Sunburn Purpura
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Is Acne? Acne Is a Disease of the Skin's Sebaceous Glands
What is Acne? Acne is a disease of the skin’s sebaceous glands. Sebaceous glands produce oils that carry dead skin cells to the surface of the skin through follicles. When a follicle becomes clogged, the gland becomes inflamed and infected, producing a pimple. Who Gets Acne? Acne is the most common skin disease. It is most prevalent in teenagers and young adults. However, some people in their forties and fifties still get acne. What Causes Acne? There are many factors that play a role in the development of acne. Some of these include hormones, heredity, oil based cosmetics, topical steroids, and oral medications (corticosteroids, lithium, iodides, some antiepileptics). Some endocrine disorders may also predispose patients to developing acne. Skin Care Tips: Clean skin gently using a mild cleanser at least twice a day and after exercising. Scrubbing the skin can aggravate acne, making it worse. Try not to touch your skin. Squeezing or picking pimples can cause scars. Males should shave gently and infrequently if possible. Soften your beard with soap and water before putting on shaving cream. Avoid the sun. Some acne treatments will cause skin to sunburn more easily. Choose oil free makeup that is “noncomedogenic” which means that it will not clog pores. Shampoo your hair daily especially if oily. Keep hair off your face. What Makes Acne Worse? The hormone changes in females that occur 2 to 7 days prior to period starting each month. Bike helmets, backpacks, or tight collars putting pressure on acne prone skin Pollution and high humidity Squeezing or picking at pimples Scrubs containing apricot seeds. -

Urticarial Vasculitis Associated with Essential Thrombocythaemia
Acta Derm Venereol 2014; 94: 244–245 SHORT COMMUNICATION Urticarial Vasculitis Associated with Essential Thrombocythaemia Annabel D. Scott, Nicholas Francis, Helen Yarranton and Sarita Singh Dermatology Registrar, Department of Dermatology, Chelsea and Westminster Hospital, 369 Fulham Road, London SW10 9NH, United Kingdom. E-mail: [email protected] Accepted Apr 3, 2013; Epub ahead of print Aug 27, 2013 Urticarial vasculitis is a form of leucocytoclastic vas- prednisolone 30 mg once daily, which controlled her culitis whereby the skin lesions resemble urticaria. It is symptoms. associated with systemic lupus erythematosus, Sjögren’s A biopsy was taken from an uticarial lesion on the syndrome, hepatitis B and C viruses (1). Rarely it is asso- arm. Histology showed numerous perivascular neutro- ciated with an underlying haematological disorders and, phils and eosinophils with margination of neutrophils to the best of our knowledge, has never been reported in in the lumen of vessels and some leucocytoclasis with association with essential thrombocythaemia. We present red cell extravasation in keeping with an urticarial a case report of urticarial vasculitis associated with es- vasculitis (Fig. 2). sential thrombocythaemia. Blood tests revealed an erythrocyte sedimentation rate of 47 mm/h (normal range 1–12), a platelet count of 1,098 × 109/l (normal range 135–400) and an eosi- CASE REPORT nophilia of 1.0 × 109/l (normal range 0–0.2). Comple- A 32-year-old woman presented with a several month ment levels, thyroid function, serum iron, haemoglobin, history of recurrent urticaria without angioedema, 4 C-reactive protein, anti-nuclear antibody, anti-nuclear months post-partum. -

What Is Acne and Why Do I Have Pimples?
What is acne and why do I have pimples? The medical term for “pimples” is acne. Most people develop at least some acne, especially during their teenage years. Although many believe that acne comes from being dirty, this is not true; rather, acne is the result of changes that occur during puberty. Your skin is made of layers. To keep the skin from getting dry, the skin makes oil in little wells called “sebaceous glands” that are found in the deeper layers of the skin. “Whiteheads” or “blackheads” are clogged sebaceous glands. “Blackheads” are not caused by dirt blocking the pores, but rather by oxidation (a chemical reaction that occurs when the oil reacts with oxygen in the air). People with acne have glands that make more oil and are more easily plugged, causing the glands to swell. Hormones, bacteria (called P. acnes) and your family’s likelihood to have acne (genetic susceptibility) also play a role. SKIN HYGIENE Good skin care habits are important and support the medications your doctor prescribes for your acne. » Wash your face twice a day, once in the morning and once in the evening (which includes any showers you take). » Avoid over-washing/over-scrubbing your face as this will not improve the acne and may lead to dryness and irritation, which can interfere with your medications. » In general, milder soaps and cleansers are better for acne-prone skin. The soaps labeled “for sensitive skin” are milder than those labeled “deodorant soap” or “antibacterial soap.” » Many “acne washes” may contain salicylic acid. Salicylic acid (SA) fights oil and bacteria mildly but can be drying and can add to irritation. -

