Immune Thrombocytopenic Purpura with Subsequent Development of JAK2 V617F-Positive Essential Thrombocythemia: Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Impact of Thrombophilia in the Management Of
S6 MPN III – Abstracts of the 8th International Hematology Expert Meeting / Leukemia Research 44 S1 (2016) S1–S12 Figure 1. Possible new treatment algorithm in polycythemia vera and essential thrombocythemia (CVR = cardiovascular risk factors). Adapted from: Tefferi A, Barbui T. Am J Hematol 2015;90(8):683–5 MPN III the Czech part of the international registry (“Registry”) of anagrelide (Thromboreductin®)-treated patients. The impact of thrombophilia in the management of MPN The recent analysis of the “Registry” [6] included altogether 1179 patients having MPD-T – either ET, PV or PMF according to PVSG criteria. In 812 J. Schwarz patients, the WHO/CZEMP diagnosis could be established: ET – 445 CZEMP (Czech Group for Ph– Myeloproliferative Disorders), Prague, Czech (54.8%), PMF – 206 (25.4%), PV – 107 (13.2%), and other (mostly MPN- Republic unclassifiable) – 54 (6.7%) cases. The M/F ratio was 2:3, the median age of The overall thrombotic risk in a normal healthy population is always based patients was 52 years (6–91 years) at diagnosis. The incidence of vascular on a combination of multiple risk factors present in one individual. The events was compared in the history (before entering the Registry) and risk parameters for arterial and venous events differ. MPD-T represents during follow-up (on anagrelide treatment). History and follow-up a situation in which the specific MPD-related risks (such as the JAK2 represented 4149 and 4742 patient-years, respectively. For arterial events, mutation) are combined with other risk factors present in the general there was a decrease in the incidence of events from 5.04 to 2.74 per 100 population. -

Urticarial Vasculitis Associated with Essential Thrombocythaemia
Acta Derm Venereol 2014; 94: 244–245 SHORT COMMUNICATION Urticarial Vasculitis Associated with Essential Thrombocythaemia Annabel D. Scott, Nicholas Francis, Helen Yarranton and Sarita Singh Dermatology Registrar, Department of Dermatology, Chelsea and Westminster Hospital, 369 Fulham Road, London SW10 9NH, United Kingdom. E-mail: [email protected] Accepted Apr 3, 2013; Epub ahead of print Aug 27, 2013 Urticarial vasculitis is a form of leucocytoclastic vas- prednisolone 30 mg once daily, which controlled her culitis whereby the skin lesions resemble urticaria. It is symptoms. associated with systemic lupus erythematosus, Sjögren’s A biopsy was taken from an uticarial lesion on the syndrome, hepatitis B and C viruses (1). Rarely it is asso- arm. Histology showed numerous perivascular neutro- ciated with an underlying haematological disorders and, phils and eosinophils with margination of neutrophils to the best of our knowledge, has never been reported in in the lumen of vessels and some leucocytoclasis with association with essential thrombocythaemia. We present red cell extravasation in keeping with an urticarial a case report of urticarial vasculitis associated with es- vasculitis (Fig. 2). sential thrombocythaemia. Blood tests revealed an erythrocyte sedimentation rate of 47 mm/h (normal range 1–12), a platelet count of 1,098 × 109/l (normal range 135–400) and an eosi- CASE REPORT nophilia of 1.0 × 109/l (normal range 0–0.2). Comple- A 32-year-old woman presented with a several month ment levels, thyroid function, serum iron, haemoglobin, history of recurrent urticaria without angioedema, 4 C-reactive protein, anti-nuclear antibody, anti-nuclear months post-partum. -

