Original Article Endogenous Risk Factors for Deep-Vein Thrombosis in Patients with Acute Spinal Cord Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Activated Protein C Resistance: the Most Common Risk Factor for Venous Thromboembolism
J Am Board Fam Pract: first published as 10.3122/15572625-13-2-111 on 1 March 2000. Downloaded from CLINICAL REVIEW Activated Protein C Resistance: The Most Common Risk Factor for Venous Thromboembolism Dawn R. Sheppard, DO Background: Venous thromboembolism is a major cause of morbidity and mortality. Although activated protein C resistance (APC-R) is the most commonly recognized inherited risk factor for venous throm boembolism, little is known about its long-tenn implications on health. Methods: MEDLINE was searched from January 1989 through August 1999 using the key words ''thromboembolism," ''thrombosis," "activated protein C resistance," and "factor V Leiden." Results: One in 1000 people in the United States is affected by venous thromboembolism annually. APC-R is now understood to be responsible for up to 64% of these cases. APC-R, which occurs widely in some ethnic groups and is nearly absent in others, is due to a single point mutation in the gene for clot ting factor V. As a result, inactivation of factor V by activated protein C is impaired, leading to a hyper coagulable state. This condition creates a lifelong increased risk of thrombosis and, possibly, anticoag- ulant therapy.. Conclusion: Family physicians have a new tool for assessing risks for venous thromboembolism. Recognizing that up to 64% of patients with venous thromboembolism can have APe-R and treating this disorder with prophylactic and therapeutic anticoagulation might reduce patient morbidity and mortal ity from venous thromboembolism. Screening high-risk patients might now be indicated. (J Am Board Fam Pract 2000i13:111-5.) Venous thromboembolism, a serious health prob "thromboembolism," "thrombosis," "activated pro lem and an important cause of morbidity, affects tein C resistance," and "factor V Leiden." about 1 in 1000 persons annually. -
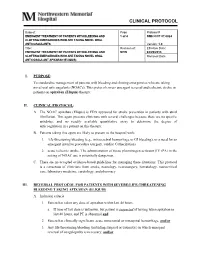
Clinical Protocol
CLINICAL PROTOCOL Subject: Page Protocol # EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND 1 of 4 NMH CCP 07.0024 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL ANTICOAGULANTS Version: 1.0 Title: Revision of: Effective Date: EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND NEW 04/29/2013 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL Removal Date: ANTICOAGULANT APIXABAN (ELIQUIS) I. PURPOSE: To standardize management of patients with bleeding and clotting emergencies who are taking novel oral anticoagulants (NOACs). This protocol covers emergent reversal and ischemic stroke in patients on apixaban (Eliquis) therapy. II. CLINICAL PROTOCOL: A. The NOAC apixaban (Eliquis) is FDA approved for stroke prevention in patients with atrial fibrillation. This agent presents clinicians with several challenges because there are no specific antidotes, and no readily available quantitative assay to determine the degree of anticoagulation in a patient on this therapy. B. Patients taking this agent are likely to present to the hospital with; 1. life-threatening bleeding (e.g., intracerebral hemorrhage or GI bleeding), or a need for an emergent invasive procedure (surgery, cardiac Catherization) 2. acute ischemic stroke. The administration of tissue plasminogen activator (IV tPA) in the setting of NOAC use is potentially dangerous. C. There are no accepted evidence-based guidelines for managing these situations. This protocol is a consensus of clinicians from stroke, neurology, neurosurgery, hematology, neurocritical care, laboratory medicine, cardiology, and pharmacy. III. REVERSAL PROTOCOL FOR PATIENTS WITH SEVERE/LIFE-THREATENING BLEEDING TAKING APIXABAN (ELIQUIS) A. Inclusion criteria: 1. Patient has taken any dose of apixaban within last 48 hours. a. If time of last dose is unknown, but patient is suspected of having taken apixaban in last 48 hours, and PT is abnormal and 2. -