Sunburn, Suntan and the Risk of Cutaneous Malignant Melanoma the Western Canada Melanoma Study J.M
Br. J. Cancer (1985), 51, 543-549 Sunburn, suntan and the risk of cutaneous malignant melanoma The Western Canada Melanoma Study J.M. Elwood1, R.P. Gallagher2, J. Davison' & G.B. Hill3 1Department of Community Health, University of Nottingham, Queen's Medical Centre, Nottingham NG7 2UH, UK; 2Division of Epidemiology and Biometry, Cancer Control Agency of British Columbia, 2656 Heather Street, Vancouver BC, Canada V5Z 3J3; and 3Department of Epidemiology, Alberta Cancer Board, Edmonton, Alberta, Canada T6G OTT2. Summary A comparison of interview data on 595 patients with newly incident cutaneous melanoma, excluding lentigo maligna melanoma and acral lentiginous melanoma, with data from comparison subjects drawn from the general population, showed that melanoma risk increased in association with the frequency and severity of past episodes of sunburn, and also that melanoma risk was higher in subjects who usually had a relatively mild degree of suntan compared to those with moderate or deep suntan in both winter and summer. The associations with sunburn and with suntan were independent. Melanoma risk is also increased in association with a tendency to burn easily and tan poorly and with pigmentation characteristics of light hair and skin colour, and history freckles; the associations with sunburn and suntan are no longer significant when these other factors are taken into account. This shows that pigmentation characteristics, and the usual skin reaction to sun, are more closely associated with melanoma risk than are sunburn and suntan histories. -

Appendix Search Strategy Treatment of Hemophilia.Pdf
Appendix Search strategies Hemophilia – general aspects PubMed (NLM) September 2009 Von Willebrand disease (TiAb) AND Controlled clinical trial (PT) NOT Purpura, Thrombocytopenic (Me) Angiohemophilia (TiAb) Meta analysis (PT) Blood coagulation disorders (Me) Randomized controlled trial (PT) Hemophilia (TiAb) Systematic (SB) Haemophilia (TiAb) Bleeding disorder (TiAb) Random* (Ti) Bleeding disorders (TiAb) OR Control* (Ti) NOT Medline (SB) ("controlled clinical trial"[Publication Type] OR "meta analysis"[Publication Type] OR "randomized controlled trial"[Publication Type] OR systematic[sb] OR ((random*[Title] OR control*[Title]) NOT Medline[sb])) AND ("von Willebrand Disease"[title/abstract] OR "angiohemophilia"[title/Abstract] OR "Blood Coagulation Disorders"[Mesh terms] OR "hemophilia"[title/abstract] OR "haemophilia"[title/abstract] OR "bleeding disorder"[title/abstract] OR "bleeding disorders"[Title/abstract]) NOT "Purpura, Thrombocytopenic"[MeSH Terms] 211 Hemophilia – general aspects Embase.com (Elsevier) September 2009 Blood clotting factor deficiency (Exp,MJR) AND Clinical trial (Exp) NOT Thrombocytopenic purpura (Exp) Von Willebrand disease (Ti) Intervention study (De) Angiohemophilia (Ti) Longitudinal study (De) Angiohaemophilia (Ti) Prospective study (De) Hemophilia (Ti) Meta analysis (De) Haemophilia (Ti) Systematic review (De) Bleeding disorder (Ti) Random* (Ti) Bleeding disorders (Ti) Control* (Ti) ('blood clotting factor deficiency'/exp/mjOR 'von willebrand disease':ti OR 'angiohemophilia':ti OR 'angiohaemophilia':ti OR 'hemophilia':ti -
Immune Thrombocytopenic Purpura with Subsequent Development of JAK2 V617F-Positive Essential Thrombocythemia: Case Report
ISSN: 2640-7914 DOI: https://dx.doi.org/10.17352/ahcrr CLINICAL GROUP Received: 13 July, 2021 Case Report Accepted: 03 August, 2021 Published: 04 August, 2021 *Corresponding author: Marisabel Hurtado-Castillo, Immune thrombocytopenic PGY-3, Internal Medicine, Department of Medicine at NYU, 536 Ovington Avenue Apartment 3, Brooklyn NYC 11209, USA, Tel: 718-312-9641; purpura with subsequent Email: Keywords: Immune thrombocytopenic purpura; development of JAK2 Essential thrombocythemia; JAK-STAT signaling path- way; JAK2(V617F) mutation V617F-positive essential https://www.peertechzpublications.com thrombocythemia: Case Report Marisabel Hurtado-Castillo1*, Brian Flaherty2 and Morris Jrada2 1PGY-3, Internal Medicine, Department of Medicine at NYU, Brooklyn, NY, USA 2Clinical Assistant Professor, Department of Medicine at NYU Grossman School of Medicine, Brooklyn, NY, USA Abstract The sequential occurrence of Immune Thrombocytopenic Purpura (ITP) and Essential Thrombocythemia (ET) has been reported in the literature on a few occasions, as these are two hematologic disorders with distinct etiologies and patients usually have contrasting clinical presentations. Our case highlights the sequential occurrence of ITP, followed by Janus kinase 2 (JAK2) (V617F)-positive ET in a 64-year-old white woman, after four years of follow-up. The pathophysiology relating to these two conditions is incompletely understood, however, JAK2(V617F) mutation has been found in all the cases reported. Early identifi cation of JAK2(V617F) mutation in a patient with a -
USMPAKL00310919(1) AKLIEF Patient Brochure
You may pay as little as $0*† LIGHTEN YOUR LOAD Patients† May pay as little as: Avoid wearing a backpack or sports equipment with $0 commercially unrestricted | $75 uninsured patients a chin strap or anything that rubs against your skin, Visit GaldermaCC.com/patients which can cause acne to fl are. to download your savings card now. * Certain limitations may apply. Visit Galdermacc.com/patients for program details. GUARD AGAINST THE SUN † Galderma CareConnect is only available for commercially insured or uninsured patients. You may have heard spending time in the sun can Patients who are enrolled in a government-run or government-sponsored healthcare plan with a pharmacy benefi t are not eligible to use the Galderma CareConnect Patient help clear up skin but, in fact, sunlight may darken Savings Card. the appearance of acne and cause it to last longer. DON'T LET IMPORTANT SAFETY INFORMATION Be sure to ask your dermatology YOUR ACNE BE ® provider if you have any questions INDICATION: AKLIEF (trifarotene) Cream, 0.005% is a retinoid indicated for the topical treatment of acne THE FOCUS. about AKLIEF Cream. vulgaris in patients 9 years of age and older. ADVERSE EVENTS: The most common adverse reactions (incidence ≥ 1%) in patients treated with AKLIEF Cream were application site irritation, application site pruritus (itching), and sunburn. WARNINGS/PRECAUTIONS: Patients using AKLIEF Cream may experience erythema, scaling, dryness, and stinging/burning. Use a moisturizer from the initiation of treatment, and, if appropriate, depending upon the severity of these adverse reactions, reduce the frequency of application of AKLIEF Cream, suspend or discontinue use. -
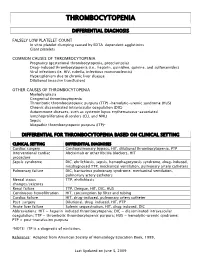
Thrombocytopenia.Pdf
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -

