Swaziland Country Operational Plan 2018 Strategic Direction Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Strengthening Community Systems. for HIV Treatment Scale-Up
Strengthening Community Systems. for HIV Treatment Scale-up. A case study on MaxART community. interventions in Swaziland. Colophon Strengthening Community Systems for HIV Treatment Scale-up A case study on MaxART community interventions in Swaziland Published: June 2015 Author: Françoise Jenniskens Photos: Adriaan Backer Design: de Handlangers For more information on the MaxART programme visit: www.stopaidsnow.org/treatment-prevention MINISTRY OF HEALTH KINGDOM OF SWAZILAND The Swaziland Ministry of Health, STOP AIDS NOW!, and the Clinton Health Access Initiative (CHAI) initiated the MaxART project in Swaziland. The programme partners include the Swaziland Network of People Living with HIV and AIDS (SWANNEPHA) and the Global Network of People Living with HIV (GNP+), the National Emergency Response Council on HIV/AIDS (NERCHA), national and international non-governmental organisations including the Southern Africa HIV & AIDS Information Dissemination Service (SAfAIDS), social scientists from the University of Amsterdam and researchers from the South African Centre for Epidemiological Modelling and Analysis (SACEMA). 2 Strengthening Community Systems for HIV Treatment Scale-up Acknowledgements Without the support of all the different partners in Swaziland it would not have been possible to draft this case study report. I would like to thank the respondents from the MoH and NERCHA for their extremely helpful insights in community systems strengthening issues in Swaziland and availing their time to talk to me within their busy time schedules. Furthermore I would like to express my gratitude to both Margareth Thwala-Tembe of SAfAIDS and Charlotte Lejeune of CHAI for their continuous support during my visit and for arranging all the appointments; dealing with logistics and providing transport for visiting the regions and key informants. -
Swaziland-VMMC-And-EIMC-Strategy
T ABLE OF C ONTENTS Table of Contents .........................................................................................................................................................................................i List of Tables ............................................................................................................................................................................................. iii List of Figures ............................................................................................................................................................................................ iii List of Boxes .............................................................................................................................................................................................. iii List of Acronyms ......................................................................................................................................................................................... iv Foreword ..................................................................................................................................................................................................... vi Acknowledgements.................................................................................................................................................................................... vii EXECUTIVE SUMMARY ...................................................................................................................................................................... -

Baphalali Swaziland Red Cross Society Clinics & Divisions Performance
