GDN Working Paper Series
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Upper East Region
REGIONAL ANALYTICAL REPORT UPPER EAST REGION Ghana Statistical Service June, 2013 Copyright © 2013 Ghana Statistical Service Prepared by: ZMK Batse Festus Manu John K. Anarfi Edited by: Samuel K. Gaisie Chief Editor: Tom K.B. Kumekpor ii PREFACE AND ACKNOWLEDGEMENT There cannot be any meaningful developmental activity without taking into account the characteristics of the population for whom the activity is targeted. The size of the population and its spatial distribution, growth and change over time, and socio-economic characteristics are all important in development planning. The Kilimanjaro Programme of Action on Population adopted by African countries in 1984 stressed the need for population to be considered as a key factor in the formulation of development strategies and plans. A population census is the most important source of data on the population in a country. It provides information on the size, composition, growth and distribution of the population at the national and sub-national levels. Data from the 2010 Population and Housing Census (PHC) will serve as reference for equitable distribution of resources, government services and the allocation of government funds among various regions and districts for education, health and other social services. The Ghana Statistical Service (GSS) is delighted to provide data users with an analytical report on the 2010 PHC at the regional level to facilitate planning and decision-making. This follows the publication of the National Analytical Report in May, 2013 which contained information on the 2010 PHC at the national level with regional comparisons. Conclusions and recommendations from these reports are expected to serve as a basis for improving the quality of life of Ghanaians through evidence-based policy formulation, planning, monitoring and evaluation of developmental goals and intervention programs. -

Preventing Illegal Gold Mining by Supporting Self Reliance
Preventing Illegal Gold Mining by Supporting Self Reliance Vocational Training in Upper East Region Talensi and Nabdam Districts, to develop trade skills and reduce illegal mining. TRAX, Ghana www.tfsr.org Preventing Illegal Gold Mining by Supporting Self Reliance Vocational Training in Upper East Region Talensi and Nabdam Districts, to develop trade skills and reduce illegal mining. Delivered by TRAX, Ghana This project aimed to reduce the number of young adults engaging in galamsey (illegal gold mining) by providing reliable and sustainable livelihood opportunities as an alternative way to earn an income. The presence of gold deposits discovered in the targeted communities has attracted a high number of unemployed young people, particularly those with a low level of formal education, into illegal small-scale gold-mining, locally referred to as galamsey. Due to the lack of opportunities, many young people turn to galamsey as a source of income. It is a high risk activity which causes environmental degradation, and social disruption. The project was located During this project, 22 young adults were trained in a trade in Bolgatanga, Ghana skill and equipped and supported to establish a small business and/or enter in to formal, safer employment. Each participant was attached to a master craftsperson and are supported to in turn train an additional two people upon completion of their training course. Project duration December 2017—December 2018 Project evaluation July 2019 Beneficiaries received training in either bicycle repairs, motorbike repairs, shoe repairs, tailoring, masonry or welding and fabrication. Their twelve-month programme also included literacy and numeracy, and an intensive life skills and functional business management programme. -
Afrikids Annual Report 2010 Statistics
Annual Report 2010 “ It’s remarkable what AfriKids has done for thousands of young lives in partnership with local communities and local government.” Colin Grassie CEO, Deutsche Bank UK AfriKids Annual Report 2011 Cover Image These children are from the Paramount Sirigu Chief’s family compound. Colin Grassie, CEO of Deutsche Bank UK, joined 47 colleagues on the experience of a lifetime in October 2010. He stayed in this compound. 01 01 Colin Grassie, CEO of Deutsche This annual report was designed Bank UK helps shell ground by Dave Brown from Ape Inc. Ltd nuts with AfriKids staff ember at a reduced cost. Ape Inc. Ltd, Joseph Asakibeem and together with David Carroll & Co, a beneficiary family of the also donated their time to rebrand Kassena Nankana Area AfriKids. This report was printed by Programme project Park Communications on Horizon Offset, a chlorine free paper sourced 02 Colin Grassie meets the from responsibly managed forests. Sirigu Elders Both the mill and the printer run ISO 03 The Chief of Sirigu, Colin’s host 14001 Environmental Management for the Deutche Bank Systems, Park are also Carbon Neutral Experience trip Paper and print was sourced at a 04 Colin takes a much needed discount by Urban Life Support Print 02 drink as the Chief’s son plays Management. with his new gift 05 AfriKids Ghana Director Nich This report is funded by the Venture Kumah and External Affairs Partnership Foundation (VPF). Manager Raymond Ayinne The majority of photographs in this share a joke in the Sumbrungu report are taken by AfriKids staff in Primary School grounds the UK and Ghana. -

