Strengthening Community Systems. for HIV Treatment Scale-Up
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

11010329.Pdf
THE RISE, CONSOLIDATION AND DISINTEGRATION OF DLAMINI POWER IN SWAZILAND BETWEEN 1820 AND 1889. A study in the relationship of foreign affairs to internal political development. Philip Lewis Bonner. ProQuest Number: 11010329 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 11010329 Published by ProQuest LLC(2018). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 ABSTRACT The Swazi kingdom grew out of the pressures associated with competition for trade and for the rich resources of Shiselweni. While centred on this area it acquired some of its characteristic features - notably a regimental system, and the dominance of a Dlamini aristocracy. Around 1815 the Swazi came under pressure from the South, and were forced to colonise the land lying north of the Lusutfu. Here they remained for some years a nation under arms, as they plundered local peoples, and were themselves swept about by the currents of the Mfecane. In time a more settled administration emerged, as the aristocracy spread out from the royal centres at Ezulwini, and this process accelerated under Mswati as he subdued recalcitrant chiefdoms, and restructured the regiments. -

Swaziland Government Gazette
Swaziland Government Gazette VOL. XIX] MBABANE, Friday, February 27th., 1981 [No. 85 CONTENTS No. Page GENERAL NOTICES 6. The Control of Insurance Brokers and Agents Regulations, ... .......... 102 7. Appointment of Assistant Registrar (Births, Marriages and Deaths) _ _ 103 8. Authorisation of Change of Surname ... ....... .................. -................ 103 9. Authorisation of Change of Surname _ — — -................. .. 104 10. Authorisation of Change of Surname .......... ................... — _ _ 104 MISCELLANEOUS Notice of Applications under the Road Transportation Proclamation, 1963 — 105 ADVERTISEMENTS ........ 112 CONTENTS OF SUPPLEMENT PART A — BILLS 3. The Deeds Registry (Amendment) Bill, 1981 — — ........... — — — — — — SI 4. The Crown Lands Disposal (Amendment) Bill, 1981 — — — — — — ~~~ — S2 PART C — LEGAL NOTICES 14. The Fixation of Powdered Milk and Allied Products Prices Regulations, 1981 — — S3 15. The Premiums for Insurance of Motor Vehicles (Amendment) Notice, 1981 — — S6 PUBLISHED BY AUTHORITY. 102 GENERAL NOTICE NO. 6 OF 1981 THE CONTROL OF INSURANCE ORDER, 1973 (King’s Order-in-Council No. 33 of 1973) THE CONTROL OF INSURANCE BROKERS AND AGENTS REGULATIONS, 1973 It is hereby notified for general information that the Honourable Minister of Finance has appointed the under-mentioned persons as Insurance Agents. Name Address Simon N. Mahlaba P.O. Box 494, Mbabane Octavius Msomi P.O. Box Al 19 Mbabane It is further notified that the Minister has removed — Name Address J.P. Vilakati P.O. Box 162, Kwaluseni G.M. Sikiti P.O. Box 97, Nhlangano P.O. Box 167, John M. Xaba Bhunya From the list of Agents appointed under General Notices No. 146 of 1975, No, 2 of 1978 and No. 63 of 1979, respectively. -
Swaziland-VMMC-And-EIMC-Strategy
T ABLE OF C ONTENTS Table of Contents .........................................................................................................................................................................................i List of Tables ............................................................................................................................................................................................. iii List of Figures ............................................................................................................................................................................................ iii List of Boxes .............................................................................................................................................................................................. iii List of Acronyms ......................................................................................................................................................................................... iv Foreword ..................................................................................................................................................................................................... vi Acknowledgements.................................................................................................................................................................................... vii EXECUTIVE SUMMARY ...................................................................................................................................................................... -