BAPHALALI SWAZILAND RED CROSS SOCIETY CLINICS & DIVISIONS PERFORMANCE 2013 PREPARED BY: ELLIOT JELE PROGRAMMES MANAGER DATE: 8TH AUGUST, 2014 i TABLE OF CONTENTS TABLE OF CONTENTS ........................................................................................................................................ II 1. INTRODUCTION ............................................................................................................................................ 1 2. PROGRAMMES DESCRIPTION ....................................................................................................................... 2 3. ACHIEVEMENTS IN 2013 ............................................................................................................................... 2 3.1. HEALTH AND SOCIAL SERVICES ................................................................................................................. 2 3.1.1. GOAL- HEALTH & SOCIAL SERVICES ........................................................................................................ 2 3.1.2. OBJECTIVES - HEALTH & SOCIAL SERVICES .............................................................................................. 3 3.1.3. OVERALL HEALTH & SOCIAL SERVICES ACHIEVEMENTS .......................................................................... 3 3.1.4. ACHIEVEMENT PER PROGRAME COMPONENT, & OUTCOME LEVEL ....................................................... 3 ORPHANED AND VULNERABLE CHILDREN ....................................................................................................... -

2000 334000 336000 338000 340000 342000 31°16'0"E 31°17'0"E 31°18'0"E 31°19'0"E 31°20'0"E 31°21'0"E 31°22'0"E 31°23'0"E 31°24'0"E 31°25'0"E
326000 328000 330000 332000 334000 336000 338000 340000 342000 31°16'0"E 31°17'0"E 31°18'0"E 31°19'0"E 31°20'0"E 31°21'0"E 31°22'0"E 31°23'0"E 31°24'0"E 31°25'0"E GLIDE number: TC-2021-000008-MOZ Activation ID: EMSR495 Int. Charter call ID: N/A Product N.: 04MANZINI, v2 0 0 0 0 0 0 4 4 7 7 Manzini - ESWATINI 0 0 7 7 Storm - Situation as of 30/01/2021 S " 0 ' Grading - Overview map 01 7 2 ° 6 2 S " 0 Mpumalanga ' Maputo 7 2 ° 6 2 Maputo^ Mozambique Channel Baia de Hhohho Maputo Mozambique Ekukhanyeni SouthMaputo Africa 03 Mozambique Channel Mbabane Manzini 05 ^ 0 0 (! Eswatini 0 0 04 0 0 2 2 7 7 0 0 Manzini INDIAN 7 7 OCEAN S " Lubombo 0 ' 8 2 ° 6 o 2 ut S p " a 0 ' M 8 2 ° 6 Ludzeludze 2 20 Shiselweni Kwazulu-Natal km Cartographic Information 1:25000 Full color A1, 200 dpi resolution 0 0.5 1 2 km 0 0 0 0 Grid: WGS 1984 UTM Zone 36S map coordinate system 0 0 0 0 7 7 Tick marks: WGS 84 geographical coordinate system S 0 0 " 7 7 0 ± ' 9 2 ° 6 2 S " 0 ' 9 2 ° Legend 6 2 Crisis Information Transportation Grading Facilities Grading Hydrography Road, Damaged Dam, Damaged River Blocked road / interruption Road, Possibly damaged General Information Stream Flooded Area Area of Interest (30/01/2021 07:55 UTC) Railway, Damaged Lake Detail map Flood trace Highway, No visible damage Manzini North Not Analysed Built Up Grading Primary Road, No visible damage Manzini Destroyed Administrative boundaries Secondary Road, No visible damage Possibly damaged Province Local Road, No visible damage Placenames Cart Track, No visible damage ! Placename Detail 02 Long-distance railway, No visible damage a Airfield runway, No visible damage n Land Use - Land Cover a Matsapha ! w Manzini Features available in the vector package h ! s Consequences within the AOI u s Possibly Total Total in u Destroyed Damaged 0 Lobamba 0 damaged* affected** AOI L 0 0 S " 0 0 ha 13.8 0 Flooded area ' 8 8 0 3 6 Lomdzala 6 ha 44.1 ° Flood trace 0 0 6 2 7 7 S Estimated population 573 177,811 " 0 ' 0 Built-up No. -
2018 Annual Report
Vision: Vision: Partner Partner of choice of choice in alleviating in alleviating human human suffering suffering in Swaziland in Swaziland i Baphalali Eswatini Red Cross Society 2018 ANNUAL REPORT Baphalali demonstrates to a drought hit Lavumisa, Etjeni Chiefdom Community member on how to practice conservation agriculture (CA) using a seed driller. Photographer: BERCS Communications Department Mission: Saving lives, changing minds Mission: Saving lives, changing minds ii TABLE OF CONTENTS TABLE OF CONTENTS .................................................................................................................................... II PRESIDENT’S REMARKS ................................................................................................................................ 