Independent Final Evaluation Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
1 Sindh Flood Response 2011 FINAL REPORT
Sindh Flood Response 2011 FINAL REPORT (OCT 18, 2011 – FEB 29, 2012) AID-OFDA-G-12-00003 Funded by: United States Agency for International Development Office of Foreign Disaster Assistance USAID/OFDA Organization: Mercy Corps Date: May 31, 2011 HQ Address: 45 SW Ankeny St Portland, OR, 97204, USA USA Pakistan Peter O'Farrell Steve Claborne, Country Director Senior Program Officer, South Asia Tel: (92) 300-501-2340 Tel.: (1) 503-896-5849 E-mail : [email protected] Fax: (1) 503-896-5013 House #36, Street #1, F/6-3 Email: [email protected] Islamabad, Pakistan Country/Region: Pakistan, Districts Badin and Mirpur Khas in Southern Sindh. Mercy Corps, Pakistan ͳ EXECUTIVE SUMMARY The monsoon rains that started in the second week of August 2011 triggered serious flooding affecting more than 5.3 million people. It is reported to have destroyed or damaged nearly one million houses and inundated 4.2 million acres of cropland, prompting the Government of Pakistan to call for support from the United Nations. The National Disaster Management Authority (NDMA) and the Provincial Disaster Management Authority (PDMA) for Sindh mobilized its resources relatively quickly, however their response was far too limited compared with the needs of so many people. During the contingency planning phase, they estimated resources adequate to the temporary care of some 50,000 IDPs. The situation had worsened nearly a month after the start of the emergency and the national authorities requested international support. At that point, the NDMA and PDMA indicated that between 5.3 million flood-affected people of Lower Sindh were in urgent need of assistance. -

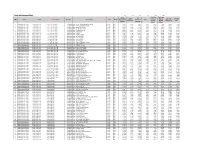
Final Merit List of Candidates Applied for Admission in Bs Medical Laboratory
BS MEDICAL LABORATORY TECHNOLOGY (BSMLT) SESSION - 2020-2021 FINAL MERIT LIST OF CANDIDATES APPLIED FOR ADMISSION IN BS MEDICAL LABORATORY TECHNOLOGY (BSMLT) SESSION 2020-2021 LIAQUAT UNIVERSITY OF MEDICAL & HEALTH SCIENCES, JAMSHORO DISTRICT - BADIN (BS MEDICAL LABORATORY TECHNOLOGY (BSMLT) - 01 - SEAT - MERIT) Test Test Int. Total Merit Inter A / Level Test Form No. Name of Candidates Fathers Name Surname Gender DOB District Seat Marks 50% score Positon Obt 50% Year Inter% Grade No. Marks 1 4841 Habesh Kumar Veero Mal Khattri Male 1/11/2001 BADIN 2019 905 82.273 A1 719 82 41 41.136 82.136 District: BADIN - WAITING Menghwar 1496 Akash Kumar Mansingh Male 10/16/2001 BADIN 2020 913 83 A1 167 78 39 41.5 80.5 2 Bhatti 3 1215 Janvi Papoo Kumar Lohana Female 2/11/2002 BADIN 2020 863 78.455 A 894 82 41 39.227 80.227 4 3344 Bushra Muhammad Ayoub Kamboh Female 9/30/2000 BADIN 2019 835 75.909 A 490 82 41 37.955 78.955 5 1161 Chanderkant Papoo Kumar Lohana Male 3/8/2003 BADIN 2020 889 80.818 A1 503 76 38 40.409 78.409 6 3479 Bushra Amjad Amjad Ali Jat Female 4/20/2001 BADIN 2019 848 77.091 A 494 73 36.5 38.545 75.045 7 4306 Noor Ahmed Ghulam Muhammad Notkani Male 10/12/2001 BADIN 2020 874 79.455 A 1575 70 35 39.727 74.727 Muhammad Talha 2779 Hasan Nasir Rajput Male 7/21/2001 BADIN 2020 927 84.273 A1 1378 65 32.5 42.136 74.636 8 Nasir 9 3249 Vandna Dev Anand Lohana Female 3/21/2002 BADIN 2020 924 84 A1 2294 65 32.5 42 74.5 10 2231 Sanjai Eshwar Kumar Luhano Male 8/17/2000 BADIN 2020 864 78.546 A 1939 70 35 39.273 74.273 RANA RAJINDAR 3771 RANA AMAR -
Tando Muhammad Khan
Tando Muhammad Khan 475 476 477 478 479 480 Travelling Stationary Inclass Co- Library Allowance (School Sub Total Furniture S.No District Teshil Union Council School ID School Name Level Gender Material and Curricular Sport Laboratory (School Specific (80% Other) 20% supplies Activities Specific Budget) 1 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010002 GBPS - YAR M. KANDRA@PIR BUX KANDRA Primary Boys 9,117 1,823 7,294 1,823 1,823 7,294 29,175 7,294 2 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010016 GBPS - YAR MUHAMMAD KANDRA Primary Boys 11,323 2,265 9,058 2,265 2,265 9,058 36,233 9,058 3 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010017 GBPS - KHUDA BUX GUMB Primary Boys 14,353 2,871 11,482 2,871 2,871 11,482 45,929 11,482 4 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010022 GBPS - ALAM KHAN TALPUR Primary Boys 44,542 8,908 35,634 8,908 8,908 35,634 142,535 35,634 5 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010025 GBPS - PALIO GHUMRANI Primary Boys 28,220 5,644 22,576 5,644 5,644 22,576 90,303 22,576 6 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010026 GBPS - KARIMABAD Primary Boys 28,690 5,738 22,952 5,738 5,738 22,952 91,808 22,952 7 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. -

