope- nia at hematology clinics in a tertiary referral center between 2013 and 2016. Patient and methods: We performed a comprehensive chart review for patients evaluated for thrombocytopenia during the study period. Patients were followed for 1 year from the initial hematology evaluation and assessed for the development of a hematologic malignancy, rheumatologic, or infectious diseases among other clinical outcomes. -

Important Information for Female Platelet Donors
Important Information for Female Platelet Donors We are grateful for the support you provide our community blood program and especially appreciate your willingness to help save lives as a volunteer platelet donor. We also take our responsibility to provide a safe and adequate blood supply very seriously and need to share the following information regarding a change to our donor eligibility criteria for female platelet donors. We recently began performing a Human Leukocyte Antigen (HLA) antibody test on each of our current female platelet donors who have ever been pregnant. In addition, we modified our Medical History Questionnaire to ask donors whether they have been pregnant since their last donation. Platelet donors who respond yes to that question will be screened for HLA antibodies. Platelet donors will also be retested after every subsequent pregnancy. These adjustments are being made as part of our effort to reduce occurrences of Transfusion-Related Acute Lung Injury (TRALI). TRALI is a rare but serious complication of blood transfusions most commonly thought to be caused by a reaction to HLA antibodies present in the donor’s plasma. When transfused, these antibodies can sometimes cause plasma to leak into the patient’s lungs, creating fluid accumulation — a condition referred to as acute pulmonary edema. Female donors who have been pregnant are more likely than others to have these HLA antibodies in their plasma. Once the antibodies develop, they are present forever. The antibodies could be harmful if transfused into certain patients. The antibodies are present in plasma — and platelet donations contain a high volume of plasma, so our current efforts are directed at screening blood samples from female platelet donors to test for the HLA antibody. -

Severe Fever with Thrombocytopenia Syndrome: a Newly Discovered Emerging Infectious Disease
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector REVIEW Severe fever with thrombocytopenia syndrome: a newly discovered emerging infectious disease D. X. Li Key Laboratory for Medical Virology, National Institute for Viral Disease Control and Prevention, China CDC, Beijing, China Abstract Severe fever with thrombocytopenia syndrome (SFTS) is a newly discovered emerging infectious disease that has recently become epidemic in Asia. The causative agent of SFTS is a novel phlebovirus in the family Bunyaviridae, designated SFTS virus (SFTSV). SFTS clinically presents with high fever, thrombocytopenia, leukocytopenia, gastrointestinal disorders, and multi-organ dysfunction, with a high viral load and a high case- fatality rate. In human infection, SFTSV targets microphages, replicates in the spleen of infected mice, and causes thrombocytopenia and a cytokine storm. The tick disseminates virus to humans and animals, forming a special transmission model in nature. Person-to-person transmission though direct contact with patient blood has been frequently reported. Measurements of viral RNA and antibodies have been established for diagnosis, but vaccines and specific therapeutics are not available so far. Clinical Microbiology and Infection © 2015 European Society of Clinical Microbiology and Infectious Diseases. Published by Elsevier Ltd. All rights reserved. Keywords: Clinical, epidemiology, SFTS virus, SFTS, virology Article published online: 11 March 2015 Virology D.X. Li, Key Laboratory for Medical Virology, NCHFP, RRC, National Institute for Viral Disease Control and Prevention, China CDC, Bei- jing 102206, China E-mail: [email protected] The causative agent of SFTS is SFTSV, which is a tick-borne virus in the family Bunyaviridae, genus Phlebovirus. -

CD59: a Long-Known Complement Inhibitor Has Advanced to a Blood Group System
B LOOD G ROUP R EVIEW CD59: A long-known complement inhibitor has advanced to a blood group system C. Weinstock, M. Anliker, and I. von Zabern The blood group system number 35 is based on CD59, a 20-kDa by Zalman et al.1 from the group of H.J. Muller-Eberhard in La membrane glycoprotein present on a large number of different Jolla, California, and in 1988 by Schönermark et al. from the cells, including erythrocytes. The major function of CD59 is to group of G.M. Hänsch in Heidelberg (Germany).2 This inhibitor protect cells from complement attack. CD59 binds to complement components C8 and C9 and prevents the polymerization of C9, was published under the designations “HRF (homologous which is required for the formation of the membrane attack restriction factor)” and “C8bp (C8 binding protein),” complex (MAC). Other functions of CD59 in cellular immunity respectively, to describe its properties.1,2 “C8bp” indicates the are less well defined. CD59 is inserted into the membrane by a glycosylphosphatidylinositol (GPI) anchor. A defect of this anchor binding capacity for C8. The name “HRF” points to a species causes lack of this protein from the cell membrane, which leads to incompatibility of this “factor” that provides protection from an enhanced sensitivity towards complement attack. Patients with complement attack more effectively in a homologous (e.g., paroxysmal nocturnal hemoglobinuria (PNH) harbor a varying human erythrocytes as a target of human complement) than in percentage of red blood cell clones with a defect in GPI-anchored proteins, including CD59. The most characteristic symptoms of a heterologous system (e.g., human erythrocytes as a target of this disease are episodes of hemolysis and thromboses. -