Baphalali Swaziland Red Cross Society Clinics & Divisions Performance
BAPHALALI SWAZILAND RED CROSS SOCIETY CLINICS & DIVISIONS PERFORMANCE 2013 PREPARED BY: ELLIOT JELE PROGRAMMES MANAGER DATE: 8TH AUGUST, 2014 i TABLE OF CONTENTS TABLE OF CONTENTS ........................................................................................................................................ II 1. INTRODUCTION ............................................................................................................................................ 1 2. PROGRAMMES DESCRIPTION ....................................................................................................................... 2 3. ACHIEVEMENTS IN 2013 ............................................................................................................................... 2 3.1. HEALTH AND SOCIAL SERVICES ................................................................................................................. 2 3.1.1. GOAL- HEALTH & SOCIAL SERVICES ........................................................................................................ 2 3.1.2. OBJECTIVES - HEALTH & SOCIAL SERVICES .............................................................................................. 3 3.1.3. OVERALL HEALTH & SOCIAL SERVICES ACHIEVEMENTS .......................................................................... 3 3.1.4. ACHIEVEMENT PER PROGRAME COMPONENT, & OUTCOME LEVEL ....................................................... 3 ORPHANED AND VULNERABLE CHILDREN ....................................................................................................... -

2000 334000 336000 338000 340000 342000 31°16'0"E 31°17'0"E 31°18'0"E 31°19'0"E 31°20'0"E 31°21'0"E 31°22'0"E 31°23'0"E 31°24'0"E 31°25'0"E
326000 328000 330000 332000 334000 336000 338000 340000 342000 31°16'0"E 31°17'0"E 31°18'0"E 31°19'0"E 31°20'0"E 31°21'0"E 31°22'0"E 31°23'0"E 31°24'0"E 31°25'0"E GLIDE number: TC-2021-000008-MOZ Activation ID: EMSR495 Int. Charter call ID: N/A Product N.: 04MANZINI, v2 0 0 0 0 0 0 4 4 7 7 Manzini - ESWATINI 0 0 7 7 Storm - Situation as of 30/01/2021 S " 0 ' Grading - Overview map 01 7 2 ° 6 2 S " 0 Mpumalanga ' Maputo 7 2 ° 6 2 Maputo^ Mozambique Channel Baia de Hhohho Maputo Mozambique Ekukhanyeni SouthMaputo Africa 03 Mozambique Channel Mbabane Manzini 05 ^ 0 0 (! Eswatini 0 0 04 0 0 2 2 7 7 0 0 Manzini INDIAN 7 7 OCEAN S " Lubombo 0 ' 8 2 ° 6 o 2 ut S p " a 0 ' M 8 2 ° 6 Ludzeludze 2 20 Shiselweni Kwazulu-Natal km Cartographic Information 1:25000 Full color A1, 200 dpi resolution 0 0.5 1 2 km 0 0 0 0 Grid: WGS 1984 UTM Zone 36S map coordinate system 0 0 0 0 7 7 Tick marks: WGS 84 geographical coordinate system S 0 0 " 7 7 0 ± ' 9 2 ° 6 2 S " 0 ' 9 2 ° Legend 6 2 Crisis Information Transportation Grading Facilities Grading Hydrography Road, Damaged Dam, Damaged River Blocked road / interruption Road, Possibly damaged General Information Stream Flooded Area Area of Interest (30/01/2021 07:55 UTC) Railway, Damaged Lake Detail map Flood trace Highway, No visible damage Manzini North Not Analysed Built Up Grading Primary Road, No visible damage Manzini Destroyed Administrative boundaries Secondary Road, No visible damage Possibly damaged Province Local Road, No visible damage Placenames Cart Track, No visible damage ! Placename Detail 02 Long-distance railway, No visible damage a Airfield runway, No visible damage n Land Use - Land Cover a Matsapha ! w Manzini Features available in the vector package h ! s Consequences within the AOI u s Possibly Total Total in u Destroyed Damaged 0 Lobamba 0 damaged* affected** AOI L 0 0 S " 0 0 ha 13.8 0 Flooded area ' 8 8 0 3 6 Lomdzala 6 ha 44.1 ° Flood trace 0 0 6 2 7 7 S Estimated population 573 177,811 " 0 ' 0 Built-up No. -
2018 Annual Report
Vision: Vision: Partner Partner of choice of choice in alleviating in alleviating human human suffering suffering in Swaziland in Swaziland i Baphalali Eswatini Red Cross Society 2018 ANNUAL REPORT Baphalali demonstrates to a drought hit Lavumisa, Etjeni Chiefdom Community member on how to practice conservation agriculture (CA) using a seed driller. Photographer: BERCS Communications Department Mission: Saving lives, changing minds Mission: Saving lives, changing minds ii TABLE OF CONTENTS TABLE OF CONTENTS .................................................................................................................................... II PRESIDENT’S REMARKS ................................................................................................................................ 1 SECRETARY GENERAL’S SUMMARY ......................................................................................................... 4 INTRODUCTION ................................................................................................................................................ 5 ACHIEVEMENTS ............................................................................................................................................... 5 1.0 HEALTH AND SOCIAL SERVICES ................................................................................................... 5 1.1 PRIMARY HEALTH CARE: MOTHER, INFANT, CHILD HEALTH, CURATIVE, AND HIV/TB . 5 2.0 FIRST AID .............................................................................................................................................. -