1 SECRETARY GENERAL’S SUMMARY ......................................................................................................... 4 INTRODUCTION ................................................................................................................................................ 5 ACHIEVEMENTS ............................................................................................................................................... 5 1.0 HEALTH AND SOCIAL SERVICES ................................................................................................... 5 1.1 PRIMARY HEALTH CARE: MOTHER, INFANT, CHILD HEALTH, CURATIVE, AND HIV/TB . 5 2.0 FIRST AID .............................................................................................................................................. -
Reduction of Drought Vulnerabilities in Southern Swaziland Final Report | September 2012
Reduction of Drought Vulnerabilities in Southern Swaziland Final Report | September 2012 Cooperative agreement number DFD-G -00-09-00136-00 Start date APRIL 9, 2009 Program duration 3 YEARS Country SWAZILAND Donor budget US$ 4,998,945 Time period covered by this report APRIL 2009 – JUNE 2012 Number of individuals affected in target area 88,605 (SVAC, 2010) Number of individual beneficiaries targeted 61,370 Number of individual IDP beneficiaries targeted 0 ACRONYMS CA Conservation Agriculture DHS Demographic Health Survey EOP End of Project (endline survey) HH Household IRD International Relief and Development MT Metric Tonne OFDA Office for Foreign Disaster Assistance PTA Parent Teacher Association UN United Nations USAID US Agency for International Development VAC Vulnerability Assessment Committee WFP World Food Programme USAID/OFDA Reduction of Drought Vulnerabilities in Southern Swaziland | FINAL REPORT | 26 September 2012 | 1 Executive Summary IRD implemented a three year program (2009-2012) whose goal was “to reduce vulnerability to drought of households and communities in the Lowveld Agro-ecological zone of Swaziland” targeting 61,370 beneficiaries in the Shiselweni and Lubombo areas of the Lowveld region. This region was targeted because it covers 31% of the country and has a semiarid climate with an average annual precipitation between 400mm and 800mm, which makes it very difficult to grow crops without a moisture conservation plan. This report covers the activities conducted under the umbrella of two primary sectors, which were the focus of the 2009- 2012 IRD Swaziland’s program areas: 1. Agriculture and Food Security Objective: to improve agricultural practices under drought conditions; 2. -

Swaziland Government Gazette Extraordinary
Swaziland Government Gazette Extraordinary VOL. XLVI] MBABANE, Friday, MAY 16th 2008 [No. 67 CONTENTS No. Page PART C - LEGAL NOTICE 104. Registration Centres For the 2008 General Elections................................................... SI PUBLISHED BY AUTHORITY 442 GENERAL NOTICE NO. 25 OF 2008 VOTERS REGISTRATION ORDER, 1992 (King’s Order in Council No.3 of 1992) REGISTRATION CENTRES FOR THE 2008 GENERAL ELECTIONS (Under Section 5(4)) Short title and commencement (1) This notice shall be cited as the Registration Centres Notice, 2008. (2) This general notice shall come into force on the date of publication in the Gazette. Registration centres for the 2008general elections It is notified for general information that the registration of all eligible voters for the 2008 general elections shall be held at Imiphakatsi (chiefdoms) and at the registration centres that have been listed in this notice; REGISTRATION CENTRES HHOHHO REGION CODE CODE CODE CHIEFDOM / POLLING Sub polling REGION INKHUNDLA STATION station 01 HHOHHO 01 HHUKWINI 01 Dlangeni 01 HHOHHO 01 HHUKWINI 02 Lamgabhi 01 HHOHHO 02 LOBAMBA 01 Elangeni 01 HHOHHO 02 LOBAMBA 02 Ezabeni 01 HHOHHO 02 LOBAMBA 03 Ezulwini 01 HHOHHO 02 LOBAMBA 04 Lobamba 01 HHOHHO 02 LOBAMBA 05 Nkhanini 01 HHOHHO 03 MADLANGEMPISI 01 Buhlebuyeza 01 HHOHHO 03 MADLANGEMPISI 02 KaGuquka 01 HHOHHO 03 MADLANGEMPISI 03 Kuphakameni/ Dvokolwako 01 HHOHHO 03 MADLANGEMPISI 04 Mzaceni 01 HHOHHO 03 MADLANGEMPISI 05 Nyonyane / KaMaguga 01 HHOHHO 03 MADLANGEMPISI 06 Zandondo 01 HHOHHO 04 MAPHALALENI 01 Edlozini 443 -