Immune Thrombocytopenia and JAK2V617F Positive Essential Thrombocythemia: Literature Review and Case Report
Hindawi Case Reports in Hematology Volume 2017, Article ID 3725089, 4 pages https://doi.org/10.1155/2017/3725089 Case Report Immune Thrombocytopenia and JAK2V617F Positive Essential Thrombocythemia: Literature Review and Case Report M. A. Sobas,1 T. Wróbel,1 K. Zduniak,2 M. Podolak-Dawidziak,1 J. Rybka,1 M. BiedroN,1 M. Sawicki,1 J. Dybko,1 and K. Kuliczkowski1 1 Department of Haematology, Blood Neoplasms and Bone Marrow Transplantation, Medical University of Wrocław, Wrocław, Poland 2Department of Pathology, Medical University of Wrocław, Wrocław, Poland Correspondence should be addressed to M. A. Sobas; [email protected] Received 27 March 2017; Revised 28 May 2017; Accepted 27 June 2017; Published 20 July 2017 Academic Editor: Eduardo Arellano-Rodrigo Copyright © 2017 M. A. Sobas et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We present the case where immune thrombocytopenia (ITP) and essential thrombocythemia (ET) sequentially appeared in the space of twenty-one years of follow-up. Impaired platelet production is present in both diseases, but clinical presentation and treatment are different. On the basis of this case history a possible role of autoimmunity as a predisposing factorto myeloproliferation has been discussed. 1. Introduction but proved one with myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML) [6]. Primaryimmunethrombocytopeniapreviouslycalledidio- pathic thrombocytopenic purpura or immune thrombocy- Here we present a case report of a patient with ITP who topenic purpura (ITP) is characterized by autoimmune- was diagnosed with ET, after 21 years of follow-up. -

Essential Thrombocythemia Effective Date: July, 2021
Guideline Resource Unit [email protected] Essential Thrombocythemia Effective Date: July, 2021 Clinical Practice Guideline LYHE-012 – Version 1 www.ahs.ca/guru Background Thrombocytosis, defined as a platelet count of ≥ 450 x 109/L, is common in clinical practice and can be related to primary or secondary causes. Essential thrombocythemia (ET), a primary cause, is a Philadelphia-negative classical myeloproliferative neoplasm (MPN) defined by clonal thrombocytosis1. Similar to other classical MPNs, mutually exclusive driver mutations including JAK2, CALR and MPL are responsible for the pathogenesis of ET with the most frequent mutation JAK2V617F found in 55% of ET, 15-30% having CALR and 4-8% having MPL, while 10-20% lack a driver mutation and are referred to as “triple negative”2. ET is complicated by thrombosis and bleeding risk with potential of transformation to myelofibrosis or alternative aggressive myeloid neoplasm. This guideline is to provide information regarding the diagnosis and management of ET based on our current standards. Guideline Questions 1. What diagnostic and baseline investigations are recommended for adult patients with suspected or confirmed ET? 2. What are the recommended treatment options for ET? 3. How do you manage extreme thrombocytosis? 4. How do you treat thrombosis in the setting of ET and other MPNs? 5. What is the current peri-operative and peripartum management strategies for ET/MPN patients? Search Strategy This guideline was generated using systematic literature searches of PubMed and MEDLINE databases, ASCO, EHA abstracts and proceedings, and ASH abstracts and proceedings. The search included practice guidelines, systematic reviews, meta-analyses, randomized controlled trials and clinical trials. -

Essential Thrombocythemia Facts No
Essential Thrombocythemia Facts No. 12 in a series providing the latest information for patients, caregivers and healthcare professionals www.LLS.org • Information Specialist: 800.955.4572 Introduction Highlights Essential thrombocythemia (ET) is one of several l Essential thrombocythemia (ET) is one of a related “myeloproliferative neoplasms” (MPNs), a group of closely group of blood cancers known as “myeloproliferative related blood cancers that share several features, notably the neoplasms” (MPNs) in which cells in the bone “clonal” overproduction of one or more blood cell lines. marrow that produce the blood cells develop and All clonal disorders begin with one or more changes function abnormally. (mutations) to the DNA in a single cell; the altered cells in l ET begins with one or more acquired changes the marrow and the blood are the offspring of that one (mutations) to the DNA of a single blood-forming mutant cell. Other MPNs include polycythemia vera and cell. This results in the overproduction of blood cells, myelofibrosis. especially platelets, in the bone marrow. The effects of ET result from uncontrolled blood cell l About half of individuals with ET have a mutation production, notably of platelets. Because the disease arises of the JAK2 (Janus kinase 2) gene. The role that this from a change to an early blood-forming cell that has the mutation plays in the development of the disease, capacity to form red cells, white cells and platelets, any and the potential implications for new treatments, combination of these three cell lines may be affected – and are being investigated. usually each cell line is affected to some degree. -