Swaziland Government
SWAZILAND GOVERNMENT Telephone: (+268) 24046244, Ministry of Natural Resources & Energy 24045376 P. O. Box 57, Fax: (+268)24044851/24047252 Mbabane, E-mail: [email protected] Swaziland 20th January, 2016. UPDATE FROM THE MINISTER ON THE DROUGHT AND CURRENT WATER SCARCITY BACKGROUND 1. Swaziland and the Southern African region is currently undergoing a very serious drought situation. Climate Change has worsened the situation and the country has been experiencing below average rainfall in the past three (3) years. We are advised this severe drought along with a scorching heat wave (El Nino) is one of the strongest on record, and is unfortunately unyielding. 2. Our current state of water storage across the country is seriously below the long term averages observed over the past five (5) years. This situation is as a result of the low river flows due to the lack of sufficient rainfall to recharge our river systems to fill up the dams. Currently our four (4) major dams; namely Hawane, Maguga, Mnjoli and Lubovane are recording very low levels of water storage. These dams are currently recording 6%, 35%, 6 % and 67% respectively. Government notes that all the five major river basins of the country have been greatly affected. In the Ngwavuma Basin there is currently no irrigation taking place as the river has since dried up. The Mbuluzi, Lusutfu, Lomati and Komati are also quickly following suit. While the situation calls for the implementation of robust measures; the Ministry is aware of the impact the complete 1 suspension of commercial irrigation in these river systems would have on the national economy and the country’s commitment to international markets. -
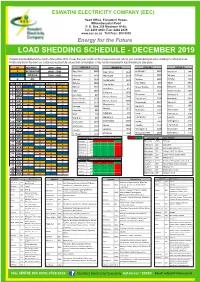
Load Shedding Schedule - December 2019
ESWATINI ELECTRICITY COMPANY (EEC) Head Office, Eluvatsini House, Mhlambanyatsi Road P. O. Box 258 Mbabane H100, Tel: 2409 4000, Fax: 2404 2335 www.eec.co.sz Toll Free: 800 9000 Energy for the Future LOAD SHEDDING SCHEDULE - DECEMBER 2019 Possible load shedding for the month of December 2019. Please find your location in the groups below and refer to your load shedding schedule detailing the affected areas. Kindly note that in the event our customers successfully reduce their consumption, it may not be necessary for load shedding to take place. M MORNING 10h00 - 14h00 GROUP A GROUP B GROUP C GROUP D A AFTERNOON 14h00 - 17h00 Pigg's Peak 3480 Pigg's Peak 3440 Endzingeni 3810 Mayiwane 3940 E EVENING 17h00 - 21h00 Mayiwane 3950 Mayiwane 3970 Sihhoye 2660 Sihhoye 2670 Nkhaba 3890 O OFF Sihhoye 2690 Dvokolwako 1320 Nkhaba 3860 Nkhaba 3880 Pine Valley 830 Mpisi 5640 DATE DAY GROUP A GROUP B GROUP C GROUP D Pine Valley 810 1 SUN E O M A Nkhaba 3870 Moses Hlophe 5350 Balegane 2610 Kent Rock 824 2 MON A E O M Mpisi 5650 Siteki 1230 Moses Hlophe 5360 3 TUE M A E O Balegane 2620 Kent Rock 827 Thompson 622 Siphocosini 925 4 WED O M A E Moses Hlophe 5340 5 THU E O M A Moses Hlophe 5330 Siphofaneni 5740 Riverbank 5090 Moses Hlophe 5380 6 FRI A E O M Moses Hlophe 5370 Thabankulu 3977 Manzini 1 508 7 SAT M A E O Magwabayi 542 KaLanga 1240 Big Bend 5014 Usutu 1093 8 SUN O M A E Mpaka 1227 9 MON E O M A Lobamba 950 Matsapha 2300 Sidvokodvo 630 10 TUE A E O M SPM 108 Edwaleni 104 Usutu 1094 Hlathikhulu 2180 11 WED M A E O Manzini 1 504 Sidvokodvo 636 Lawuba -