Historical Sketch of Peasant Activism: Tracing Emancipatory Political Strategies of Peasant Activists of Sindh
International Journal Humanities and Social Sciences (IJHSS) ISSN (P): 2319-393X; ISSN(E): 2319-3948 Vol. 3, Issue 5, Sep 2014, 23-42 © IASET HISTORICAL SKETCH OF PEASANT ACTIVISM: TRACING EMANCIPATORY POLITICAL STRATEGIES OF PEASANT ACTIVISTS OF SINDH GHULAM HUSSAIN 1 & ANWAAR MOHYUDDIN 2 1MPhil Scholar, Department of Anthropology, Quaid-i-Azam University, Islamabad, Pakistan 2 Lecturer, Department of Anthropology, Quaid-i-Azam University, Islamabad, Pakistan ABSTRACT Peasant activism in Sindh is very diverse and has its own typical history. Temporally, it has been focused on contextual issues that demand more than just land reforms. Peasant activists have, over the years, pursued roughly articulated, expedient and highly diverse agendas that are enacted by the mix of civil society activists, NGOs and ethnic peasant activists. In this article, which is the result of ethnographic study and the analysis of secondary ethnographic and historical data, effort has been made to trace the formation of peasantivist agendas and strategies in Sindh, particularly tracing it from the peasant struggle of Shah Inayat in 17 th century. The introduction of exploitative Batai system during British rule, the consequent institutionalization of sharecropping, establishment of Hari Committee in 1930s, the launching of Batai Tehreek and Elati Tehreek have been traced in relation to shifting peasantivist agendas. Failure of peasant activists to bring about substantive land reforms and the recent process of NGO-ising of peasant activism, have been analyzed vis-à-vis historical past. KEYWORDS: Peasant Activism, Peasant Movements, N.G.Os INTRODUCTION In this study the genesis of exploitation in peasant communities of Sindh has been elaborated, and the historical analysis of some of the important peasant struggles, rebels, and movements have been done to understand where peasants and peasant activist in Sindh stands now. -