Appendix Search Strategy Treatment of Hemophilia.Pdf
Appendix Search strategies Hemophilia – general aspects PubMed (NLM) September 2009 Von Willebrand disease (TiAb) AND Controlled clinical trial (PT) NOT Purpura, Thrombocytopenic (Me) Angiohemophilia (TiAb) Meta analysis (PT) Blood coagulation disorders (Me) Randomized controlled trial (PT) Hemophilia (TiAb) Systematic (SB) Haemophilia (TiAb) Bleeding disorder (TiAb) Random* (Ti) Bleeding disorders (TiAb) OR Control* (Ti) NOT Medline (SB) ("controlled clinical trial"[Publication Type] OR "meta analysis"[Publication Type] OR "randomized controlled trial"[Publication Type] OR systematic[sb] OR ((random*[Title] OR control*[Title]) NOT Medline[sb])) AND ("von Willebrand Disease"[title/abstract] OR "angiohemophilia"[title/Abstract] OR "Blood Coagulation Disorders"[Mesh terms] OR "hemophilia"[title/abstract] OR "haemophilia"[title/abstract] OR "bleeding disorder"[title/abstract] OR "bleeding disorders"[Title/abstract]) NOT "Purpura, Thrombocytopenic"[MeSH Terms] 211 Hemophilia – general aspects Embase.com (Elsevier) September 2009 Blood clotting factor deficiency (Exp,MJR) AND Clinical trial (Exp) NOT Thrombocytopenic purpura (Exp) Von Willebrand disease (Ti) Intervention study (De) Angiohemophilia (Ti) Longitudinal study (De) Angiohaemophilia (Ti) Prospective study (De) Hemophilia (Ti) Meta analysis (De) Haemophilia (Ti) Systematic review (De) Bleeding disorder (Ti) Random* (Ti) Bleeding disorders (Ti) Control* (Ti) ('blood clotting factor deficiency'/exp/mjOR 'von willebrand disease':ti OR 'angiohemophilia':ti OR 'angiohaemophilia':ti OR 'hemophilia':ti -
Thrombocytopenia.Pdf
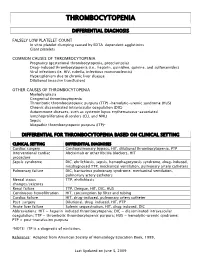
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -

Erythromelalgic Microvascular Disturbances, Major Thrombosis
& Throm gy b o o l e o t m Journal of Hematology & a b o m l e i c H D f o i s l e a Thromboembolic Diseases ISSN: 2329-8790 a Michiels, J Hematol Thromb Dis 2014, 2:5 n s r e u s o J DOI: 10.4172/2329-8790.1000149 Review Article Open Access Erythromelalgic Microvascular Disturbances, Major Thrombosis and Hemorrhagic Manifestations of Thrombocythemia in Patients with Essential Thrombocythemia and Polycythemia Vera: Therapeutic Implications Jan Jacques Michiels* Academic Hospital Dijkzigt, Erasmus University Rotterdam (EUR 1974-1998), Department of Hematology, Antwerp University Hospital, Belgium, and Goodheart Institute, Bloodcoagulation and Vascular Medicine Center, Rotterdam, (1998-2014) The Netherlands Abstract Aspirin responsive erythromelalgia is the presenting symptom of thrombocythemia in patients with essential thrombocythemia (ET) and polycythemia vera (PV). Skin punch biopsies taken from the affected areas of erythromelalgia and acrocyanotic compications show typical arteriolar inflammation, fibromuscular intimal proliferation and thrombotic occlusions. If left untreated both microvascular and major thrombosis frequently do occur in thrombocythemia in ET and PV patients, but can easily be cured and prevented by low dose aspirin. The stratification as low, intermediate and high thrombotic risk in the retrospective Bergamo studies has been performed in ET patients not treated with aspirin. The risk of thrombosis in aspirin treated ET and PV is not age dependent when on low dose aspirin, and does recur when not on low dose aspirin during follow-up. The persistence of the Bergamo definition of low, intermediate and high thrombotic risk in the 2012 International Prognostic Score of Thrombosis in ET (IPSET) is applicable for JAK2 mutated ET and PV patients not on aspirin and has led to significant overtreatment with hydroxyurea. -