DRUG-INDUCED PHOTOSENSITIVITY (Part 1 of 4)
DRUG-INDUCED PHOTOSENSITIVITY (Part 1 of 4) DEFINITION AND CLASSIFICATION Drug-induced photosensitivity: cutaneous adverse events due to exposure to a drug and either ultraviolet (UV) or visible radiation. Reactions can be classified as either photoallergic or phototoxic drug eruptions, though distinguishing between the two reactions can be difficult and usually does not affect management. The following criteria must be met to be considered as a photosensitive drug eruption: • Occurs only in the context of radiation • Drug or one of its metabolites must be present in the skin at the time of exposure to radiation • Drug and/or its metabolites must be able to absorb either visible or UV radiation Photoallergic drug eruption Phototoxic drug eruption Description Immune-mediated mechanism of action. Response is not dose-related. More frequent and result from direct cellular damage. May be dose- Occurs after repeated exposure to the drug dependent. Reaction can be seen with initial exposure to the drug Incidence Low High Pathophysiology Type IV hypersensitivity reaction Direct tissue injury Onset >24hrs <24hrs Clinical appearance Eczematous Exaggerated sunburn reaction with erythema, itching, and burning Localization May spread outside exposed areas Only exposed areas Pigmentary changes Unusual Frequent Histology Epidermal spongiosis, exocytosis of lymphocytes and a perivascular Necrotic keratinocytes, predominantly lymphocytic and neutrophilic inflammatory infiltrate dermal infiltrate DIAGNOSIS Most cases of drug-induced photosensitivity can be diagnosed based on physical examination, detailed clinical history, and knowledge of drug classes typically implicated in photosensitive reactions. Specialized testing is not necessary to make the diagnosis for most patients. However, in cases where there is no prior literature to support a photosensitive reaction to a given drug, or where the diagnosis itself is in question, implementing phototesting, photopatch testing, or rechallenge testing can be useful. -