Bawku West District
BAWKU WEST DISTRICT Copyright © 2014 Ghana Statistical Service ii PREFACE AND ACKNOWLEDGEMENT No meaningful developmental activity can be undertaken without taking into account the characteristics of the population for whom the activity is targeted. The size of the population and its spatial distribution, growth and change over time, in addition to its socio-economic characteristics are all important in development planning. A population census is the most important source of data on the size, composition, growth and distribution of a country’s population at the national and sub-national levels. Data from the 2010 Population and Housing Census (PHC) will serve as reference for equitable distribution of national resources and government services, including the allocation of government funds among various regions, districts and other sub-national populations to education, health and other social services. The Ghana Statistical Service (GSS) is delighted to provide data users, especially the Metropolitan, Municipal and District Assemblies, with district-level analytical reports based on the 2010 PHC data to facilitate their planning and decision-making. The District Analytical Report for the Bawku West district is one of the 216 district census reports aimed at making data available to planners and decision makers at the district level. In addition to presenting the district profile, the report discusses the social and economic dimensions of demographic variables and their implications for policy formulation, planning and interventions. The conclusions and recommendations drawn from the district report are expected to serve as a basis for improving the quality of life of Ghanaians through evidence- based decision-making, monitoring and evaluation of developmental goals and intervention programmes. -
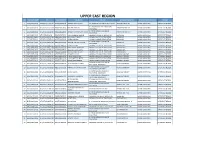
Upper East Region S.No Index Number Ntc Nss Number Full Name College School Posted To: Sponsorship District Region
UPPER EAST REGION S.NO INDEX_NUMBER NTC NSS_NUMBER FULL_NAME COLLEGE SCHOOL POSTED TO: SPONSORSHIP_DISTRICT REGION 1 SACE/0006/2018 NTC/GTLE/11319/18 NSSGTG7079518 ALBERTA ABULISONGA ST. AMBROSE COLLEGE OF EDUCATION ABANDE MEMO JHS BAWKU MUNICIPAL UPPER EAST REGION ST. BOSCO'S COLLEGE EDUCATION, 2 SBCE/0016/2018 NTC/GTLE/11225/18 NSSGTG6354818 RICHARD AKOLGO ABANDE MEMO JHS BAWKU MUNICIPAL UPPER EAST REGION NAVRONGO ST. JOHN BOSCO'S COLLEGE OF 3 SBCE/0058/2018 NTC/GTLE/04330/18 NSSGTG6352618 AYAMGA AKARIYAMBIRE ISAAC ABANDE MEMO JHS BAWKU MUNICIPAL UPPER EAST REGION EDUCATION 4 GBCE/0432/2018 GTLE/NR00580/19 NSSGTG7427018 SAANI ZUMBILA IBRAHIM GBEWAA COLLEGE OF EDUCATION BADOR JHS BAWKU MUNICIPAL UPPER EAST REGION 5 JACE/0197/2018 NTC/GTLE/23474/18 NSSGTG8077018 AHLI SAMUEL KWASI JASIKAN COLLEGE OF EDUCATION BADOR JHS BAWKU MUNICIPAL UPPER EAST REGION 6 JACE/0357/2018 NTC/GTLE/05297/18 NSSGTG6608618 AIKENS OWUANI JASIKAN COLLEGE OF EDUCATION BADOR JHS BAWKU MUNICIPAL UPPER EAST REGION ST. JOHN BOSCO'S COLLEGE OF 7 SBCE/0027/2018 NTC/GTLE/10064/18 NSSGTG6344718 ANYAGRI ABUGBIL ALFRED BADOR JHS BAWKU MUNICIPAL UPPER EAST REGION EDUCATION 8 GBCE/0298/2018 NTC/GTLE/19813/18 NSSGTG7446318 JIBREELA ISSAH GBEWAA COLLEGE OF EDUCATION BARIBARI JHS BAWKU MUNICIPAL UPPER EAST REGION 9 GBCE/0344/2018 NTC/GTLE/09615/18 NSSGTG7431218 MOHAMMED MANSURA GBEWAA COLLEGE OF EDUCATION BARIBARI JHS BAWKU MUNICIPAL UPPER EAST REGION 10 GBCE/0354/2018 NTC/GTLE/04736/18 NSSGTG6637918 ASSAMA-U MUSTAPHA GBEWAA COLLEGE OF EDUCATION BARIBARI JHS BAWKU MUNICIPAL UPPER -