The Rise of Dalit Peasants Kolhi Activism in Lower Sindh
The Rise of Dalit Peasants Kolhi Activism in Lower Sindh (Original Thesis Title) Kolhi-peasant Activism in Naon Dumbālo, Lower Sindh Creating Space for Marginalised through Multiple Channels Ghulam Hussain Mahesar Quaid-i-Azam University Department of Anthropology ii Islamabad - Pakistan Year 2014 Kolhi-Peasant Activism in Naon Dumbālo, Lower Sindh Creating Space for Marginalised through Multiple Channels Ghulam Hussain Thesis submitted to the Department of Anthropology, Quaid-i-Azam University Islamabad, in partial fulfillment of the degree of ‗Master of Philosophy in Anthropology‘ iii Quaid-i-Azam University Department of Anthropology Islamabad - Pakistan Year 2014 Formal declaration I hereby, declare that I have produced the present work by myself and without any aid other than those mentioned herein. Any ideas taken directly or indirectly from third party sources are indicated as such. This work has not been published or submitted to any other examination board in the same or a similar form. Islamabad, 25 March 2014 Mr. Ghulam Hussain Mahesar iv Final Approval of Thesis Quaid-i-Azam University Department of Anthropology Islamabad - Pakistan This is to certify that we have read the thesis submitted by Mr. Ghulam Hussain. It is our judgment that this thesis is of sufficient standard to warrant its acceptance by Quaid-i-Azam University, Islamabad for the award of the degree of ―MPhil in Anthropology‖. Committee Supervisor: Dr. Waheed Iqbal Chaudhry External Examiner: Full name of external examiner incl. title Incharge: Dr. Waheed Iqbal Chaudhry v ACKNOWLEDGEMENT This thesis is the product of cumulative effort of many teachers, scholars, and some institutions, that duly deserve to be acknowledged here. -
![[Jan-Mar.'2006] Awareness / Disclosure](https://docslib.b-cdn.net/cover/0740/jan-mar-2006-awareness-disclosure-680740.webp)
[Jan-Mar.'2006] Awareness / Disclosure
Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized PREFACE The report in hand is the Final (updated October 2006) of the Integrated Social & Environmental Assessment (ISEA) for proposed Water Sector Improvement Project (WSIP). This report encompasses the research, investigations, analysis and conclusions of a study carried out by Mls Osmani & Co. (Pvt.) Ltd., Consulting Engineers for the Institutional Reforms Consultant (IRC) of Sindh Irrigation & Drainage Authority (SIDA). The Proposed Water Sector Improvement Project (WSIP) Phase-I, being negotiated between Government of Sindh and the World Bank entails a number of interventions aimed at improving the water management and institutional reforms in the province of Sindh. The second largest province in Pakistan, Sindh has approx. 5.0 Million Ha of farm area irrigated through three barrages and 14 canals. The canal command areas of Sindh are planned to be converted into 14 Area Water Boards (AWBs) whereby the management, operations and maintenance would be carried out by elected bodies. Similarly the distributaries and watercourses are to be managed by Farmers Organizations (FOs) and Watercourse Associations (WCAs), respectively. The Project focuses on the three established Area Water Boards (AWBs) of Nara, Left Bank (Akram Wah & Phuleli Canal) & Ghotki Feeder. The major project interventions include the following targets:- * Improvement of 9 main canals (726 Km) and 37 branch canals (1,441 Km). This includes new lining of 50% length of the lined reach of Akram Wah. * Control of Direct Outlets * Replacement of APMs with agreed type of modules * Improvement of 173 distributaries and minor canals ( 1527 Krn) including 145 Km of geomembrane lining and 1 12 Km of concrete lining in 3 AWBs. -

SEF Middle-High School Program (SMHSP)
Sindh Education Foundation, Govt. of Sindh SEF Middle/High School Schools (103) SN School Code Level Village Union Council Taluka District Operator Operator Contact Nd Nm Ns Ed Em Es 1 SMHS0074 Middle/High MIR KHAN MEHAR KURKELI SINJHORO SANGHAR (AMRDF) AL-MEHRAN RESEARCH0301-3813519 AND DEVELOMENT FOUNDATION25 59 477 68 51 385 2 SMHS0075 Middle/High MUHAMMAD URS BROHI KURKELI SINJHORO SANGHAR (AMRDF) AL-MEHRAN RESEARCH0301-3813519 AND DEVELOMENT FOUNDATION25 59 241 68 47 416 3 SMHS0076 Middle/High SIJHORO ROYAL CITY SINJHORO SINJHORO SANGHAR (AMRDF) AL-MEHRAN RESEARCH0301-3813519 AND DEVELOMENT FOUNDATION25 01 970 68 48 530 4 SMHS0077 Middle/High NAO MAIL SAYED MATTO SHAH BULRI SHAH KARIM T-M KHAN ABDUL WAHID KHOSO 0333-2656882 25 02 225 68 26 101 5 SMHS0078 Middle/High SHER M.LANGHA LAKHAT T-M KHAN T-M KHAN ABDUL WAHID KHOSO 0333-2656882 25 03 490 68 30 389 6 SMHS0044 Middle/High CHANNA MUHALLA GUJJO KHAIRPUR KHAIRPUR AHSAN ALI CHANDIO 0301-3680745 27 32 574 68 44 397 7 SMHS0040 Middle/High MEHRAN COLONY NOSHERO FEROZ NOSHERO FEROZ N-FEROZ AKBAR ALI SOOMRO 0300-8101611 26 51 195 68 07 298 8 SMHS0041 Middle/High Daro UC-4 DADU DADU AKBAR ALI SOOMRO 0300-8101611 26 44 104 67 46 379 9 SMHS0079 Middle/High VILLAGE DALAIL SHAR TORI MORIKOT NAWAB SANGHAR SANGHAR ALI DINO 0333-2912090 26 00 209 69 02 072 10 SMHS0080 Middle/High MIAN MIAN SANGHAR SANGHAR ALI DINO 0333-2912090 DNA DNA DNA DNA DNA DNA 11 SMHS0081 Middle/High CHEEHO CHEEHO NOSHERO FEROZ N-FEROZ ALI EDUCATION AND WELFARE3003640795 SOCIETY 26 47 365 68 14 490 12 SMHS0082 Middle/High -