The Kingdom of Swaziland
THE KINGDOM OF SWAZILAND MASTERPLAN TOWARDS THE ELIMINATION OF NEGLECTED TROPICAL DISEASES - 2015- 2020 Foreword Acknowledgements Table of Contents .......................................................................................................................................... 1 LIST OF TABLES .................................................................................................................. 5 PART 1: SITUATION ANALYSIS ....................................................................................... 10 1.1 Country profile ......................................................................................................... 10 1.1.1 Geographical characteristics ............................................................................... 10 1.1 .2 PHYSICAL FEATURES AND CLIMATIC CONDITIONS ....................................... 11 1.1.3. ADMINISTRATIVE STRUCTURES, DEMOGRAPHY AND COMMUNITY STRUCTURES ................................................................................................................... 12 1.3.2 Population ............................................................................................................. 13 Health Information System ........................................................................................... 25 Health workforce ........................................................................................................... 26 Medical products .......................................................................................................... -
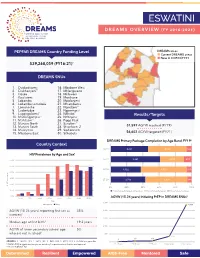
DREAMS Fact Sheet ESWATINI
ESWATINI DREAMS OVERVIEW (fy 2016-2021) PEPFAR DREAMS Country Funding Level DREAMS areas Current DREAMS areas New in COP20/FY21 $39,268,059 (FY16-21)* DREAMS SNUs 1. Dvokodvweni 16. Mbabane West 2. Ekukhanyeni** 17. Mhlangatane 3. Hosea 18. Mkhiweni 4. Kwaluseni 19. Motshane 5. Lobamba 20. Mpolonjeni 6. Lobamba Lomdzala 21. Mtsambama 7. Lomahasha 22. Ngudzeni** 8. Ludzeludze 23. Ngwempisi 9. Lugongolweni** 24. Nkhaba** Results/Targets 10. Madlangampisi** 25. Ntfonjeni 11. Mafutseni** 26. Piggs Peak ** 12. Manzini North 27. Sandleni 5 13. Manzini South 28. Shiselweni 2 31,597 AGYW reached (FY19) 14. Maseyisini 29. Siphofaneni * 15. Mbabane East 30. Sithobela 56,602 AGYW targeted (FY21) DREAMS Primary Package Completion by Age Band, FY195 Country Context 10-14 4,031 4,044 566 HIV Prevalence by Age and Sex1 15-19 60.0% 5,281 2,507 857 50.0% 20-24 3,022 4,515 510 40.0% 30.0% 25-29 2,712 3,208 344 20.0% HIV Prevalence HIV 0% 20% 40% 60% 80% 100% 10.0% Primary Package Completed and Secondary Primary Package Completed Primary Package Incomplete 0.0% 5 10-14 15-19 20-24 25-29 30-34 35-39 40-44 45-49 AGYW (15-24 years) Initiating PrEP in DREAMS SNUs Age 5,000 Female Male 4,755 AGYW (18-24 years) reporting first sex as 35% 4,000 coerced2 3,000 Median age at first birth3 19.2 years 2,000 AGYW of lower secondary school age 5% 4 who are not in school 1,000 704 1 99 108 SOURCES: 1. -

Download 2018 National Elections-Winners
2018 NATIONAL ELECTIONS - WINNERS LIST OF TINDVUNA TETINKHUNDLA (2018) HHOHHO REGION INKHUNDLA NAME OF OFFICER HHUKWINI Mkhabela Titus F LOBAMBA Bhembe Bhekisisa A MADLANGEMPHISI Maseko Aron M MAPHALALENI Dlamini Gabangani MAYIWANE Dlamini Hhohho MBABANE EAST Mavuso Mefika MBABANE WEST Dlamini Mlondi MHLANGATANE Vilakati Gcinile T MOTSHANE Shongwe Nigel T NDZINGENI Mvila Fikelephi Lakhatsidze NKHABA Dlamini Shege NTFONJENI Dlamini Olga Cebile PIGG’S PEAK Matsebula Lucky M SIPHOCOSINI Mavimbela Gcinumuzi TIMPHISINI Mndazwe Sipho 2018 NATIONAL ELECTIONS - WINNERS LIST OF MEMBERS OF PARLIAMENT (2018) HHOHHO REGION INKHUNDLA NAME OF OFFICER HHUKWINI Ngwenya Nkhanyeti C. LOBAMBA Betram Allen Stewart MADLANGEMPHISI Nxumalo Sibusiso S MAPHALALENI Maseko Mabulala MAYIWANE Dlamini Gcina S MBABANE EAST Bulunga Harries M MBABANE WEST Zwane Musa Z.Z MHLANGATANE Mhlanga Madala MOTSHANE Magongo Robert M NDZINGENI Lutfo Dlamini NKHABA Magongo Zakhele NTFONJENI Magagula Sifiso PIGG’S PEAK Jabulani Clement Mabuza SIPHOCOSINI Matsebula Mduduzi Mlondi TIMPHISINI Mamba Nelson REGIONAL WOMAN MEMBER Bujela Nokunceda 2018 NATIONAL ELECTIONS - WINNERS LIST OF TINDVUNA TETINKHUNDLA (2018) LUBOMBO REGION INKHUNDLA NAME OF OFFICER DVOKODVWENI Dlamini Mayibongwe GILGAL Robert Nyawo LOMAHASHA Mphaphu Nkosingiphile LUBULINI Manesi Dlamini LUGONGOLWENI Phindile Felicia Shongwe MATSANJENI – NORTH Thandiwe F.Ndzimandze MHLUME Dlamini Morris Hlalangenkhani MPOLONJENI Thulani City Dlamini NKILONGO Sandziso Mamba SIPHOFANENI Mzimela Nhlanhla Simelane SITHOBELA Fanyana Joel -