Acute Immune Thrombocytopenic Purpura in Children
Turk J Hematol 2007; 24:41-51 REVIEW ARTICLE © Turkish Society of Hematology Acute immune thrombocytopenic purpura in children Abdul Rehman Sadiq Public School, Bahawalpur, Pakistan [email protected] Received: Sep 12, 2006 • Accepted: Mar 21, 2007 ABSTRACT Immune thrombocytopenic purpura (ITP) in children is usually a benign and self-limiting disorder. It may follow a viral infection or immunization and is caused by an inappropriate response of the immune system. The diagnosis relies on the exclusion of other causes of thrombocytopenia. This paper discusses the differential diagnoses and investigations, especially the importance of bone marrow aspiration. The course of the disease and incidence of intracranial hemorrhage are also discussed. There is substantial discrepancy between published guidelines and between clinicians who like to over-treat. The treatment of the disease ranges from observation to drugs like intrave- nous immunoglobulin, steroids and anti-D to splenectomy. The different modes of treatment are evaluated. The best treatment seems to be observation except in severe cases. Key Words: Thrombocytopenic purpura, bone marrow aspiration, Intravenous immunoglobulin therapy, steroids, anti-D immunoglobulins 41 Rehman A INTRODUCTION There is evidence that enhanced T-helper cell/ Immune thrombocytopenic purpura (ITP) in APC interactions in patients with ITP may play an children is usually a self-limiting disorder. The integral role in IgG antiplatelet autoantibody pro- American Society of Hematology (ASH) in 1996 duction -

Painless Purple Streaks on the Arms and Chest
PHOTO CHALLENGE Painless Purple Streaks on the Arms and Chest Tiffany Alexander, MD; Bernard Cohen, MD A 10-year-old boy presented with painless purple streaks on the arms and chest of 2 months’ duration. The rash recurred several times per month and cleared without treatment in 3 to 5 days. There was no history of trauma or medication exposure, and he was growing and developing normally.copy WHAT’S THE DIAGNOSIS? a. child maltreatment syndrome b. notfactitial purpura c. Henoch-Schönlein purpura d. idiopathic thrombocytopenic purpura Doe. meningococcemia PLEASE TURN TO PAGE E9 FOR THE DIAGNOSIS CUTIS Dr. Alexander was from the University of Maryland, Baltimore, and currently is from the Department of Dermatology, Duke University Medical Center, Durham, North Carolina. Dr. Cohen is from the Department of Dermatology, Division of Pediatric Dermatology, Johns Hopkins University School of Medicine, Baltimore. The authors report no conflict of interest. Correspondence: Bernard Cohen, MD, Johns Hopkins University School of Medicine, Division of Pediatric Dermatology, David M. Rubenstein Child Health Bldg, Ste 2107, 200 N Wolfe St, Baltimore, MD 21287 ([email protected]). E8 I CUTIS® WWW.MDEDGE.COM/DERMATOLOGY Copyright Cutis 2019. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: Factitial Purpura actitial dermatologic disorders are characterized by the state of one’s health and life span.4 Cupping is per- skin findings triggered by deliberate manipulation formed by placing a glass cup over a painful body part. F of the skin with objects to create lesions and feign A partial vacuum is created by flaming, mechanical with- signs of a dermatologic condition to seek emotional drawal, or thermal cooling of the entrapped air under the and psychological benefit.1 The etiology of the lesions is cup. -