Familial Multiple Coagulation Factor Deficiencies
Journal of Clinical Medicine Article Familial Multiple Coagulation Factor Deficiencies (FMCFDs) in a Large Cohort of Patients—A Single-Center Experience in Genetic Diagnosis Barbara Preisler 1,†, Behnaz Pezeshkpoor 1,† , Atanas Banchev 2 , Ronald Fischer 3, Barbara Zieger 4, Ute Scholz 5, Heiko Rühl 1, Bettina Kemkes-Matthes 6, Ursula Schmitt 7, Antje Redlich 8 , Sule Unal 9 , Hans-Jürgen Laws 10, Martin Olivieri 11 , Johannes Oldenburg 1 and Anna Pavlova 1,* 1 Institute of Experimental Hematology and Transfusion Medicine, University Clinic Bonn, 53127 Bonn, Germany; [email protected] (B.P.); [email protected] (B.P.); [email protected] (H.R.); [email protected] (J.O.) 2 Department of Paediatric Haematology and Oncology, University Hospital “Tzaritza Giovanna—ISUL”, 1527 Sofia, Bulgaria; [email protected] 3 Hemophilia Care Center, SRH Kurpfalzkrankenhaus Heidelberg, 69123 Heidelberg, Germany; ronald.fi[email protected] 4 Department of Pediatrics and Adolescent Medicine, University Medical Center–University of Freiburg, 79106 Freiburg, Germany; [email protected] 5 Center of Hemostasis, MVZ Labor Leipzig, 04289 Leipzig, Germany; [email protected] 6 Hemostasis Center, Justus Liebig University Giessen, 35392 Giessen, Germany; [email protected] 7 Center of Hemostasis Berlin, 10789 Berlin-Schöneberg, Germany; [email protected] 8 Pediatric Oncology Department, Otto von Guericke University Children’s Hospital Magdeburg, 39120 Magdeburg, Germany; [email protected] 9 Division of Pediatric Hematology Ankara, Hacettepe University, 06100 Ankara, Turkey; Citation: Preisler, B.; Pezeshkpoor, [email protected] B.; Banchev, A.; Fischer, R.; Zieger, B.; 10 Department of Pediatric Oncology, Hematology and Clinical Immunology, University of Duesseldorf, Scholz, U.; Rühl, H.; Kemkes-Matthes, 40225 Duesseldorf, Germany; [email protected] B.; Schmitt, U.; Redlich, A.; et al. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Regulation of Coagulation by the Fibrinolytic System: Expecting the Unexpected
Bleeding disorders Regulation of coagulation by the fibrinolytic system: expecting the unexpected K.A. Hajjar ABSTRACT Department of Cell and Recent investigations into fibrinolysis and coagulation have yielded exciting and unexpected findings. Developmental Biology, Of note, deficiencies of the major components of the classical fibrinolytic system, namely plasminogen, Department of Pediatrics tissue plasminogen activator, and urokinase, are now recognized to be rare causes of macrovascular Department of Medicine, thrombosis. At the same time, both plasminogen activator excess and fibrinolytic inhibitor deficiencies Weill Cornell Medical College, are associated with clinically significant bleeding, while elevated inhibitor levels, particularly thrombin New York, New York, USA activatable fibrinolysis inhibitor, appear to confer clinically significant risk for thrombosis. Receptor- mediated cell surface fibrinolysis adds a new dimension to the regulation of fibrin balance. Exaggerated expression of the annexin A2 complex, for example, is associated with hemorrhage in acute promyelo- Hematology Education: cytic leukemia, whereas autoantibodies directed against A2 correlate with thrombotic disease in the education program for the patients with antiphospholipid syndrome. The contributions of the urokinase receptor and a diverse annual congress of the European array of plasminogen receptors to fibrin homeostasis remain to be defined. Future studies are likely to Hematology Association reveal novel mechanisms that co-regulate coagulation and -