CODEO's Statement on the Official Results of The
FOR IMMEDIATE RELEASE CODEO’S STATEMENT ON THE OFFICIAL RESULTS OF THE 2020 PRESIDENTIAL ELECTIONS CONTACT Mr. Albert Arhin CODEO National Coordinator Phone: +233 (0) 24 474 6791 / (0) 20 822 1068 Secretariat: +233 (0) 244 350 266/ 0277 744 777 Email: [email protected] Website: www.codeoghana.org Thursday, December 10, 2020 Accra, Ghana Introduction On Sunday, December 6, 2020, the Coalition of Domestic Election Observers (CODEO), in its press statement, communicated to the nation its intention to once again employ the Parallel Vote Tabulation (PVT) methodology to observe the 2020 presidential election, just as it did in 2008, 2012 and 2016. The PVT methodology is a reliable tool available to independent and non-partisan citizens’ election observer groups around the world for verifying the accuracy of official presidential elections results. In keeping with our protocols, which is that CODEO releases its PVT findings after the official results have been announced by the Electoral Commission, CODEO is here to release its PVT estimates for the presidential election. CODEO’s PVT estimates for the presidential results form part of its comprehensive election observation activities for the 2020 elections that covered voter registration exercise, pre-election environment observation for three months (September to November), and election day observation. The PVT Methodology The PVT is an advanced and scientific election observation technique that combines well-established statistical principles and Information Communication Technology (ICT) to observe elections. The PVT involves deploying trained accredited Observers to a nationally representative random sample of polling stations. On Election-Day, PVT Observers observe the entire polling process and transmit reports about the conduct of the polls and the official vote count in real-time to a central election observation database, using the Short Message Service (SMS) platform. -

The Senegambia Confederation In
Aka: The Continued Search for Appropriate Structures for Governance an AkaCameraReady final (Do Not Delete) 7/5/2017 10:05 AM CALIFORNIA WESTERN INTERNATIONAL LAW JOURNAL VOLUME 47 SPRING 2017 NUMBER 2 THE CONTINUED SEARCH FOR APPROPRIATE STRUCTURES FOR GOVERNANCE AND DEVELOPMENT IN AFRICA IN THE 21ST CENTURY: THE SENEGAMBIA CONFEDERATION IN HISTORICAL AND COMPARATIVE PERSPECTIVE PHILIP C. AKA*† * Professor of Political Science, Chicago State University; Adjunct Professor of Law, Indiana University Robert H. McKinney School of Law—Indianapolis; Member of the Illinois Bar; former Vice Chair, ABA Committee on International Human Rights; and Corresponding Editor, International Legal Materials (ILM); S.J.D., IU Robert H. McKinney School of Law—Indianapolis; Ph.D., Howard University; LL.M. (summa cum laude), IU Robert H. McKinney School of Law— Indianapolis; J.D., Temple University Beasley School of Law; M.A., University of North Texas; B.A. (magna cum laude), Edinboro University of Pennsylvania. Dr. Aka has written extensively on issues related to minority populations in Africa and the United States, including human rights. His recent publications germane to these topics include HUMAN RIGHTS IN NIGERIA’S EXTERNAL RELATIONS: BUILDING THE RECORD OF MORAL SUPERPOWER (Lexington Books, 2017), and Bridging the Gap Between Theory and Practice in Humanitarian Action: Eight Steps to Humanitarian Wellness in Nigeria, 24 WILLAMETTE JOURNAL OF INT’L LAW & DISPUTE RESOLUTION 1 (Fall 2016). † This Article evolved from a contribution to a festschrift for Professor Sulayman S. Nyang on his retirement following a distinguished academic career at 109 Published by CWSL Scholarly Commons, 2017 1 California Western International Law Journal, Vol. -