Original Research Article Open Access
Available online at http://www.journalijdr.com ISSN: 2230-9926 International Journal of Development Research Vol. 09, Issue, 06, pp. 28352-28357, June, 2019 REVIEW ARTICLE ORIGINAL RESEARCH ARTICLE OPEN ACCESS DETERMINATION OF DDT AND ITS METABOLITE IN MARULA PRODUCTS IN ESWATINI USING A MOLECULAR IMPRINTED POLYMER *Sithole Nothando Beautiness, Thwala Justice Mandla and Bwembya Gabriel Chewe University of Eswatini, Department of Chemistry, Kwaluseni, Eswatini ARTICLE INFO ABSTRACT Article History: Dichlorodiphenyltrichloroethane (DDT) is an effective organochlorine pesticide which is used in Received 25th March, 2019 Indoor Residual Spraying (IRS) in Eswatini yet it is toxic, susceptible to long range Received in revised form environmental transport and bio-accumulate in fatty tissues. The main objective was to quantify 22nd April, 2019 the amount of DDT and its metabolites (DDE and DDD) in Marula brew and kernels. The Accepted 21st May, 2019 samples were pre-extracted with acetonitrile, extracted using a periodic mesoporousorganosilica th Published online 30 June, 2019 molecular imprinted polymer (PMO-MIP) with acetone in cyclohexane and then analyzed with GC/ECD. DDT was detectedin 88% of the samples with the highest concentrations at 0.903 ppm Key Words: in brew and 148.686 mg/kg from the kernels. DDD was detected in 86% of the Marula brew DDT, marula products, samples with the highest concentration at 0.483 ppm and 68.219 mg/kg from the kernels. mesoporous, organosilica, imprinted, polymer However, DDE was found in lower concentrations of 0.138 ppm and 30.132 mg/kg from the brew and residual. and kernels respectively. The study concluded that people and animals are at risk of DDT residual accumulation as 98% of the samples collected had the analytes detected at level above the WHO safety limit of 0.05 ppm. -

SWAZILAND Vulnerability Assessment Committee Results 2015
SWAZILAND Vulnerability Assessment Committee Results 2015 Regional Socio - Economic Context Population at risk of food and livelihoods insecurity trend Malnutrition Rates (%) 2014/15 Population 1,12 million people Stunting Underweight Wasting Life expectancy 47.8 years 262,000 223,249 28.7 31 Population Growth Rate 1.0% 160,989 201,000 29 115,713 Human Development Index 0.148 (2013) 88,511 25.5 Adult Literacy 87.8% (2012) Employment Rate 71.9% (2014) Average GDP Growth 2.3% (2013) 2009/10 2010/11 2011/12 2012/13 2013/14 2014/15 Under 5 Mortality Rate 67 per 1,000 live births May 2015 to April 2016 Projected Livelihood Outcomes 9.6 Inflation 5.70% (2015, CSO) 5.8 HIV and AIDS 26.0% (2009) Timphisini Proportion of Children (%) 5.4 5.8 Ntfonjeni Mayiwane 2.5 2 1.2 0.8 Objectives of Assessment 2014/15 Mhlangatane Pigg's Peak 2000 2007 2010 2014 • To assess the status of livelihoods and vulnerability in rural households and provide timely Ndzingeni information for programming and decision making. 201,000 Lomahasha population at risk of food • To understand the different capabilities (assets) of households to cope with crises such as Mandlangempisi Mhlume Key Recommendations and livelihoods Nkhaba droughts, floods, economic fluctuations, plant or animal pests and diseases. • Crop diversification (not only maize) especially in the Lubombo region and production of insecurity Maphalaleni • Use the Household Economy Approach to get the numbers of people food insecure for the drought resistant crops in this region. consumption period 2015-2016. Mbabane Mkhiweni Hlane • Use of the existing irrigation infrastructure for sugar cane plantations.