Neonatal Leukopenia and Thrombocytopenia
Neonatal Leukopenia and Thrombocytopenia Vandy Black, M.D., M.Sc., FAAP March 3, 2016 April 14, 2011 Objecves • Summarize the differenHal diagnosis of leukopenia and/or thrombocytopenia in a neonate • Describe the iniHal steps in the evaluaon of a neonate with leukopenia and/or thrombocytopenia • Review treatment opHons for leukopenia and/ or thrombocytopenia in the NICU Clinical Case 1 • One day old male infant admiUed to the NICU for hypoglycemia and a sepsis rule out • Born at 38 weeks EGA by SVD • Birth weight 4 lbs 13 oz • Exam shows a small cephalohematoma; no dysmorphic features • PLT count 42K with an otherwise normal CBC Definions • Normal WBC count 9-30K at birth – Mean 18K • What is the ANC and ALC – <1000/mm3 is abnormal – 6-8% of infants in the NICU • Normal platelet count: 150-450,000/mm3 – Not age dependent – 22-35% of infants in the NICU have plts<150K Neutropenia Absolute neutrophil count <1500/mm3 Category ANC* InfecHon risk • Mild 1000-1500 None • Moderate 500-1000 Minimal • Severe <500 Moderate to Severe (Highest if <200) • Recurrent bacterial or fungal infecHons are the hallmark of symptomac neutropenia! • *ANC = WBC X % (PMNs + Bands) / 100 DefiniHon of Neutropenia Black and Maheshwari, Neoreviews 2009 How to Approach Cytopenias • Normal vs. abnormal (consider severity) • Malignant vs. non-malignant • Congenital vs. acquired • Is the paent symptomac • Transient, recurrent, cyclic, or persistent How to Approach Cytopenias • Adequate vs. decreased marrow reserve • Decreased producHon vs. increased destrucHon/sequestraon Decreased neutrophil/platelet producon • Primary – Malignancy/leukemia/marrow infiltraon – AplasHc anemia – Genec disorders • Secondary – InfecHous – Drug-induced – NutriHonal • B12, folate, copper Increased destrucHon/sequestraon • Immune-mediated • Drug-induced • Consumpon à Hypersplenism vs. -

Essential Thrombocythemia Facts No
Essential Thrombocythemia Facts No. 12 in a series providing the latest information for patients, caregivers and healthcare professionals www.LLS.org • Information Specialist: 800.955.4572 Introduction Highlights Essential thrombocythemia (ET) is one of several l Essential thrombocythemia (ET) is one of a related “myeloproliferative neoplasms” (MPNs), a group of closely group of blood cancers known as “myeloproliferative related blood cancers that share several features, notably the neoplasms” (MPNs) in which cells in the bone “clonal” overproduction of one or more blood cell lines. marrow that produce the blood cells develop and All clonal disorders begin with one or more changes function abnormally. (mutations) to the DNA in a single cell; the altered cells in l ET begins with one or more acquired changes the marrow and the blood are the offspring of that one (mutations) to the DNA of a single blood-forming mutant cell. Other MPNs include polycythemia vera and cell. This results in the overproduction of blood cells, myelofibrosis. especially platelets, in the bone marrow. The effects of ET result from uncontrolled blood cell l About half of individuals with ET have a mutation production, notably of platelets. Because the disease arises of the JAK2 (Janus kinase 2) gene. The role that this from a change to an early blood-forming cell that has the mutation plays in the development of the disease, capacity to form red cells, white cells and platelets, any and the potential implications for new treatments, combination of these three cell lines may be affected – and are being investigated. usually each cell line is affected to some degree. -