Controlled Growth of Zinc Oxide Nanowire Arrays by Chemical Vapor Deposition (CVD) Method
IJCSNS International Journal of Computer Science and Network Security, VOL.19 No.8, August 2019 135 Controlled Growth of Zinc Oxide Nanowire Arrays by Chemical Vapor Deposition (CVD) Method Waseem A. Bhutto1, Abdul Majid Soomro1, Altaf H. Nizamani1, Hussain Saleem2*, Murad Ali Khaskheli1, Ali Ghulam Sahito3, Roshan Das1, Usman Ali Khan1, Samina Saleem2,4 1Institute of Physics, University of Sindh, Jamshoro, Pakistan. 2Department of Computer Science, UBIT, University of Karachi, Karachi, Pakistan. 3Centre for Pure & Applied Geology, University of Sindh, Jamshoro, Pakistan. 4Karachi University Business School, KUBS, University of Karachi, Pakistan. *Corresponding Author: [email protected] Abstract The Nanostructured materials like nanotubes, nanowires, sensors [11], Resistive-switching Random Access Memory nanorods, and nanobelts etc. have remained the subject of interest (RRAM) [12][13], nano-generators [14][15], nano- these days because of its unique thermal, mechanical and optical capacitors [16], and gas sensors [17][18]. properties. Zinc Oxide (푍푛푂), is the most attractive material due to its unique properties and availability of a variety of growth The performance of 푍푛푂 based devices strongly depend methods. At nanostructured level, the properties of 푍푛푂 can be on their dimensions and morphologies [19][20][21][22][23] altered by controlling the growth process, such as the shape, size, [24][25][26]. Therefore, the investigation of 푍푛푂 nano- morphology, aspect ratio and density control. In this work, structures in highly oriented, aligned and ordered arrays is of Aligned 푍푛푂 Nanowires (NWs) were successfully synthesized by critical importance for the development of novel devices. Chemical Vapor Deposition (CVD) on Aluminum doped Zinc Different methods have been used to synthesize 푍푛푂 Oxide (AZO) substrate. -

Provisional Seniority List of Bs-20 Officers of Pakistan Administrative Service (Pas)
A GOVERNMENT OF PAKISTAN •CABINET SECRETARIAT ESTABLISHMENT DIVISION No. 3/1 /2006-CP-6(130 Islamabad the 27th March, 2019 CIRCULAR Subject:- PROVISIONAL SENIORITY LIST OF BS-20 OFFICERS OF PAKISTAN ADMINISTRATIVE SERVICE (PAS) A provisional seniority list of BS-20 officers of Pakistan Administrative Service (PAS), as on 25-03-2019 has been prepared in accordance with the relevant rules and circulated for perusal/information of all concerned. 2. Objections, if any, duly supported with documentary evidence, may please be sent within 15 days from the date of issuance of this circular. The objections received thereafter, will not be entertained and the list will be finalized. 3. This . provisional seniority list issues with the approval of Secretary Establishment Division. Ends: (as above) (Ali Anan Qamar) Deputy Secretary (CP-I) 051-9205748 Distribution:- All concerned officers. „ Chief Secretary, Punjab/Sindh/KP/Balochistan/G.B. with request to distribute the Seniority List to all concerned officers working under their administration. Copy for information to:- Joint `..;ecretary listablishment Di \ ision. Islamabad. ii) Director (11). Establishment Division. Islamabad with request to place it on the \vebsite of Establishment Division. iii) Director (PD), Establishment Division, Islamabad. iv) Section Officer (E-5), Establishment Division, Islamabad. v) P.S. to Additional Secretary-II, Establishment Division, Islamabad. vi) P.S. to Secretary, Establishment Division, Islamabad. PROVISIONAL SENIORITY LIST OF OFFICERS OF PAS/BS-20 S• Date of Date of Joining Names of Officers Domicile No. Birth . PAS/ Present Rank . apt. (Retd) Muhammad Tariq 19-07-1959 KPK 22-10-1985 Hayat 23-09-2008 2. Mr. Ahmad Bakhsh Narejo 12-01-1964 Sindh-R 14-11-1987 07-03-2008 3. -