Talensi District
Table of Contents 1. ESTABLISHMENT OF THE DISTRICT ..................................................................................... 3 2. DISTRICT ECONOMY .................................................................................................................. 3 3. VISION OF THE DISTRICT ASSEMBLY................................................................................... 5 4. MISSION STATEMENT OF THE DISTRICT ASSEMBLY ...................................................... 6 5. KEY ACHIEVEMENTS IN 2018 ................................................................................................... 6 6. REVENUE AND EXPENDITURE PERFORMANCE .............................................................. 13 (a) REVENUE PERFORMANCE ............................................................................................. 13 REPUBLIC OF GHANA (b) EXPENDITURE PERFORMANCE .................................................................................... 15 7. GOAL ............................................................................................................................................. 15 8. CORE FUNCTIONS ..................................................................................................................... 15 COMPOSITE BUDGET 9. NMTDF POLICY OBJECTIVES ................................................................................................ 17 10. POLICY OUTCOME INDICATORS AND TARGETS ........................................................ 17 11. Revenue Mobilization Strategies -

2023 Programme Based Budget Estimates for 2020 Kassena
For copies of the KNMA PBB Estimates, please contact the address below: The Municipal Coordinating Director, Kassena Nankana Municipal Assembly P .O .Box 1 Navrongo, Upper East Region REPUBLIC OF GHANA The KNMA MTEF PBB Estimate for 2020 is also available on the internet at: COMPOSITE BUDGET www.mofep.gov.gh or www.ghanadistricts.com FOR 2020 - 2023 PROGRAMME BASED BUDGET ESTIMATES FOR 2020 KASSENA NANKANA MUNICIPAL 1 2 Table of Contents ACRONYMS ACRONYMS ............................................................................................................................................... 4 AEAs Agricultural Extension Agents PART A: STRATEGIC OVERVIEW ........................................................................................................ 5 BAC Business Advisory Centre CHPs Community Health Planning Services 1. Establishment of the District ........................................................................................................ 5 CLTS Community Led Total Sanitation 3. Municipal Economy: ....................................................................................................................... 5 DACF District Assemblies Common Fund 4. Vision statement of the Municipal Assembly ........................................................................... 9 DDF District Development Fund 5. Mission statement of the Municipal Assembly ........................................................................ 9 DRI District Response Initiative DPAT District Assemblies Performance Assessment Tool -