Immune Thrombocytopenic Purpura (ITP) — Adult Conditions for Which Ivig Has an Established Therapeutic Role
Immune thrombocytopenic purpura (ITP) — adult Conditions for which IVIg has an established therapeutic role. Specific Conditions Newly Diagnosed Immune thrombocytopenic purpura (ITP) Persistent Immune thrombocytopenic purpura (ITP) Chronic Immune thrombocytopenic purpura (ITP) Evans syndrome ‐ with significant Immune thrombocytopenic purpura (ITP) ‐ adult Indication for IVIg Use Newly diagnosed ITP — initial Ig therapy ITP in pregnancy — initial Ig therapy ITP with life‐threatening haemorrhage or the potential for life‐threatening haemorrhage Newly diagnosed or persistent ITP — subsequent therapy (diagnosis <12 months) Refractory persistent or chronic ITP — splenectomy failed or contraindicated and second‐line agent unsuccessful Subsequent or ongoing treatment for ITP responders during pregnancy and the postpartum period ITP and inadequate platelet count for planned surgery HIV‐associated ITP Level of Evidence Evidence of probable benefit – more research needed (Category 2a) Description and Diagnostic Immune thrombocytopenic purpura (ITP) is a reduction in platelet count Criteria (thrombocytopenia) resulting from shortened platelet survival due to anti‐platelet antibodies, reduced platelet production due to immune induced reduced megakaryopoeisis and/or immune mediated direct platelet lysis. When counts are very low (less than 30x109/L), bleeding into the skin (purpura) and mucous membranes can occur. Bone marrow platelet production (megakaryopoiesis) is morphologically normal. In some cases, there is additional impairment of platelet function related to antibody binding to glycoproteins on the platelet surface. It is a common finding in patients with human immunodeficiency virus (HIV) disease, and while it may be found at any stage of the infection, its prevalence increases as HIV disease advances. Around 80 percent of adults with ITP have the chronic form of disease. -

Thrombocytopenia in Older Adults Melissa (Kah Poh) Loh, MD
URMC Division of Geriatrics & Aging March 2019 Thrombocytopenia in Older adults Melissa (Kah Poh) Loh, MD Background Thrombocytopenia (or low platelet count) is a common hematologic abnormality encountered in older adults Common causes of thrombocytopenia include (Table 1): Immune-related [e.g. immune thrombocytopenia purpura (ITP)] Drug-induced [e.g. heparin-induced thrombocytopenia (HIT)] Bone marrow failure Other: Infections (e.g. H. pylori, HIV, hepatitis), pseudothrombocytopenia (Figure 1), alcohol abuse, liver Figure 1: Peripheral smear showing clumped cirrhosis, blood transfusion, thrombotic thrombocytopenia platelets (pseudothrombocytopenia — falsely purpura (TTP), and hemolytic-uremic syndrome (HUS), low platelet count) thyroid disease Age-related changes in the organ and vasculature systems increase the risks of thrombocytopenia on hemostasis Factors that may enhance bleeding in older adults. These include: Comorbidities Medications Loss of subcutaneous tissue Age-specific factors that may prevent bleeding in older adults include enhanced platelet aggregation and increased fibrinogen, factor V, and von Willebrand factor Thrombocytopenia is often multifactorial in older adults. Table 1: Quick Facts on Thrombocytopenia PATHOPHYSIOLOGY Immune Thrombocytopenia Purpura Drug-Induced Increased platelet clearance in the reticulo-endothelial Impaired production (direct marrow toxicity or system of bone marrow, spleen, and/or liver megakaryocyte-specific inhibition) Inadequate platelet production due to megakaryocyte Increased platelet clearance (indirect immune clearance, inhibition by IgG antibodies antibody-specific immune clearance, miscellaneous immune -mediated) Often suppress other cell lines CAUSES Immune Thrombocytopenia Purpura Drug-Induced Often idiopathic See Table 2 Can be associated with underlying hematologic abnormalities (e.g. myelodysplastic syndrome, chronic lymphocytic leukemia) INCIDENCE RATES Immune Thrombocytopenia Purpura Drug-Induced 4.62 per 100,000 adults aged >60 years vs.