Alpha-Dystroglycan Plays Functional Roles in Platelet Aggregation and Thrombus Growth
Alpha-dystroglycan plays functional roles in platelet aggregation and thrombus growth by Reid Gallant A thesis submitted in conformity with the requirements For the degree of Master of Science Graduate Department of Laboratory Medicine and Pathobiology University of Toronto © Copyright by Reid Gallant 2017 i Alpha-dystroglycan Plays Functional Roles in Platelet Aggregation and Thrombus Growth Reid Gallant Master of Science Department of Laboratory Medicine and Pathobiology University of Toronto 2017 ABSTRACT Fibrinogen (Fg) and von Willebrand factor (VWF) have been considered essential for platelet adhesion and aggregation. However, platelet aggregation still occurs in mice lacking Fg and/or VWF but not β3 integrin, suggesting other, unidentified αIIbβ3 integrin ligand(s) mediate platelet aggregation. Through screening published platelet proteomics data, we identified a candidate, alpha-dystroglycan (α-DG). Using Western blot and flow cytometry, I found α-DG is expressed on platelets. Using aggregometry, I observed that antibodies against α-DG or its N- terminal Laminin-binding site, decreased platelet aggregation induced by various platelet agonists in both platelet-rich plasma and gel-filtered platelets. These antibodies also decreased platelet adhesion/aggregation in perfusion chambers independent of α-DG-Laminin interaction. Using laser injury intravital microscopy and carotid artery thrombosis models, we further found that these anti-α-DG antibodies decreased thrombus growth in vivo. Our results showed that α- DG may form an α-DG-fibronectin complex that binds to αIIbβ3 integrin, contributing to platelet adhesion/aggregation, and thrombosis growth. ii Acknowledgements ―It helps a man immensely to be a bit of a hero-worshipper, and the stories of the lives of the masters of medicine do much to stimulate our ambition and rouse our sympathies‖ – Sir William Osler I will always be grateful to my MSc supervisor, Dr. -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -

Factor V Leiden Thrombophilia
Factor V Leiden thrombophilia Description Factor V Leiden thrombophilia is an inherited disorder of blood clotting. Factor V Leiden is the name of a specific gene mutation that results in thrombophilia, which is an increased tendency to form abnormal blood clots that can block blood vessels. People with factor V Leiden thrombophilia have a higher than average risk of developing a type of blood clot called a deep venous thrombosis (DVT). DVTs occur most often in the legs, although they can also occur in other parts of the body, including the brain, eyes, liver, and kidneys. Factor V Leiden thrombophilia also increases the risk that clots will break away from their original site and travel through the bloodstream. These clots can lodge in the lungs, where they are known as pulmonary emboli. Although factor V Leiden thrombophilia increases the risk of blood clots, only about 10 percent of individuals with the factor V Leiden mutation ever develop abnormal clots. The factor V Leiden mutation is associated with a slightly increased risk of pregnancy loss (miscarriage). Women with this mutation are two to three times more likely to have multiple (recurrent) miscarriages or a pregnancy loss during the second or third trimester. Some research suggests that the factor V Leiden mutation may also increase the risk of other complications during pregnancy, including pregnancy-induced high blood pressure (preeclampsia), slow fetal growth, and early separation of the placenta from the uterine wall (placental abruption). However, the association between the factor V Leiden mutation and these complications has not been confirmed. Most women with factor V Leiden thrombophilia have normal pregnancies. -

Factor V Leiden Thrombophilia Jody Lynn Kujovich, MD
GENETEST REVIEW Genetics in Medicine Factor V Leiden thrombophilia Jody Lynn Kujovich, MD TABLE OF CONTENTS Pathogenic mechanisms and molecular basis.................................................2 Obesity ...........................................................................................................8 Prevalence..............................................................................................................2 Surgery...........................................................................................................8 Diagnosis................................................................................................................2 Thrombosis not convincingly associated with Factor V Leiden....................8 Clinical diagnosis..............................................................................................2 Arterial thrombosis...........................................................................................8 Testing................................................................................................................2 Myocardial infarction.......................................................................................8 Indications for testing......................................................................................3 Stroke .................................................................................................................8 Natural history and clinical manifestations......................................................3 Genotype-phenotype -