Financial and Technical Resources Available to the Education Sector in Senegal, Mali, Guinea and Ghana
Financial and Technical Resources Available to the Education Sector in Senegal, Mali, Guinea and Ghana Version 1.0 Published October 2005 1 ACKNOWGLEDGEMENTS Many people have provided guidance, information, time and energy to make this work possible. Thank you to those who gave freely of their time to furnish the information contained in these pages. Susan Gannon, an independent consultant based in Dakar, has done the majority of work in collecting information and developing this guide. For this and for being a solid long-term partner, MTT West wishes to extend their deep appreciation. A particular word of thanks to the MTT/West Project’s Administrative Coordinator, Valerie Moulay-Omar, for the many hours of proof reading that have resulted in the publication of this document. Grey Cardigan Consulting provided editing and formatting services for this document. They can be reached at [email protected]. This Guide is made possible by the support from USAID under the terms of Cooperative Agreement No. RLA-A-A-00-03-00026-00. Any opinions expressed are those of the authors and do not necessarily reflect the views of USAID. 2 3 HOW TO USE THIS GUIDE The fight against HIV/AIDS requires resources and the purpose of this tool is to assist you in identifying financial and technical resources available to the education sector in Senegal, Mali, Guinea and Ghana. Of course, this information is current as we go to press but change is occurring at a rapid pace, resources continue to be made available and new alliances are being formed between donors and other stakeholders. -

Landscape Report on Early Grade Literacy
Landscape Report on Early Grade Literacy Landscape Report on Early Grade Literacy August 26, 2016 Young-Suk Grace Kim,1 Helen N. Boyle,2 Stephanie Simmons Zuilkowski,2 and Pooja Nakamura3 1 School of Education, University of California at Irvine 2 College of Education and Learning Systems Institute, Florida State University 3 American Institutes for Research Suggested citation: Kim, Y.-S. G., Boyle, H. N., Zuilkowski, S. S., & Nakamura, P. (2016). Landscape Report on Early Grade Literacy. Washington, D.C.: USAID. Disclaimer The views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development. RIGHTS AND PERMISSIONS — This work is available under the Creative Commons Attribution 3.0 IGO license (CC BY 3.0 IGO) http://creativecommons.org/licenses/by/3.0/igo. Under the Creative Commons Attribution license, you are free to copy, distribute, transmit and adapt this work, including for commercial purposes, under the following conditions: Attribution—Please cite the work as follows: LICENSE: Creative Commons Attribution CC BY 3.0 IGO TRANSLATIONS — If you create a translation of this work, please add the following disclaimer along with the attribution: This translation was not created by USAID and should not be considered an official USAID translation. USAID shall not be liable for any content or error in this translation. ADAPTATIONS — If you create an adaptation of this work, please add the following disclaimer along with the attribution: This is an adaptation of an original work by USAID. Views and opinions expressed in the adaptation are the sole responsibility of the author or authors of the adaptation and are not endorsed by USAID. -

Paper Title: Institutional Pluralism in Charcoal Chain in a Context of Decentralization in Senegal: the Stakes for Local Democracy
Papa Faye Associated researcher at CODESRIA Ph. D candidate in Sociology, UCAD, SENEGAL Tel: 542 68 44 [email protected] WRI Reviewed draft for Institutional Choice and Recognition: Effects on the Formation and Consolidation of Local Democracy Program. Panel 1: Institutional Choice and Recognition in Natural Resource Management: Competition, Cooperation and Conflict among Local Institutions Paper title: Institutional Pluralism in charcoal chain in a context of Decentralization in Senegal: The Stakes for Local Democracy. 2nd draft, 24 April 2006 1 I. Introduction As African and third-world States, politics of decentralization has been engaged in Senegal, early in the last century (Diagne 2003). But, the phase which interest us starts at the local “collectivities code” promulgation in 1996. By this code, government of Senegal settles three forms of “local collectivities”: rural communities, communes and regions in urban areas. In the nine powers they have received was the management of environment and natural resources. So the code the former code of 1993 which doesn’t integrated decentralization considerations was called to be reviewed in 1998. The particularity of the Senegalese political decentralization reforms is fist, the fact that it we’ll be accompanied by an administrative decentralization – “deconcentration”–process. Second, the forestry service needed projects and programs to embody the “new inclusive” politics (RDS Communication of 1980). So, PROGEDE was the model designed by the national forestry service to be tried out. As other projects in forestry, it created its own institutions: villagers committees of management and development (CVGD)1 and inter villagers committees of management and development (CIVGD) in addition to the pre-existing institutions –traditional like village chiefs–.