Swaziland Country Operational Plan 2018 Strategic Direction Summary
SWAZILAND Country Operational Plan (COP) 2018 Strategic Direction Summary March 29, 2018 Acronym and Word List A Adolescents AE Adverse Event AG Adolescent Girls AGYW Adolescent Girls and Young Women ALHIV Adolescents Living with HIV ANC Antenatal Clinic APR Annual Program Results ARROWS ART Referral, Retention, and Ongoing Wellness Support ARV Antiretroviral ART Antiretroviral Therapy ASLM African Society for Laboratory Medicine C Children C/A Children/Adolescents CAG Community Adherence Group CANGO Coordinating Assembly of Non-Governmental Organizations CCM Country Coordinating Mechanism CEE Core Essential Element CHAI Clinton Health Access Initiative CIHTC Community-Initiated HIV Testing and Counseling CMIS Client Management Information System CMS Central Medical Stores CoAg Cooperative Agreement CQI Continuous Quality Improvement CS(O) Civil Society (Organizations) DBS Dried Blood Spot DQA Data Quality Assessment DSD Direct Service Delivery E Swazi Emalangeni (1 lilangeni equals 1 rand) ECD Early Childhood Development EID Early Infant Diagnosis eNSF extended National Multi-Sectoral Strategic Framework for HIV & AIDS EQA External Quality Assessment DMPPT Decision Makers Program Planning Toolkit EU European Union FDC Fixed dose combination FDI Foreign Direct Investment FP Family Planning FSW Female Sex Workers GBV Gender Based Violence GHSP Global Health Services Partnership GKoS Government of the Kingdom of Swaziland GF Global Fund to fight AIDS, Tuberculosis and Malaria GDP Gross Domestic Product GNI Gross National Income HC4 HIV -

Page 1 2018 NATIONAL ELECTIONS
2018 NATIONAL ELECTIONS - POLLING STATIONS REGION INKHUNDLA POLLING DIVISION HHOHHO HHUKWINI Dlangeni HHUKWINI KaSiko HHUKWINI Lamgabhi HHUKWINI Lamgabhi HHUKWINI Sitseni LOBAMBA Elangeni LOBAMBA Ezulwini LOBAMBA Ezulwini LOBAMBA Ezulwini LOBAMBA Lobamba LOBAMBA Nkhanini LOBAMBA Nkhanini LOBAMBA Zabeni LOBAMBA Zabeni MADLANGEMPISI Dvokolwako / Ekuphakameni MADLANGEMPISI Dvokolwako / Ekuphakameni MADLANGEMPISI Ekukhulumeni/ Mandlangempisi MADLANGEMPISI Ekukhulumeni/ Mandlangempisi MADLANGEMPISI Gucuka MADLANGEMPISI Mavula MADLANGEMPISI Nyonyane/ Maguga MADLANGEMPISI Tfuntini/Buhlebuyeza MADLANGEMPISI Tfuntini/Buhlebuyeza MADLANGEMPISI Tfuntini/Buhlebuyeza MADLANGEMPISI Tfuntini/Buhlebuyeza MADLANGEMPISI Zandondo MADLANGEMPISI Zandondo MAPHALALENI Dlozini MAPHALALENI Madlolo MAPHALALENI Maphalaleni MAPHALALENI Mcengeni MAPHALALENI Mfeni MAPHALALENI Nsingweni MAPHALALENI Nsingweni MAYIWANE Herefords MAYIWANE Mavula MAYIWANE Mfasini MAYIWANE Mkhuzweni MAYIWANE Mkhuzweni MAYIWANE Mkhweni MBABANE EAST Fontein MBABANE EAST Fontein MBABANE EAST Mdzimba/Lofokati MBABANE EAST Mdzimba/Lofokati MBABANE EAST Msunduza MBABANE EAST Msunduza MBABANE EAST Msunduza MBABANE EAST Sidwashini MBABANE EAST Sidwashini MBABANE EAST Sidwashini MBABANE EAST Sidwashini MBABANE WEST Mangwaneni MBABANE WEST Mangwaneni MBABANE WEST Mangwaneni MBABANE WEST Manzana MBABANE WEST Nkwalini MBABANE WEST Nkwalini MBABANE WEST Nkwalini MBABANE WEST Nkwalini MHLANGATANE Emalibeni MHLANGATANE Mangweni MHLANGATANE Mphofu MHLANGATANE Mphofu MHLANGATANE Ndvwabangeni MHLANGATANE -