A First in Class Treatment for Thrombosis Prevention. a Phase I
Journal of Cardiology and Vascular Medicine Research Open Access A First in Class Treatment for Thrombosis Prevention. A Phase I study with CS1, a New Controlled Release Formulation of Sodium Valproate 1,2* 2 3 2 1,2 Niklas Bergh , Jan-Peter Idström , Henri Hansson , Jonas Faijerson-Säljö , Björn Dahlöf 1Department of Molecular and Clinical Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden 2 Cereno Scientific AB, Gothenburg, Sweden 3 Galenica AB, Malmö, Sweden *Corresponding author: Niklas Bergh, The Wallenberg Laboratory for Cardiovascular Research Sahlgrenska University Hospi- tal Bruna Stråket 16, 413 45 Göteborg, Tel: +46 31 3421000; E-Mail: [email protected] Received Date: June 11, 2019 Accepted Date: July 25, 2019 Published Date: July 27, 2019 Citation: Niklas Bergh (2019) A First in Class Treatment for Thrombosis Prevention? A Phase I Study With Cs1, a New Con- trolled Release Formulation of Sodium Valproate. J Cardio Vasc Med 5: 1-12. Abstract Several lines of evidence indicate that improving fibrinolysis by valproic acid may be a fruitful strategy for throm- bosis prevention. This study investigated the safety, pharmacokinetics, and effect on biomarkers for thrombosis of CS1, a new advanced controlled release formulation of sodium valproate designed to produce optimum valproic acid concen- trations during the early morning hours, when concentrations of plasminogen activator inhibitor (PAI)-1 and the risk of thrombotic events is highest. Healthy volunteers (n=17) aged 40-65 years were randomized to receive single doses of one of three formulations of CS1 (FI, FII, and FIII). The CS1 FII formulation showed the most favorable pharmacokinetics and was chosen for multiple dosing. -

Congenital Thrombophilia
Congenital thrombophilia The term congenital thrombophilia covers a range of Factor V Leiden and pregnancy conditions that are inherited by someone at birth. This means It is important that women with Factor V Leiden who are that their blood is sticker than normal, which increases the pregnant discuss this with their obstetrician as they have an risk of blood clots and thrombosis. increased risk of venous thrombosis during pregnancy. Some Factor V Leiden and Prothrombin 20210 are the most evidence suggests that they may also have a slightly higher common thrombophilias among people of European origin. risk of miscarriage and placental problems. Other congenital thrombophilias include Protein C Deficiency, Protein S Deficiency, and Antithrombin Deficiency. Prothrombin 20210 Prothrombin is one of the blood clotting factors. It circulates Factor V Leiden in the blood and when activated, is converted to thrombin. Factor V Leiden is by far the most common congenital Thrombin causes fibrinogen, another clotting factor, to thrombophilia. In the UK it is present in 1 in 20 individuals of convert to fibrin strands, which make up part of a clot. European origin. It is rare in people of Black or Asian origin. The condition known as Prothrombin 20210 is due to a Factor V Leiden is caused by a change in the gene for Factor mutation of the prothrombin gene. Individuals with the V, which helps the blood to clot. To stop a clot spreading a condition tend to have slightly stickier blood, due to higher natural blood thinner, known as Protein C, breaks down prothrombin levels. Factor V. -

Therapeutic Fibrinolysis How Efficacy and Safety Can Be Improved
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY VOL.68,NO.19,2016 ª 2016 PUBLISHED BY ELSEVIER ON BEHALF OF THE ISSN 0735-1097/$36.00 AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION http://dx.doi.org/10.1016/j.jacc.2016.07.780 THE PRESENT AND FUTURE REVIEW TOPIC OF THE WEEK Therapeutic Fibrinolysis How Efficacy and Safety Can Be Improved Victor Gurewich, MD ABSTRACT Therapeutic fibrinolysis has been dominated by the experience with tissue-type plasminogen activator (t-PA), which proved little better than streptokinase in acute myocardial infarction. In contrast, endogenous fibrinolysis, using one-thousandth of the t-PA concentration, is regularly lysing fibrin and induced Thrombolysis In Myocardial Infarction flow grade 3 patency in 15% of patients with acute myocardial infarction. This efficacy is due to the effects of t-PA and urokinase plasminogen activator (uPA). They are complementary in fibrinolysis so that in combination, their effect is synergistic. Lysis of intact fibrin is initiated by t-PA, and uPA activates the remaining plasminogens. Knockout of the uPA gene, but not the t-PA gene, inhibited fibrinolysis. In the clinic, a minibolus of t-PA followed by an infusion of uPA was administered to 101 patients with acute myocardial infarction; superior infarct artery patency, no reocclusions, and 1% mortality resulted. Endogenous fibrinolysis may provide a paradigm that is relevant for therapeutic fibrinolysis. (J Am Coll Cardiol 2016;68:2099–106) © 2016 Published by Elsevier on behalf of the American College of Cardiology Foundation. n occlusive intravascular thrombus triggers fibrinolysis, as shown by it frequently not being A the cardiovascular diseases that are the lead- identified specifically in publications on clinical ing causes of death and disability worldwide.