SUNBURN QUESTIONS and ANSWERS Don’T Fry Day
www.skincancerprevention.org SUNBURN QUESTIONS AND ANSWERS Don’t Fry Day Don’t Fry Day Sunburn Questions and Answers Why is it important to avoid sunburn on Don’t Fry Day - and every day? Sunburns are painful, and should be avoided for that reason. But sunburns represent skin damage. Your skin can repair some damage to DNA that results from too much sun, but this safety mechanism can be overwhelmed by the massive DNA damage caused by a sunburn. Mutations that are not repaired can lead to the development of skin cancer. This is why we should all avoid sunburn, especially for children. But wait, there’s more: sun’s skin-damaging ultraviolet (UV) rays also produce free radicals in skin cells, which can lead not only to cancer but also to wrinkles, blotches, and premature aging. If Don’t Fry Day is cloudy, I don’t need to take any preCautions, right? In fact, some of the worst sunburns happen on hazy days. Many people mistakenly assume that if it’s cool or cloudy outdoors they won’t get burned. They don’t realize that while clouds block the heat (infrared) energy, UV rays can still penetrate through quite strongly. What are other Causes of sunburn? Probably the most common cause of sunburn is accidental overexposure. Falling asleep while in the sun, forgetting to apply or re-apply sunscreen, or underestimating how quickly your skin will burn are typical mistakes. There may be no signs or symptoms while the overexposure is occurring because it can take hours following the exposure before the skin becomes red or tender. -

WHAT YOU NEED to KNOW ABOUT SEYSARA® a Novel Treatment Developed Specifi Cally for Acne
Not an actual patient, results may vary. WHAT YOU NEED TO KNOW ABOUT SEYSARA® A novel treatment developed specifi cally for acne. PLEASE SEE THE ACCOMPANYING PATIENT INFORMATION AND FULL PRESCRIBING INFORMATION. almirall.us INTRODUCING SEYSARA: A NOVEL ORAL ANTIBIOTIC TREATMENT DESIGNED SPECIFICALLY FOR ACNE WHAT IS SEYSARA? WHAT CAUSES ACNE? SEYSARA is a prescription medicine used to treat moderate to Acne appears when a small hole in our skin (pore) clogs with dead severe acne vulgaris in people 9 years and older. SEYSARA should not skin cells. Normally, dead skin cells rise to the surface of the pore, be used for the treatment or prevention of infections. It is not known where they are shed. Excess production of sebum—the oil that keeps if SEYSARA is safe and effective for use for longer than 12 weeks. our skin from drying out—can cause the dead skin cells to stick SEYSARA should not be used in children under 9 years of age, or if you together and get trapped inside the pore. 1 are pregnant or breastfeeding. Sometimes the bacteria that live naturally on our skin, C. acnes, also get inside the pore, where they can multiply quickly. With WHAT IS MODERATE TO SEVERE ACNE? bacteria inside, the pore becomes infl amed (red and swollen). If the acne goes deep into the skin, an acne cyst or nodule appears.4 Acne is a common skin condition involving blockage and/or infl ammation of hair follicles and their associated gland. Depending on the severity, acne is generally categorized as mild, moderate, or severe. -

Tanning? How Last Millennium Elizabeth Michaelson to Learn Whether Tanning’S Popu- Have to Clear Up
BEAUTY & ANTI-AGING Tanning? How Last Millennium ELIZABETH MICHAELSON To learn whether tanning’s popu- have to clear up. A healthy glow means larity has faded, we went right to the your [natural] skin tone, glowing. You, source: fashion and beauty magazines. looking luminous.” After an informal focus group of eight Larkworthy agrees. “Skin that’s not prominent beauty editors confirmed that tan is gorgeous… The more you take suntans are at last going out of style, we care of it and don’t subject it to the sun, conducted several in-depth follow-up the less makeup you need. Taking care Lois Johnson Valerie Monroe interviews. As Jane Larkworthy, Beauty of your skin is almost, in and of itself, a More Magazine O, The Oprah Magazine Director of W, notes, “I can’t remember type of foundation. It’s one step less in the last time I saw a tanned model in my your makeup routine — you don’t have magazine; I can’t remember the last time to cover up the wrinkles as much as you I saw a tanned model on the runway.” would if you’d spent 20 or 30 years in Tanning’s TIRED TYRANNY Val Monroe, O, The Oprah Magazine’s the sun.” Suntans promote a particularly Beauty Director, has likewise observed limited vision of health and beauty, consumers’ shifting attitudes: “I do no- YOU GLOW, GIRL since the popular image of the tanned tice more people walking around pale in But while UV tan-seeking is a no-no, all-American beauty was tradition- the summertime than there used to be.” a little glow, the kind that comes ally a light-skinned Caucasian whose Lois Johnson, Beauty Editor at More, from non-UV tanning products and golden glow was the result of UV puts it more flatly: “Tanning as a life bronzers, while still using sunscreen, exposure rather than genetic inheri- priority is over.” is still permissible and won’t sacrifice tance.