Grantor: Dining for Women Project Title: WORTH: Investing in the Economic Security of Eswatini's Female Caretakers Duration
Grantor: Dining for Women Project Title: WORTH: Investing in the Economic Security of Eswatini's Female Caretakers Duration: 2 Years Project Dates: January 2020 – December 2021 Period covered in this report: 2 January 2020 – 15 December 2020 Representative: Mr. Khulekani Magongo Position: Executive Director Address: P. O. Box 7967, Mbabane. Eswatini Lot 33, Pholinjane Road, Malunge Township, Farm 2, Dalriach No. 188, Mbabane Telephone: +268 7806 3607 Email: [email protected] www.youngheroes.org.sz Ms. Sithandazile Dube - Project Manager Project team: Mr. Maxwell Simelane- Project Officer Mrs. Xolisile Mpanza - Project Officer. Project Objectives The economic strengthening project aims to mitigate gender inequalities and socioeconomic disparities to all orphan and vulnerable (OVC) caregivers and encourage participation in the WORTH groups. In the first year, 199 caregivers participate in 10 groups, and each group comprises 20 members starting in the Lubombo region. The overall goal is to improve OVC households' economic status so that they are self-reliant and sustain themselves economically. This is achieved by bringing women together into groups, encouraging participation, financial literacy training, and managing Income Generating Activities (IGAs). The changes expected at the end of the project are: • The economic condition of participating women and their children improves as the women become financially literate and support each other in establishing microenterprises. This additional income will strengthen their families' health via better nutrition and provide funds for household necessities and school tuitions. • Women will be financially literate and create the opportunity for them to become self- sufficient microentrepreneurs. Funding The program remains fully funded by the grant provided by Dining for Women and implemented by Young Heroes in Eswatini. -

Swaziland Technology Needs Assessment Report 1
SWAZILAND TECHNOLOGY NEEDS ASSESSMENT REPORT 1 CLIMATE CHANGE ADAPTATION Revised Draft 15 June 2016 Prepared by Deepa Pullanikkatil (PhD), CANGO Table of Contents Chapter 1 Introduction ................................................................................................................................ 6 1.1 Background of TNA project ........................................................................................................................ 6 1.2 Existing national policies related to technological innovation, adaptation to climate change and development priorities ............................................................................................................................................. 7 1.3 Vulnerability assessments in the country .................................................................................................. 11 1.4 Sector selection ......................................................................................................................................... 14 1.4.1 An Overview of Expected Climate Change and its Impacts in Sectors Vulnerable to Climate Change ... 14 1.4.2 Process and results of sector selection .................................................................................................. 24 Chapter 2 Institutional arrangement for the TNA and the stakeholder involvement ................................. 26 2.1 National TNA team ..................................................................................................................................