In the High Court of Sindh, Karachi
[1] IN THE HIGH COURT OF SINDH, KARACHI C.P.No.D-2186 of 2021 Date Order with signature of Judge(s) Before: Mr. Justice Nazar Akbar Mr. Justice Muhammad Faisal Kamal Alam --------------------------------------------------------------------- Petitioner : Zabardast Khan Mahar, through Mr. Waqar Alam Abbasi, Advocate. Versus Respondent No.1 : The Federation of Pakistan Respondent No.2 : The Director General NAB, Sukkur. Date of Hearing : 05.04.2021 O R D E R NAZAR AKBAR, J:- The Petitioner has sought the following relief(s) through this petition: i. To reduce the surety amount to a reasonable and just sum to enunciate that the grant of bail is a form of relief and not a method of punishment as observed by the Hon'ble Supreme Court of Pakistan as well. ii Any other relief(s) which this Hon'ble Court deems fit and pr0per may kindly be granted. 2. On query from the Court, learned counsel for the Petitioner was unable to satisfy the Court that how an independent/fresh constitution petition can be filed when the Petitioner is aggrieved by an order passed by this very Bench in C.P No.D-1078/2020, whereby the said petition was disposed of. In the first place if the Petitioner was aggrieved by any observation, he should have filed petition for leave to appeal before Hon'ble Supreme Court. Additionally, this petition is not maintainable also for the following reasons: (i) This petition has not been signed and supported with the affidavit of the Petitioner. [2] (ii) Office objection No.7 that affidavit of Petitioner in support of petition is to be filed/sworn has not been properly answered by the Petitioner. -

Bonded Labour in Agriculture: a Rapid Assessment in Sindh and Balochistan, Pakistan
InFocus Programme on Promoting the Declaration on Fundamental Principles WORK IN FREEDOM and Rights at Work International Labour Office Bonded labour r in agriculture: e a rapid assessment p in Sindh and Balochistan, a Pakistan P Maliha H. Hussein g Abdul Razzaq Saleemi Saira Malik Shazreh Hussain n i k r Special Action Programme to Combat Forced Labour o DECLARATION/WP/26/2004 ISBN 92-2-115484-X W WP. 26 Working Paper Bonded labour in agriculture: a rapid assessment in Sindh and Balochistan, Pakistan by Maliha H. Hussein Abdul Razzaq Saleemi Saira Malik Shazreh Hussain International Labour Office Geneva March 2004 Foreword In June 1998 the International Labour Conference adopted a Declaration on Fundamental Principles and Rights at Work and its Follow-up that obligates member States to respect, promote and realize freedom of association and the right to collective bargaining, the elimination of all forms of forced or compulsory labour, the effective abolition of child labour, and the elimination of discrimination in respect of employment and occupation.1 The InFocus Programme on Promoting the Declaration is responsible for the reporting processes and technical cooperation activities associated with the Declaration; and it carries out awareness raising, advocacy and research – of which this Working Paper is an example. Working Papers are meant to stimulate discussion of the questions covered by the Declaration. They express the views of the author, which are not necessarily those of the ILO. This Working Paper is one of a series of Rapid Assessments of bonded labour in Pakistan, each of which examines a different economic sector. -

Government of Sindh Finance Department
2021-22 Finance Department Government of Sindh 1 SC12102(102) GOVERNOR'S SECRETARIAT/ HOUSE Rs Charged: ______________ Voted: 51,652,000 ______________ Total: 51,652,000 ______________ ____________________________________________________________________________________________ GOVERNOR'S SECRETARIAT ____________________________________________________________________________________________ BUILDINGS ____________________________________________________________________________________________ P./ADP DDO Functional-Cum-Object Classification & Budget NO. NO. Particular Of Scheme Estimates 2021 - 2022 ____________________________________________________________________________________________ Rs 01 GENERAL PUBLIC SERVICE 011 EXECUTIVE & LEGISLATIVE ORGANS, FINANCAL 0111 EXECUTIVE AND LEGISLATIVE ORGANS 011103 PROVINCIAL EXECUTIVE KQ5003 SECRETARY (GOVERNOR'S SECRETARIAT/ HOUSE) ADP No : 0733 KQ21221562 Constt. of Multi-storeyed Flats Phase-II at Sindh Governor's 51,652,000 House, Karachi (48 Nos.) including MT-s A12470 Others 51,652,000 _____________________________________________________________________________ Total Sub Sector BUILDINGS 51,652,000 _____________________________________________________________________________ TOTAL SECTOR GOVERNOR'S SECRETARIAT 51,652,000 _____________________________________________________________________________ 2 SC12104(104) SERVICES GENERAL ADMIN & COORDINATION Rs Charged: ______________ Voted: 1,432,976,000 ______________ Total: 1,432,976,000 ______________ _____________________________________________________________________________