Appendix Search Strategy Treatment of Hemophilia.Pdf
Appendix Search strategies Hemophilia – general aspects PubMed (NLM) September 2009 Von Willebrand disease (TiAb) AND Controlled clinical trial (PT) NOT Purpura, Thrombocytopenic (Me) Angiohemophilia (TiAb) Meta analysis (PT) Blood coagulation disorders (Me) Randomized controlled trial (PT) Hemophilia (TiAb) Systematic (SB) Haemophilia (TiAb) Bleeding disorder (TiAb) Random* (Ti) Bleeding disorders (TiAb) OR Control* (Ti) NOT Medline (SB) ("controlled clinical trial"[Publication Type] OR "meta analysis"[Publication Type] OR "randomized controlled trial"[Publication Type] OR systematic[sb] OR ((random*[Title] OR control*[Title]) NOT Medline[sb])) AND ("von Willebrand Disease"[title/abstract] OR "angiohemophilia"[title/Abstract] OR "Blood Coagulation Disorders"[Mesh terms] OR "hemophilia"[title/abstract] OR "haemophilia"[title/abstract] OR "bleeding disorder"[title/abstract] OR "bleeding disorders"[Title/abstract]) NOT "Purpura, Thrombocytopenic"[MeSH Terms] 211 Hemophilia – general aspects Embase.com (Elsevier) September 2009 Blood clotting factor deficiency (Exp,MJR) AND Clinical trial (Exp) NOT Thrombocytopenic purpura (Exp) Von Willebrand disease (Ti) Intervention study (De) Angiohemophilia (Ti) Longitudinal study (De) Angiohaemophilia (Ti) Prospective study (De) Hemophilia (Ti) Meta analysis (De) Haemophilia (Ti) Systematic review (De) Bleeding disorder (Ti) Random* (Ti) Bleeding disorders (Ti) Control* (Ti) ('blood clotting factor deficiency'/exp/mjOR 'von willebrand disease':ti OR 'angiohemophilia':ti OR 'angiohaemophilia':ti OR 'hemophilia':ti -
Immune Thrombocytopenic Purpura with Subsequent Development of JAK2 V617F-Positive Essential Thrombocythemia: Case Report
ISSN: 2640-7914 DOI: https://dx.doi.org/10.17352/ahcrr CLINICAL GROUP Received: 13 July, 2021 Case Report Accepted: 03 August, 2021 Published: 04 August, 2021 *Corresponding author: Marisabel Hurtado-Castillo, Immune thrombocytopenic PGY-3, Internal Medicine, Department of Medicine at NYU, 536 Ovington Avenue Apartment 3, Brooklyn NYC 11209, USA, Tel: 718-312-9641; purpura with subsequent Email: Keywords: Immune thrombocytopenic purpura; development of JAK2 Essential thrombocythemia; JAK-STAT signaling path- way; JAK2(V617F) mutation V617F-positive essential https://www.peertechzpublications.com thrombocythemia: Case Report Marisabel Hurtado-Castillo1*, Brian Flaherty2 and Morris Jrada2 1PGY-3, Internal Medicine, Department of Medicine at NYU, Brooklyn, NY, USA 2Clinical Assistant Professor, Department of Medicine at NYU Grossman School of Medicine, Brooklyn, NY, USA Abstract The sequential occurrence of Immune Thrombocytopenic Purpura (ITP) and Essential Thrombocythemia (ET) has been reported in the literature on a few occasions, as these are two hematologic disorders with distinct etiologies and patients usually have contrasting clinical presentations. Our case highlights the sequential occurrence of ITP, followed by Janus kinase 2 (JAK2) (V617F)-positive ET in a 64-year-old white woman, after four years of follow-up. The pathophysiology relating to these two conditions is incompletely understood, however, JAK2(V617F) mutation has been found in all the cases reported. Early identifi cation of JAK2(V617F) mutation in a patient with a -
Thrombocytopenia.Pdf
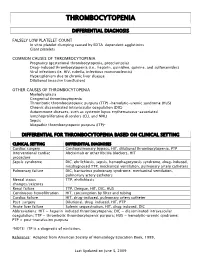
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -
Canine and Feline Coagulopathies Office News Michelle Fulks, DVM, Virginia Sinnott, DVM, DACVECC William B
Monthly Update August 2013 Issue Contributors: Michelle Fulks, DVM, Virginia Sinnott, DVM, DACVECC, William B. Henry DVM, DACVS Editor: William B. Henry DVM, DACVS Canine and Feline Coagulopathies Office News Michelle Fulks, DVM, Virginia Sinnott, DVM, DACVECC William B. Henry, Jr. DVM, DACVS Canine and Feline Coagulopathies Bleeding disorders are considered a potential life-threatening emergency in small animal practice. It is crucial to recognize the potential for a coagulation disorder through history and physical exam findings, pursue appropriate diagnostic tests and then treat appropriately in order to prevent massive bleeding in these patients. Three areas of the hemostatic system may be affected to cause coagulopathies: Amanda Spencer, CVT joined our surgery team in late 2012. She has 10 1. Disorders of Primary Hemostasis years experience in surgery and 2. Disorders of Secondary Hemostasis emergency care. Her sole focus at BVS 3. Disorders of Fibrinolysis is with the surgical practice. Her skills, dedication to excellence, and caring Primary hemostasis is the formation of the initial platelet plug. Decreases in attitude towards our clients and platelet number, platelet function, or reduced von Willebrand factor (VWF) can all patients, has been outstanding. Her cause disorders of primary hemostasis and lead to mucosal bleeding or calm upbeat personality makes our bruising. Secondary hemostasis is the formation of a stable fibrin clot via cascade days together as a team more of enzymes that ultimately convert fibrinogen to fibrin. Defects in coagulation enjoyable. She is one of those staff factors can lead to severe bleeding diatheses. Fibrinolysis is the breakdown of the members "behind the public eye" who fibrin clot by plasmin.